Human Physiology pt 1
1/202
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
203 Terms
What are the 4 general categories of specialized cells? Give a general description for each
epithelial cells
found at surface of body or hollow organ
specialized to secrete or absorb ions/organic molecules
connective tissue cells
form extracellular elements
connect, anchor, and support body structures
neurons
highly specialized cells for rapid communication
initiate, integrate, and conduct electrical signals
muscle cells
electrically excitable
key feature is that they can change their shape based on actin and myosin filaments that generate force and movement
What are tissues, organs, and organ systems?
tissues = collections of cells that carry out related functions
organs = collections of multiple tissue types that carry out related functions
organ systems = collections of multiple organs that work together
What are the 10 physiological organ systems in the body?
integumentary system
skin
one of 2 barriers between you and outside world
forms a protective boundary that separates the body’s internal environment and external environment
digestive system
the other barrier between you and outside world; tube that takes outside world through the body essentially
takes up nutrients and water and eliminates wastes
reproductive system
produces eggs or sperm
immune system
provides defense against foreign invaders
endocrine system
coordinates body function through synthesis and release of regulatory molecules
one of two communication systems in the body
nervous system
the other communication system in body
coordinates body function through electrical signals and release of regulatory molecules
circulatory system
transports material between all parts of the body
respiratory system
exchanges O and CO2
musculoskeletal system
provides support and is responsible for movement
urinary system
maintains water and solutes in internal environment
waste removal
Explain how the outside world affects the cell turnover rate in the integumentary and digestive systems?
integumentary and digestive systems are the 2 main protective barriers between internal and external environments
their cells are so abused by the outside world that they need to keep turning over the cells
they keep shedding and creating new cells at a relatively fast rate because of their contact with the outside world
Explain cellular differentiation
cellular differentiation is a process that happens during development
a single cell proliferates and those cells become specialized into the 4 functional groups
What is one important way in which cells regulate their own activity?
By maintaining differences in fluid composition across the cell membrane
What is intracellular fluid and what is extracellular fluid?
intracellular fluid = fluid inside cells
distinct from ECF
extracellular fluid = ECF
made of plasma and interstitial fluid
interstitial fluid = fluid directly in contact with outside of cells
plasma = fluid in blood; flowing around in cardiovascular system
serves as buffer zone bw cells and outside environment
What is the interstitium?
The space containing interstitial fluid
What percent of body weight is water? What percentages are intracellular, plasma, and interstitial volumes?
60% of TOTAL body weight is water
2/3 of body FLUID is intracellular fluid
of the remaining 1/3:
20-25% is plasma
and remaining 75-80% is interstitial fluid
another way to think about it is this:
67% of ALL body FLUID is intracellular
26% of ALL body FLUID is interstitial
7% of ALL body FLUID is plasma
How does the ECF serve as a buffer zone bw cells? How is it for red and white blood cells?
essentially all cells except for RBC and WBC are surrounded by interstitial fluid and the plasma from their nearest blood capillary also does buffering/exchange of materials
however since RBC and WBC are already in the blood, they aren’t surrounded in interstitial fluid they only have the plasma
when the ECF composition varies outside its normal range of values, the body has compensatory mechanisms that bring it back to the normal state
that is how the intracellular state is controlled/maintained
Compare the composition of intracellular fluid and extracellular fluid
ICF = higher in protein and potassium (K+)
ECF = lower in protein but higher in Na+
Compare the compositions of interstitial fluid and plasma
both are quite similar but plasma has a much higher concentration of protein
think bc it has RBC, WBC, and cellular fragments
Why is there a greater difference in composition between ECF and ICF, compared to the difference between interstitial fluid and plasma?
there is the cell membrane between the ECF and ICF keeping them separate and deciding what passes between them
there is no such barrier between the interstitial fluid and plasma (blood capillaries are very leaky so they freely allow fluid to pass from one compartment to the other)
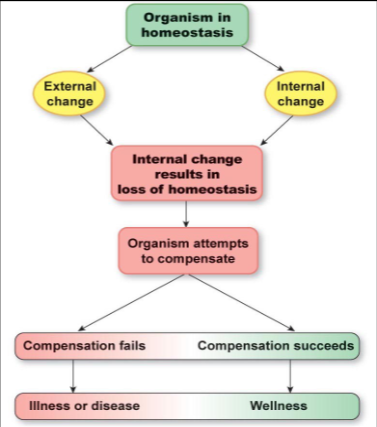
What is homeostasis? What is the term for when it is normal and what is the term for when it is not?
homeostasis = relatively stable condition of internal environment that results from regulatory system actions
physiology = when homeostasis is normal
pathophysiology = when homeostasis is not normal
What is dynamic constancy? Give an example
levels of a certain physiological variable change over short periods of time (dramatically) but over a long period of time they remain relatively constant
ex)
blood sugar remains relatively constant throughout day but then spikes after a meal but then goes back to set point
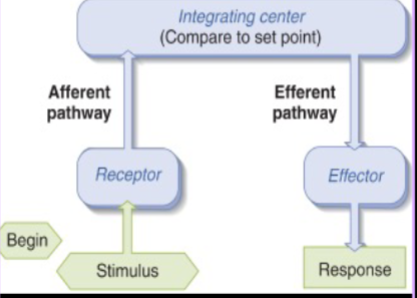
What is a reflex?
a specific INVOLUNTARY, unpremeditated, unlearned, built-in response to a particular stimulus
What is a reflex arc? What are the 7 parts of it?
stimulus = DETECTABLE change in internal/external environment
a change in a physiological parameter
receptor = detects stimulus
afferent pathway = takes signal from receptor to integrating center
integrating center = compares signal to set point and decides what to do next
can receive signals from many receptors at a time
efferent pathway = takes signal from integrating center to effector
effector = muscle or gland that carries out response
response = brings back environment to set point (in negative reflex arc at least)
REMEMBER: A comes before E in alphabet → afferent BEFORE efferent
note actual body parts/organs/glands/etc are bolded; others are more so processes or pathways, etc
What is a negative feedback arc and what is a positive feedback arc?
negative arc = response acts to counter the stimulus and bring it back to set point → HOMEOSTATIC
positive arc = response reinforces stimulus and brings further away from set point → NOT HOMEOSTATIC
What is an example of a positive feedback arc/loop?
childbirth
basically, when a woman is in labor, the baby pushes on cervical stretch receptors which causes a signal to go to brain and indicate that labor has started, to which the brain produces more oxytocin. the oxytocin travels through blood down to uterine lining and causes more contractions, which leads to baby pushing against cervical stretch receptors even more (reinforcement of stimulus)
in terms of a reflex arc:
stimulus: uterus drops and baby’s head pushes on cervical stretch receptors
receptor: the cervical stretch receptors
afferent pathway takes signal to brain
integrating center: hypothalamus → sends efferent pathway
efferent pathway → oxytocin, which gets circulated throughout body by vascular system and reaches the effector
effector organ = uterine lining
response = more contractions and pushing
What are 2 ways in which cells communicate short distance and 2 ways in which they communicate long distance?
if target is close:
paracrine = signal diffuses to nearby cells
autocrine = cell sends signal to itself but externally
if target is distant:
endocrine = signal travels by blood circulation
neuronal = signal transmitted by nervous system
What are two advantages of intracellular signaling pathways?
can amplify a signal → make small signal into big response in cell
can allow for tight regulation of pathway → cells can integrate multiple signals
What are 4 potential responses/effects a signaling pathway can cause in a cell?
immediate change in metabolism in the cell
ex) increased glycogen breakdown when a liver cell detects epinephrine
immediate change in electrical charge across plasma membrane
source of action potentials
immediate change in regulation of cytoskeletal proteins
affects cellular motility
change in transcription → takes more time
What is signal transduction?
any process by which a cell converts one kind of signal to another
can take millisecond to a few seconds
signaling cascade → signal is amplified bc of increasing number of enzymes and second messengers, etc, with every step of the chain
can also lead to diversification of outcomes within cell bc of multiple second messengers
What is a second messenger? Give 2 examples
a molecule (that is not a protein or peptide) that relays signals to target molecules in the cytosol and/or nucleus
often times, serves to amplify signal
ex) cyclic nucleotides
cyclic AMP → derived from ATP
cyclic GMP → derived from GTP
ex) Ca2+
What are the 2 types of extracellular signal molecules? What are the examples we learned for each subcategory?
with intracellular receptors
small/hydrophobic enough to cross plasma membrane by self
examples:
Nitric oxide (NO) → gasses can also be signaling molecules
Cortisol → steroid molecules have intracellular receptors bc they are hydrophobic (derived from cholesterol)
with extracellular receptors
too big/hydrophilic to cross membrane
3 types of hydrophilic cell signaling receptors:
G-protein linked receptors
ion-channel linked receptors
enzyme linked receptors
Explain how nitric oxide (NO) works as a signaling molecule?
a nerve innervating an endothelial cell of the lumen of a blood vessel has a signal that causes it to release acetylcholine
the acetylcholine binds to the receptor of an endothelial cell of the lumen of a blood vessel, which opens gate for Ca2+ to enter cell
increased Ca2+ levels in cell, causes activation of NO synthase, which is the enzyme that breaks down arginine (amino acid) into NO
NO is a nonpolar gas molecule, which diffuses rapidly and acts as a paracrine signal to nearby smooth muscle cells of the blood vessel
NO enters smooth muscle cells, and activates the guanylyl cyclase, which is the enzyme that converts GTP to cGMP (cyclic GMP)
increased cGMP levels leads to dilation of smooth muscle cells by perturbing the cytoskeletal machinery→ causes blood vessel to dilate
only happens in arteries and veins, not in capillaries bc capillaries have no smooth muscle cells
Explain how Viagra works
Phosphodiesterase (PDE) are the enzymes that break down the cGMP and allow the smooth muscle cells to contract again, so pharmaceutical companies wanted to create a drug that would inhibit PDE so the smooth muscle cells could stay dilated for longer
another way this is phrased is that PDE is inhibited so NO signal is prolonged, but Viagra doesn’t actually affect the NO signal pathway by any way it just inhibits PDE so the cGMP isn’t broken down for a longer time
original plan was to do this as a way to counteract hypertension → PDE inhibited would allow arteries to remain dilated and lower BP
Pfizer made Viagra for this purpose, but found there are multiple types of PDE in the body, and the one that Viagra inhibited is found only in the male reproductive organ
Viagra inhibits that specific PDE and counteracts erectile dysfunction by allowing smooth muscle to remain dilated for longer
How do steroid hormones work as signaling molecules? Give 4 examples
all steroid hormones are derived from cholesterol and have the nonpolar ring structures allowing them to pass through plasma membrane easily
the receptors for many of these steroid hormones are transcription factors
process:
steroid hormones pass through plasma membrane and bind to transcription factor receptors
the steroid receptor complex then moves into nucleus and binds to regulatory region of the target gene and either activates or inhibits transcription of that gene
ex) cortisol, estradiol, testosterone, and thyroid hormones
Where are hydrophilic cell signaling receptors found in a cell? What are the 3 types of hydrophilic cell signaling receptors?
found on cell-surface (extracellular side of plasma membrane)
3 types
G-protein linked receptors
Ion-channel linked receptors
Enzyme linked receptors
What are G-protein linked receptors?
largest family of cell-surface receptors
many types of G-protein receptors → specific to ligand
all have trimeric G-proteins with y, a, B subunits and GDP attached to the a subunit during inactive state
different effector proteins as well
What is the general process for all G-protein linked receptors?
hydrophilic ligand binds to extracellular side of receptor and causes conformational change to receptor on the cytoplasmic side
this change causes receptor to bind with G-protein, which causes GDP to be exchanged with GTP which activates the G-protein
once activated, the G-protein splits into By and a subunits that can both interact with target proteins in plasma membrane, but we are usually primarily interested in what the a subunit is doing → go and activate effector proteins
upon activating the effector protein, the a subunit replaces GTP with GDP and that shuts down the protein → the trimeric G-protein reunite
What effector protein do all Gs coupled protein receptors interact with?
adenylate cyclase
Explain the Gs protein linked receptor pathway
signal stimulus binds to the extracellular side of receptor and activates it
the activated receptor then activates the trimeric Gs protein
the a subunit of the Gs protein goes to adenylyl cyclase and activates it, which deactivates the Gs
when adenylyl cyclase is activated, it catalyzes formation of cyclic AMP (cAMP)
cAMP is a 2nd messenger, which goes and activates Protein Kinase A (PKA)
Phosphodiesterase quickly degrades cAMP
PKA moves into the nucleus and phosphorylates specific gene regulatory proteins
PKA can also phosphorylate proteins in cytosol
when phosphorylated they go and stimulate the transcription of a whole set of target genes
Explain GQ protein linked receptor pathway
ligand binds to extracellular end of receptor which causes intracellular part to bind to GQ trimeric protein and activate it, causing a subunit to go and activate Phospholipase C (PLC)
the activated PLC cleaves PIP2 into two different second messengers: IP3 and DAG
IP3 binds to a ligand gated ion channel on the smooth ER, which opens a gate to allow Ca2+ to leave smooth ER
DAG goes to Protein Kinase C (PKC) and removes the inhibitory protein attached to it
DAG is hydrophobic so it remains embedded in the intracellular side of the membrane
the Ca2+ from IP3 subpathway also goes to PKC and helps it go do other stuff
basically DAG and IP3 together maximize what PKC does
What does the Gi protein linked receptor pathway do?
it inhibits adenylyl cyclase, in turn inhibiting production of cAMP, inhibiting activation of PKA, and inhibiting activation of gene regulatory proteins
What does Gt protein linked receptor pathway do?
stimulates cGMP phosphodiesterase production
What degrades cAMP? Why is fast cAMP degradation necessary? What happens if cAMP is not degraded?
Phosphodiesterase (PDE) degrades cAMP
it is important to shut down cAMP quickly to maintain sensitivity of the cell to the extracellular signal molecules
Give an example of a natural phosphodiesterase inhibitor and explain how it works
Caffeine is a natural inhibitor of PDE that breaks down cAMP
it allows cAMP to continue staying in the cell, causing PKA to continue being activated
in neuronal cells, the PKA continuing being activated leads to improved synaptic transmission and increased neuronal activity → which is why caffeine is a stimulant
What are the two ways in which G protein pathways are regulated? (at least the ones we studied)
the G protein a subunit is self-regulating in the sense that it turns off (replaces GTP with GDP) after activating effector protein
Phosphodiesterase breaks down the cyclic nucleotides (cAMP or cGMP) to preserve sensitivity of cell receptor to signal
Explain how ion channel-linked receptors work
a ligand binds to ion channel protein gate on receptor on extracellular side
this causes a conformational change in the shape of the gate, making it go from closed to open
ions (Na+, K+, Ca2+, Cl-, etc) can be let out or in depending on concentration gradient
How do ion channel-linked receptors convert signals?
they convert a chemical signal (in the form of a hydrophilic ligand) into an electrical signal because ions bring a charge with them whether they are leaving or entering the cell, and therefore cause a change in voltage across the plasma membrane of that cell
this is especially important in the nervous system
How do enzyme linked receptors work? Give the name of an example
ligand binds to receptor, causes conformational change in the enzyme, triggering activity
ex) receptor tyrosine kinases (RTK)
What are receptor tyrosine kinases (RTKs)? Give a specific example
basically RTKs cause assembly of an intracellular signaling complex on the intracellular tail of the receptor (from trans-autophosphorylation after dimerization of receptors)
specific example we studied was the Epidermal Growth Factor receptor pathway → note even tho pathway name is EGF the main enzyme is the RTK
Explain how the epidermal growth factor receptor pathway works
1 epidermal growth factor (EGF) binds to extracellular end of 1 epidermal growth factor receptor (EGFR)
this causes dimerization of the EGFR
basically another EGF must bind to another EGFR and that causes two of them to bind to each other (dimerize)
this dimerization causes enzymatic activity that causes trans-autophosphorylation basically all the tyrosine residues on the EGFRs get autophosphorylated
the phosphorylated tyrosine residues activate downstream scaffolding cytoplasmic proteins
the tyrosine on the EGFR are called receptor tyrosine kinase (RTK)
scaffolding proteins are aka adaptor proteins
these proteins build a bridge between the (RTK) and the Ras protein, activating it
unactivated, the Ras protein has a GDP but upon activation it gets a GTP (Ras GDP → Ras GTP)
the Ras protein is bound to plasma membrane on cytoplasmic side by a lipid tail
when activated, Ras protein activates a phosphorylation cascade
phosphorylates MAP-kinase-kinase-kinase. which phosphorylates MAP-kinase-kinase, which phosphorylates MAP-kinase, which phosphorylates several other target proteins
these other target proteins can affect cell metabolic activities or activate transcription factors etc.
eventually causes cell growth in case of EGF
How similar are all growth factor receptor pathways?
they have different signaling ligands and different ligand-specific receptors, but the main process is the same
the pathways all activate the Ras-GTP
once Ras-GTP is activated it will cause proliferation of the cell
What is the connection between the Ras gene and cancer?
~30% of human cancers involve mutations of the Ras gene that cause it to be constitutively activated
basically a mutation of the gene causes Ras proteins to always be bound to GTP (turned on) therefore constantly stimulating cell proliferation
uncontrolled cell proliferation is cancer
Ras protein is a monomeric GTP protein which dephosphorylates the GTP to GDP and turns itself off under normal conditions
Why do drugs have side effects?
signaling pathways are highly interconnected
a drug is made to affect one pathway but may have unintended impacts on the effects of other pathways too which causes side effects
What is the endocrine system? Also, give four examples of organs you don’t expect to be a part of the endocrine system but are
one of the two major communication systems in the body
made of glands and hormone secreting cells
includes glands exclusive to endocrine system but also other organs (such as heart, kidneys, liver, and stomach) that you don’t expect to be part of the endocrine system but they are bc they produce hormones
What are main differences between the two major communication systems of the body?
nervous system is very fast and directly sends signal to targeted spot it wants to, however, endocrine system is much slower and sends signal throughout body through the vascular system but only cells with correct receptors elicit a response
this is also why endocrine system signals are longer lasting than nervous system signals
What is the difference between a neurohormone and a neurotransmitter?
neurotransmitter = neuronal chemical signal released at the synapse by a neuron
neurohormone = neuronal chemical signal released directly into bloodstream by a neuron/neurosecretory cell
Briefly go over what it means if a single endocrine gland is secreting multiple hormones and give an example
In general, single cell types in glands secrete only one hormone. This means, multiple hormone secreting glands have different types of endocrine cells producing and secreting different hormones.
ex) pancreas
Explain pancreas as a multiple hormone secreting endocrine gland. What are the 3 main hormones it produces and how does its structure allow that?
Hormones:
insulin = lowers blood glucose levels
glucagon = increases blood glucose levels
somatostatin = inhibits secretion of pancreatic hormones
Islets of Langerhans = endocrine areas of the pancreas in which there are alpha, beta, and delta cells
alpha → glucagon
beta → insulin
delta → somatostatin
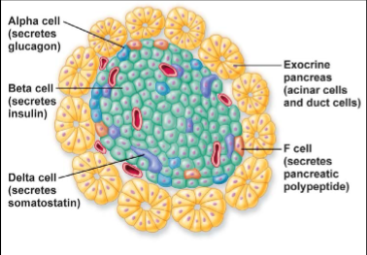
What is the difference between exocrine and endocrine glands? Give example with pancreas
exocrine = gland that secretes into a duct from where secretion either leads out to lumen of organ or from where they exit the body
ex) part of pancreas (called acinar cells) producing and secreting digestive enzymes → goes from pancreas to intestines
endocrine = gland that has no ducts and secretes into interstitial fluid which diffuses into bloodstream
ex) part of pancreas (islets of Langerhans) producing and secreting insulin, glucagon, and somatostatin
What are the 3 major chemical classes of endocrine hormones? Give brief description of each
amine hormones
derived from the amino acid tyrosine
made by thyroid gland, adrenal medulla, and hypothalamus
peptides and proteins
largest class of endocrine hormones → makes up most endocrine hormones
produced in tissues all over the body
steroids
lipids with ring-like structures
primarily produced by the adrenal cortex, gonads, and placenta during pregnancy
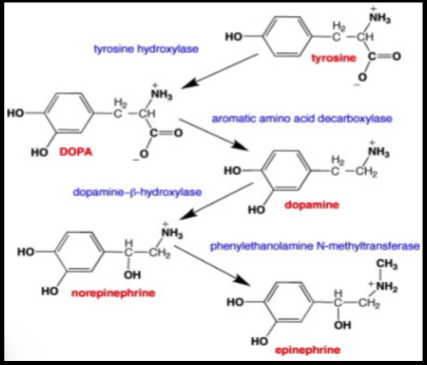
What are 4 examples of amine hormones? How are they produced?
4 examples:
1. thyroid hormones (T3 and T4) → produced in thyroid gland
catecholamines → produced in adrenal medulla
2. epinephrine (aka adrenaline)
3. norepinephrine (aka noradrenaline)
4. dopamine → produced in hypothalamus
they are produced by thyroid gland, adrenal medulla, and hypothalamus
they are all derived from tyrosine, which is an amino acid
which hormone that tyrosine gets converted to in that secretory cell, depends on the enzymes present within that cell
What are the thyroid hormones?
The thyroid hormones are T3 and T4 and they are amine hormones derived from tyrosine and iodinated
Why is iodine so important in our diets?
iodine is essential to make the T3 and T4 (thyroid hormones) functional
thyroid hormones are essential in metabolic processes, and if they are not iodinated properly, they will not work
if T3 and T4 are messed up, then person is lethargic and does not grow properly
if the body has insufficient iodine for extended time, it can form a goiter which is proliferation of thyroid cells in an attempt to make more T3 and T4
which is why salt is iodized to make sure ppl are getting enough iodine
What are catecholamines?
amine hormones with the catechol groups
dopamines, epinephrine, norepinephrine

What does iodine do to thyroid hormones that makes them different from catecholamines?
the iodination allows thyroid hormones to pass through plasma membrane more easily → thus they can have intracellular receptors
however, catecholamines cannot pass easily through plasma membrane so they need extracellular receptors
What are peptides and proteins? Gvie 2 examples
the largest class of endocrine hormones
made not just by exclusively endocrine system hormones
examples
insulin
glucagon
they have extracellular receptors because they are hydrophilic
What are insulin and glucagon? How do those pathways work?
insulin and glucagon are produced and secreted by the beta and alpha cells of the pancreas, respectively
the beta and alpha cells act as both receptor and integrating center for blood glucose levels
they monitor blood glucose levels
if too high (above 110) → release insulin → goes to liver or muscle cells to get them to take up glucose and convert to glycogen
if too low → release glucagon → goes to liver to release stored glucose
in this way, insulin and glucagon act as efferent signals
How are peptide hormones made? Give the example of insulin
process:
preprohormones are large and inactive polypeptide chains encoded by the mRNA
contains signal sequence, one or more copies of the hormone, and additional peptide fragments
the signal sequence takes preprohormone to the rough ER, where the signal sequence is cleaved off, making it an inactive prohormone
the prohormone travels to Golgi apparatus, where it is packaged into secretory vesicles
within the vesicles, prohormone is cleaved into the final hormone and the inactive parts
Example of insulin:
preproinsulin goes to rough ER, where the signal sequence is cleaved off, making it proinsulin
the proinsulin goes to Golgi apparatus where it is packaged into vesicles
the enzymes cut the proinsulin into insulin and C-peptides
the vesicles store the insulin and C-peptides until ready to be released via exocytosis
How is insulin measured in body, usually by diabetic patients?
C-peptide levels are measured because insulin as pretty short half-life, but C-peptide does not → it can be used as a marker of insulin secretion
What are steroid hormones? Give 4 examples with a brief description of each
steroid hormones are lipid hormones derived from cholesterol
examples
cortisol
aka stress hormone
glucocorticoid
secreted from adrenal cortex
regulates metabolism during stress
aldosterone
mineralocorticoid
promotes Na+and H2O reabsorption
testosterone - sex hormone
estradiol - sex hormone
How long before release are steroid hormones synthesized?
steroid hormones are released as soon as they are synthesized because they are lipids → they can pass through the plasma bilayer so there’s no way to hold them back and wait till release
How are steroid hormones synthesized?
an anterior pituitary gland hormone binds to cell surface receptor
intercellular end of receptor activates trimeric Gs protein
Gs protein a subunit goes and activates adenylyl cyclase
activated adenylyl cyclase produces cAMP, which activates PKA
activated PKA phosphorylates many proteins including cholesterol esterase
activated cholesterol esterase releases free cholesterol from liquid droplet (from LDL) that exists in the cell
the free cholesterol is transported to the mitochondria where it is processed in many steps and shuttled between the smooth ER and the mitochondria
once formed, the steroid hormone diffuses out of the parent cell and travels to target cell (sometimes with help of carrier protein) and diffuses into target cell
How do carrier proteins help certain hormones? Give some examples
they help transport steroid hormones and thyroid hormones through the blood to get to their target cell because they are both hydrophobic so they don’t like being in the blood
ex)
corticosteroid-binding globulin → helps cortisol
albumin → general protein
Explain the parts of the adrenal gland and what hormones they produce
2 adrenal glands (one on top of each kidney but doesn’t really impact kidney filtration function)
capillary beds go all the way in to ensure hormones can be transported easily
2 main parts:
adrenal medulla
inside part
¼ of mass
secretes catecholamines (epinephrine and norepinephrine)
secretes 4 times more epinephrine than norepinephrine
involved in fight or flight response
adrenal cortex
outside of medulla
¾ of mass
has 3 layers from closest to medulla to furthest out:
Zona reticularis → sex hormones
Zona fasciculata → glucocorticoids
Zona glomerulosa → aldosterone
stupid memorization trick: meri raat faltu gayi
What are the two factors upon which a hormone’s plasma concentration depends?
rate of secretion by endocrine gland
rate of removal (clearance)
happens either by excretion or by metabolic transformation
What are the 3 possible ways that a hormone can be removed (cleared)?
metabolized or excreted by kidneys and liver
metabolized by target cell by way of endocytosis of hormone-receptor complex
enzymes in blood
What are the 4 ways in which hormones can interact with one another in a cell?
Permissiveness
hormone B can only exert its full effect when hormone A is present
one possible mechanism is that this happens because hormone A upregulates the expression of receptors for hormone B
ex) epinephrine can release large amounts of fatty acids from adipose tissue but only in the presence of thyroid hormones bc thyroid hormones stimulate the synthesis of B-adrenergic receptors for epinephrine in adipose tissue
Additive
when hormones are combined, their combined effects are added together (measuring same factor ex. blood glucose)
Synergistic
when hormones are combined, their combined physiological effect is far greater than additive
Antagonistic
opposite effect
What are the 3 types of inputs that control hormone secretion in endocrine cells? Explain all 3 in the example of insulin secretion from pancreatic B cells.
changes in plasma concentrations of ions or organic nutrients
ex) increase in blood glucose concentration can trigger release of insulin
neurotransmitters released from neurons ending on the endocrine cell
ex) stretch receptor in digestive tract, send afferent signal to CNS, which sends efferent signal to pancreas to release insulin
another hormone acting on the endocrine cell
ex) blood glucose also releases Glucagon-like peptide-1 (GLP-1) from endocrine cells in small intestine
GLP-1 is another hormone that promotes insulin secretion from pancreas
often times cells are receiving simultaneous opposing inputs and the rate of hormone secretion reflects the integration of all of these inputs
ex) insulin secretion from pancreatic B cells is regulated by all 3
What are the 2 main categories of disease in endocrine systems? What are the 4 total endocrine disease types within those 2 categories? Give examples
disease from abnormal hormonal secretion
hyposecretion = too little hormone
hypersecretion = too much hormone
disease from abnormal responsiveness of target cells
hyporesponsiveness = reduced responsiveness
hyperresponsiveness = increased responsiveness
Example:
Type 1 diabetes mellitus → hyposecretion of insulin
patient has reduced number of active pancreatic B cells so not enough insulin is produced
Type 2 diabetes mellitus → hyporesponsiveness
patient has reduced cellular sensitivity to insulin, so not enough responsiveness
What is the most important control area for homeostatic regulation of the internal environment?
the hypothalamus
What is the pituitary gland?
two glands with different embryological origins that fused during development
not considered part of the brain → sits in protected pocket of bone, connected to the hypothalamus (which is part of the brain) by a thin stalk called the infundibulum or pituitary stalk
together the hypothalamus and pituitary gland regulate essentially every part of the body
What are the 2 parts of the pituitary gland? Describe both of them
anterior pituitary gland
anterior = closer to front of body
the anterior pituitary is a true endocrine gland of epithelial origin
posterior pituitary gland
not a true gland but rather just an extension of the hypothalamus → no endocrine cell bodies found here
the hypothalamus sends its axons down
secretes neurohormones synthesized in the hypothalamus
oxytocin → milk ejection and childbirth
vasopressin → water regulation
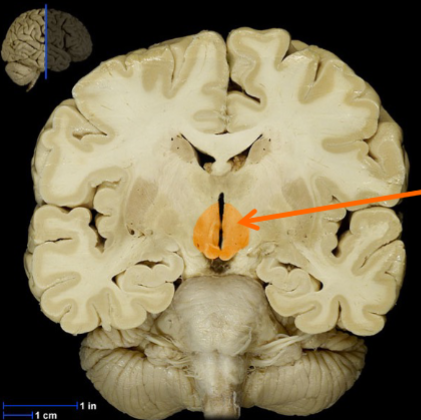
Label all of the parts of this diagram
hypothalamus
supraoptic nuclei
paraventricular nuclei
infundibulum
posterior pituitary
anterior pituitary
sphenoid bone
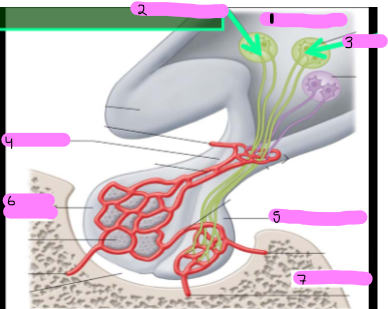
What do nuclei refer to in the central nervous system? What are the two nuclei in the posterior pituitary and what do they do?
nuclei = cluster of nerve cell bodies in the central nervous system
the two nuclei in the posterior pituitary are neurosecretory endocrine cells - even tho they look like neurons
they both extend axons to posterior pituitary and synthesize the neurohormones: Vasopressin and Oxytocin
end of axons terminate in interstitial fluid - not into a synapse and that is why they are not neurons
Supraoptic nuclei → just above the optic nerve
Paraventricular nuclei
Describe the two posterior pituitary neurohormones
Oxytocin and vasopressin
both are small peptide neurohormones made of 9 amino acids each
Oxytocin:
involved in 2 reflexes:
ejection of milk in response to stimulation of nipples during nursing
stimulation of contractions of uterine smooth muscle cells in response to stretch receptors being activated in the cervix during birth
Vasopressin
aka antidiuretic hormone (ADH)
acts on the kidneys to regulate water balance in body
What is the process of neurohormones being secreted from posterior pituitary gland?
neurohormone (oxytocin or vasopressin) is made and packaged in cell body of neuron (supraoptic nuclei or paraventricular nuclei)
vesicles transport it down axons
in the infundibulum
vesicles containing the neurohormone are stored in axon terminals were they wait for a release signal
axon terminals are in the posterior pituitary gland itself
the signal - in the form of an action potential - passes down neuron and releases neurohormones into blood
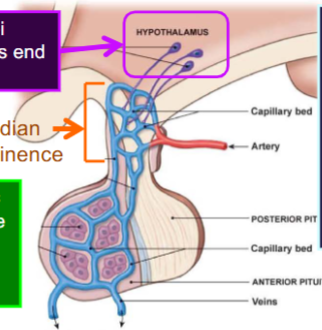
What is the structure of the anterior pituitary gland? How do neurohormones get from hypothalamus to anterior pituitary gland?
several hypothalamic nuclei send axons from hypothalamus to median eminence → these nuclei are what primarily regulate the anterior pituitary
median eminence = where hypothalamic axon terminals end
those neurosecretory cells release neurohormones into interstitial fluid then to capillary bed in the median eminence
from the capillary bed, portal vessels take neurohormones to all over body, but primarily they take them from median eminence to anterior pituitary, where they leak into interstitial fluid again and get to endocrine cells in the anterior pituitary
What regulates the anterior pituitary gland endocrine cells?
Hypophysiotropic hormones
aka hypothalamic inhibiting/releasing hormones
some non-hypothalamic hormones also influence the anterior pituitary gland - involved in some feedback inhibition
What is the structure of the anterior pituitary? What is the name of the circulatory region through which neurohormones from the hypothalamus reach the anterior pituitary gland?
hypothalamic neurons/neurosecretory cells (bc they secrete into capillaries not synapses) synthesize hypophysiotropic hormones in cell bodies and extend axons down to median eminence
here the neurosecretory cells release their neurohormones into capillaries of the hypothalamic-hypophyseal portal system
portal vessels carry hormones directly to anterior pituitary endocrine cells
from their the endocrine cells release their hormones to second set of capillaries that distribute them to rest of body
What is the 3 hormone sequence through which hypophysiotropic hormones act?
Stimulus
Hypothalamus → Increase in Hormone 1 secretion
increase in Hormone 1 plasma concentration in hypothalamo-pituitary portal vessels (aka hypothalamic-hypophyseal portal system)
Anterior pituitary → increase in Hormone 2 secretion
Increase in Hormone 2 plasma concentration
Third endocrine gland → Increase in Hormone 3 secretion
Increase in Hormone 3 plasma concentration
Target cells of Hormone 3 → response to Hormone 3
What is the 3 hormone sequence for producing insulin-like growth factor in the liver?
Hypothalamus releases GHRH into portal vessels
GHRH stimulates anterior pituitary to produce GH
GH goes through vascular system to reach the liver, which then produces IGFs (insulin-like growth factors)
IGFs go to bone and soft tissue to stimulate growth
What are the 6 hypophysiotropic hormones and what tropic hormones do they regulate?
FSH and LH
1. GnRH = gonadotropin releasing hormone
stimulates release of FSH and LH (gonadotropins)
ACTH
2. CRH = corticotropin releasing hormone
stimulates release of ACTH (corticotropin)
TSH
3. TRH = thyrotropin-releasing hormone
stimulates release of TSH (thyrotropin)
Prolactin
4. DA = dopamine
inhibits release of Prolactin; prolactin is produced only in absence of dopamine, there is no stimulatory hormone
Growth Hormone - under dual control
5. GHRH = Growth Hormone Releasing Hormone
stimulates release of GH
6. SS = Somatostatin
inhibits release of GW
What are the 6 peptide hormones the anterior pituitary secretes? Give a brief description of them
Tropic hormones = hormones that ONLY stimulate other endocrine glands
FSH = Follicle-Stimulating Hormone
gonadotropic
LH = Luteinizing Hormone
gonadotropic
ACTH = Adrenocorticotropic Hormone
tells adrenal cortex to make and secrete cortisol
TSH = Thyroid Stimulating Hormone
tells thyroid gland to make and secrete T3 and T4
hormones that stimulate another body part DIRECTLY
Prolactin
milk producing hormones goes to mammary glands
i → ignore; just to help with memorization
GH = Growth Hormone
tells liver to make and secrete the growth promoting hormone (which is an insulin-like growth factor)
How is ACTH synthesized in the anterior pituitary from POMC protein?
POMC = pro-opiomelanocortin
precursor protein to ACTH, synthesized in Golgi apparatus of endocrine cells in the anterior pituitary gland
in post-translational processing, POMC gets cut into:
ACTH
y-lipotropin (alpha lipotropin)
B-endorphin (beta endorphin) → endogenous opioid that helps block pain
after acting as a hormone, ACTH can get further processed in non-pituitary tissues:
a-MSH
stimulates melanin synthesis, immune response, and decreases food ingestion/intake
Where are hypophysiotropic hormones produced and where are tropic hormones produced?
hypophysiotropic → produced in hypothalamus, pass through median eminence, and pass via the portal vessels to get to the anterior pituitary
tropic → produced in anterior pituitary
Explain how negative feedback is used to control the hypothalamo-pituitary system and the two loops through which this can be done
one hormone out of the 3-hormone pathway will go back and switch off the pathway at some point
can be done in two ways:
short-loop: when hormone goes to switch off the one before
ex) pituitary hormone feeds back to switch off hypothalamic hormone secretion
ex) hormone 3 feeds back to pituitary gland to switch off hormone secretion
long-loop: when last hormone goes to switch off hypothalamus
ex) hormone 3 goes to pituitary to switch off hormone 2 production and to hypothalamus to switch off pathway
Explain the milk ejection reflex in terms of prolactin and oxytocin
prolactin
anterior pituitary hormone
stimulates milk PRODUCTION
oxytocin
posterior pituitary hormone
involved in control of milk EJECTION
What is cortisol?
steroid hormone secreted from adrenal cortex
stress hormone
plays direct role in mediation of chronic stress
What is stress as used in biology?
any change in the environment that changes or threatens to change an existing optimal state
most stresses activate homeostatic reactions at the molecular, cellular, or systemic level
What is the control pathway for cortisol secretion?
hypothalamic-pituitary-adrenal (HPA) pathway
1) corticotropin-releasing hormone (CRH) is secreted by the hypothalamus into the hypothalamic=hypophyseal portal system
this secretion is stimulated by circadian rhythm or by stress
2) CRH stimulates release of adrenocorticotropic hormone (ACTH) from anterior pituitary gland
ACTH aka corticotropin
from anterior pituitary it passes into interstitial fluid and then into the capillaries/vascular system all through simple diffusion
3) ACTH goes to adrenal cortex (zona fasciculata) to promote synthesis and release of cortisol
4) cortisol acts as negative feedback signal and inhibits ACTH and CRH secretion
cortisol can inhibit ACTH and CRH
ACTH can inhibit CRH and stimulate cortisol
What is the most important metabolic effect of cortisol in non-stress conditions?
Protection against hypoglycemia
when blood glucose drops, pancreas secretes glucagon
glucagon promotes gluconeogenesis and glycogen breakdown
in the absence of cortisol, glucagon cannot respond adequately to a hypoglycemic challenge
cortisol has permissive effect on glucagon and catecholamine activity
What does cortisol do in non-stress conditions and how?
cortisol has permissive effect on glucagon and catecholamine activity
protects liver against hypoglycemia
when blood glucose levels drop, pancreas secretes glucagon to bring it back up through gluconeogenesis and glycogen, but glucagon can’t do that adequately without the presence of cortisol
helps arterioles maintain normal blood pressure
has permissive action on the reactivity of catecholamines by smooth muscle cells that surround arterioles → cortisol basically increases vascular smooth muscle responsiveness and promotes vasoconstriction
basal levels of cortisol help maintain normal blood pressure
What has happened in experiments when adrenal glands have been removed?
the subjects have died when exposed to any significant environmental stress
What impact does cortisol have on the immune system? How does it do this?
Cortisol suppresses immune system
cortisol prevents cytokine release and antibody production by WBC
cytokine signals white blood cells to activate and proliferate
cortisol inhibits inflammatory response by decreasing leukocyte mobility and migration
leukocytes are WBC, so very important for immune system
What are pharmaceutical applications of cortisol?
because cortisol inhibits inflammatory response by decreasing leukocyte mobility and migration it has been used as an anti-inflammatory drug
can be used to treat bee stings, pollen allergies or even to prevent the rejection of transplanted organs
What do cortisol pathologies usually result from? What are the 2 main types? What is an uncommon cause?
cortisol pathologies result from too much or too little cortisol
1) hypocortisolism
cortisol deficiency
2) hypercortisolism
cortisol excess
aka Cushing’s syndrome
Abnormal tissue responsiveness is an uncommon cause of adrenal steroid disorders