Mood disorders and antidepressants 2
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
53 Terms
What causes mood disorders?
1. Genetics
2. Neurotransmitter dysfunction
3. Psychosocial/ environmental factors
Give an example of a mood disorder with strong genetic links
Bipolar disorder - 93% genetic link
Describe what neurotransmitters are linked to mood disorders
1. Monoamines (dopamine, noradrenaline, 5-HT) - depression
2. Neuroendocrine - depression due to increases in cortisol
3. Neurogenesis - cortisol damages neurogenesis which is implicated in depression. There are a small amount of nerve cells in the brain which can grow, renew, divide and integrate into neuronal circuits to enhance adaptability of brain. Could new antidepressant drugs stimulate neurogenesis?
4. Neuroinflammation - inflammatory mediators are raised in a subset of depressed patients
5. Glutamate - ketamine MoA works by binding to glutamate NMDA receptor, therefore is glutamate could be involved in what causes depression.
What psychosocial and environmental factors can contribute to mood disorders?
1. Stressful life events e.g. childhood abuse, loss of job, marriage breakdown
2. Medication e.g. corticosteroids, oral contraceptives, interferon (targeting inflammatory factors)
3. Co-morbidities e.g. drug dependence, chronic pain
Describe how neurotransmitter can influence major depressive disorder (MDD)
Depression is related to low levels of 5-HT and or noradrenaline (and or dopamine)
Describe how neurotransmitter can influence mania
Mania is related to high levels of noradrenaline and dopamine and low levels of 5-HT.
What is evidence that 5-HT is involved in depression?
1. Tryptophan (an amino acid) is the precursor for 5-HT. When people recovered from depression are tryptophan depleted, they have a relapse in depression.
2. When reserpine is used, it inhibits 5-HT and NA storage which lowers mood in patients.
What is the monoamine hypothesis?
Depression is a functional deficit of 5-HT and or noradrenaline in the brain.
Dopamine is involved in reward and motivation neurotransmitter.
Noradrenaline is alive, alert, awake neurotransmitter.
Therefore, it makes sense that a deficit in both would cause depression
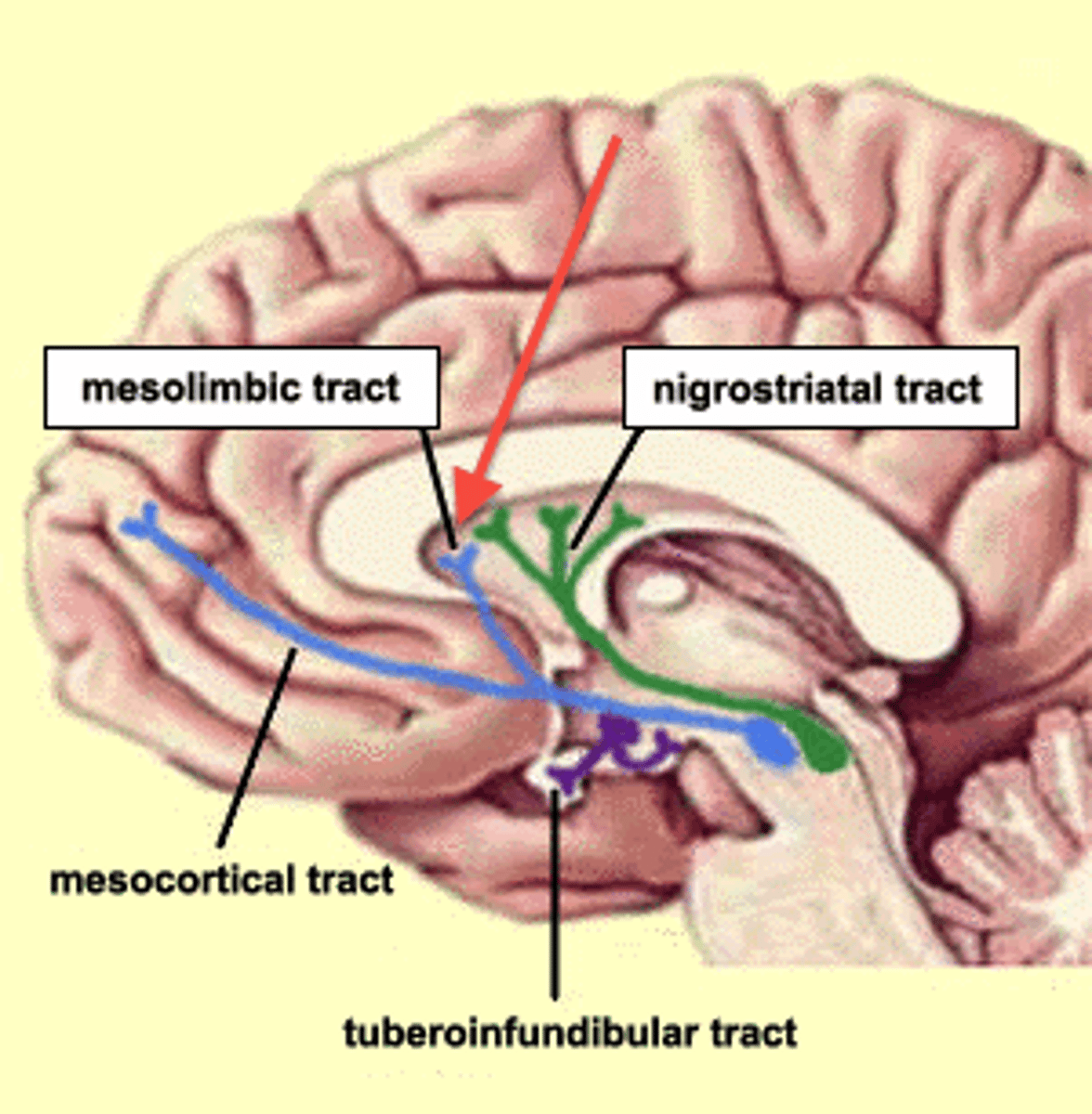
What areas of the brain regulate mood?
1. Ventral tegmental area (VTA)
- sends dopaminergic projections to other areas
2. Dorsal raphe (DR)
- sends serotonergic projections to other areas
3. Locus Coeruleus (LC)
- sends noradrenergic input to other areas.
Low activity in these brain regions is involved in depression. Therefore this links to how monoamines may be involved in depression.
Give examples of brain imaging
PET
fMRI
What are the different types of brain imaging studies?
1. Structural studies:
Focus on number of or connections among cells
2. Functional activation studies:
Focus on activity levels
Describe the results from brain imaging in depressed patients
There is diminished activity in the
- prefrontal cortex
- anterior cingulate
- hippocampus
There is elevated activity in the amygdala (mediates response to emotional stimuli)
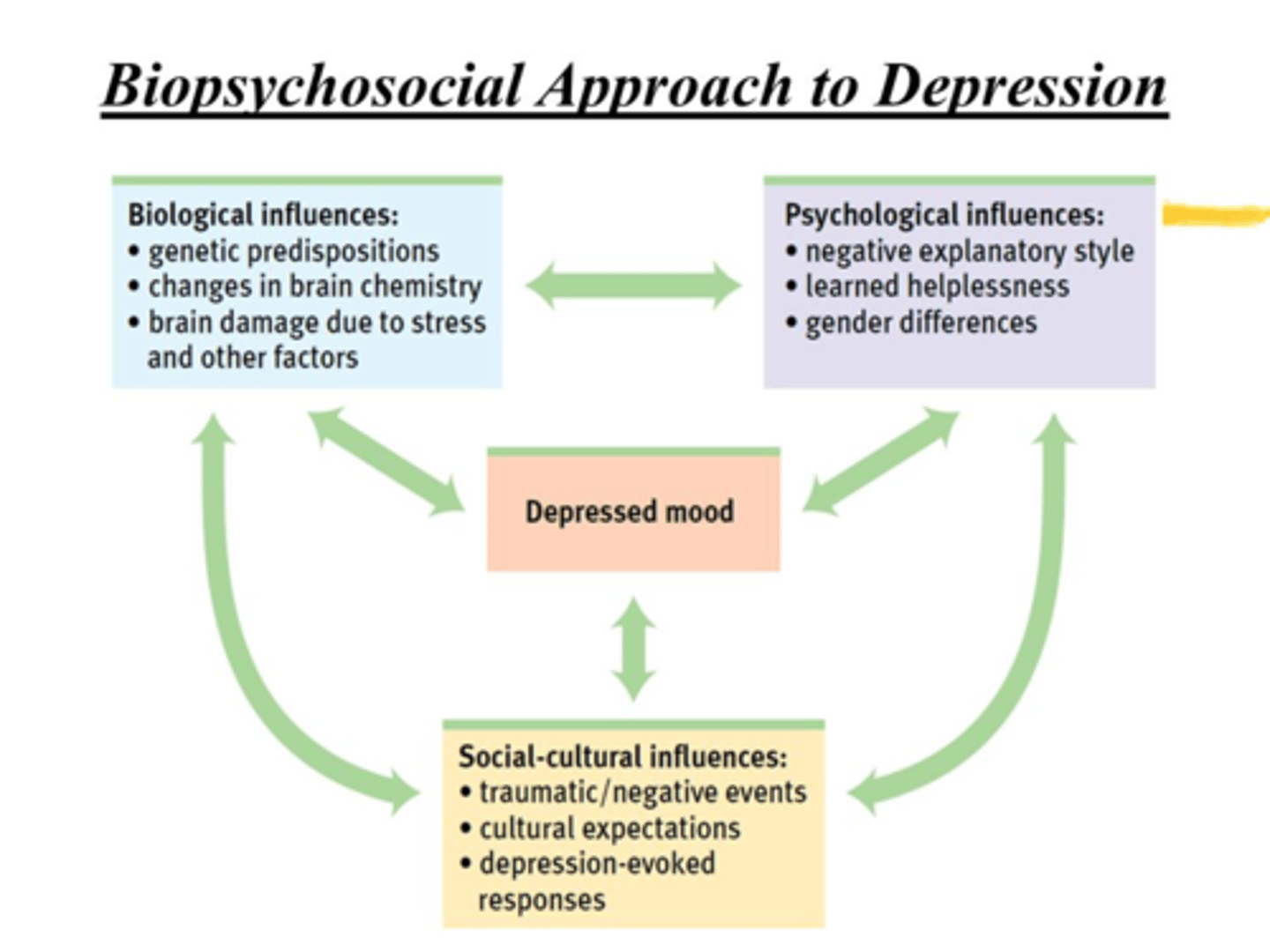
What is the biopsychosocial model of depression?
1. Biological vulnerability e.g. gender, genes
- Different genes could be impaired which subtly alter levels of neurotransmitters
2. Exogenous stressors
e.g. Trauma, illness, environment
This alters chemistry of brain and how neurotransmitter is released
3. Mood regulatory circuits e.g. connectivity, chemistry
- These can all then cause a depressive episode
Describe the treatment approach for depression
It is a stepped care model. It is based on the severity of depression
mild-moderate, moderate-severe, severe and complex depression.
Mild-moderate depression
- Low intensity psychosocial interventions
- May consider medication
Moderate-Severe
-High intensity psychosocial intervention
- Medication is recommended
Severe and complex depression
- Medication is highly recommended
-High intensity psychosocial intervention
- Electroconvulsive therapy
What are the different psychological treatments for mood disorders?
1. Interpersonal psychotherapy (IPT)
- Short term treatment; focuses on current relationships
2. Cognitive therapy
- Monitor and identify automatic thoughts
- replace negative thoughts with neutral or positive thoughts
3. Mindfulness based cognitive therapy (MBCT)
- strategies e.g. meditation to prevent relapse
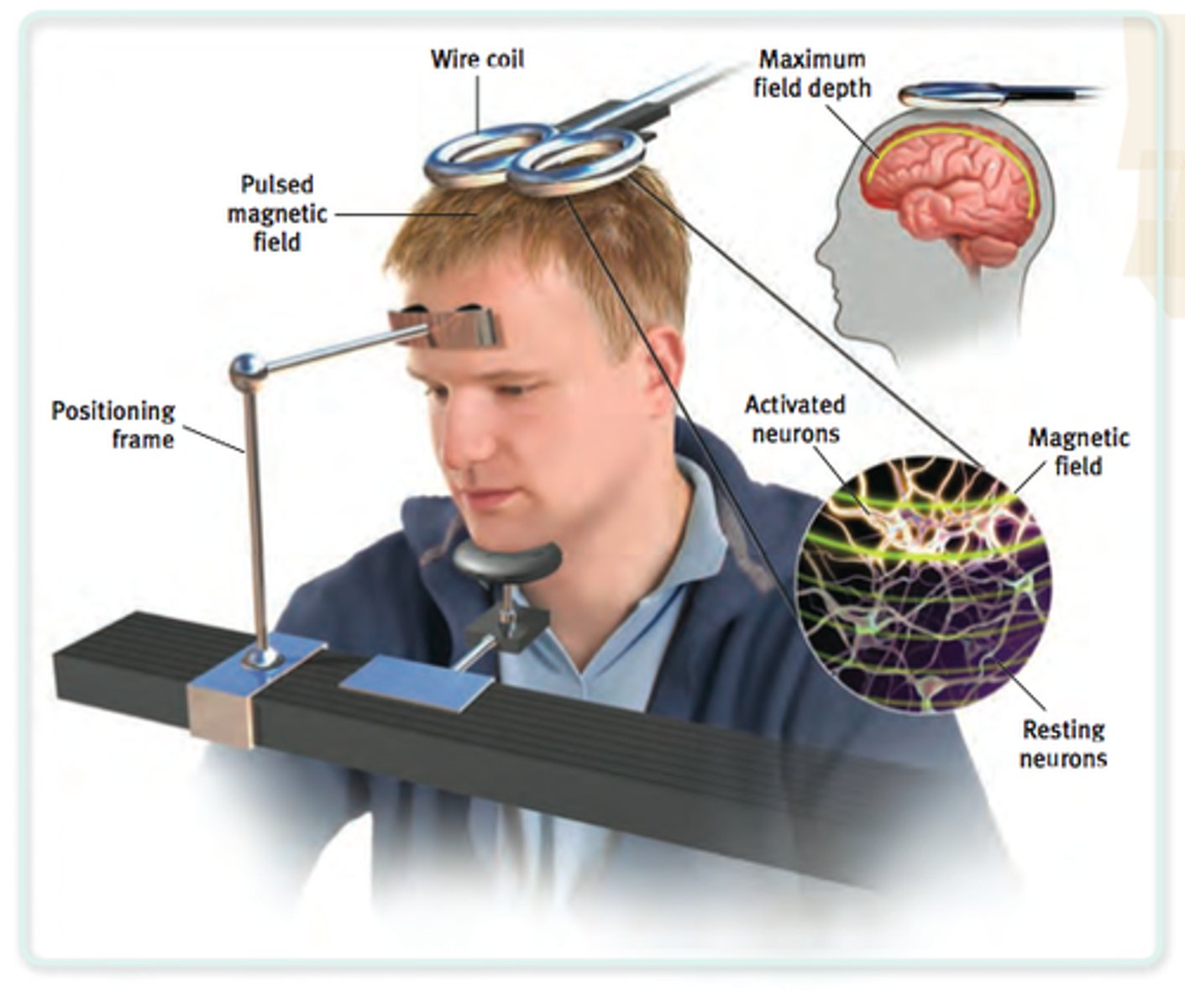
Describe electroconvulsive therapy
This is where needles are inserted into the brain to stimulate recurrent electrical activity.
It is thought to "reset the brain"- people don't know why it works.
However, it is a controversial treatment as some people experience memory loss alongside treatment.
This is reserved for people who don't respond to antidepressants.
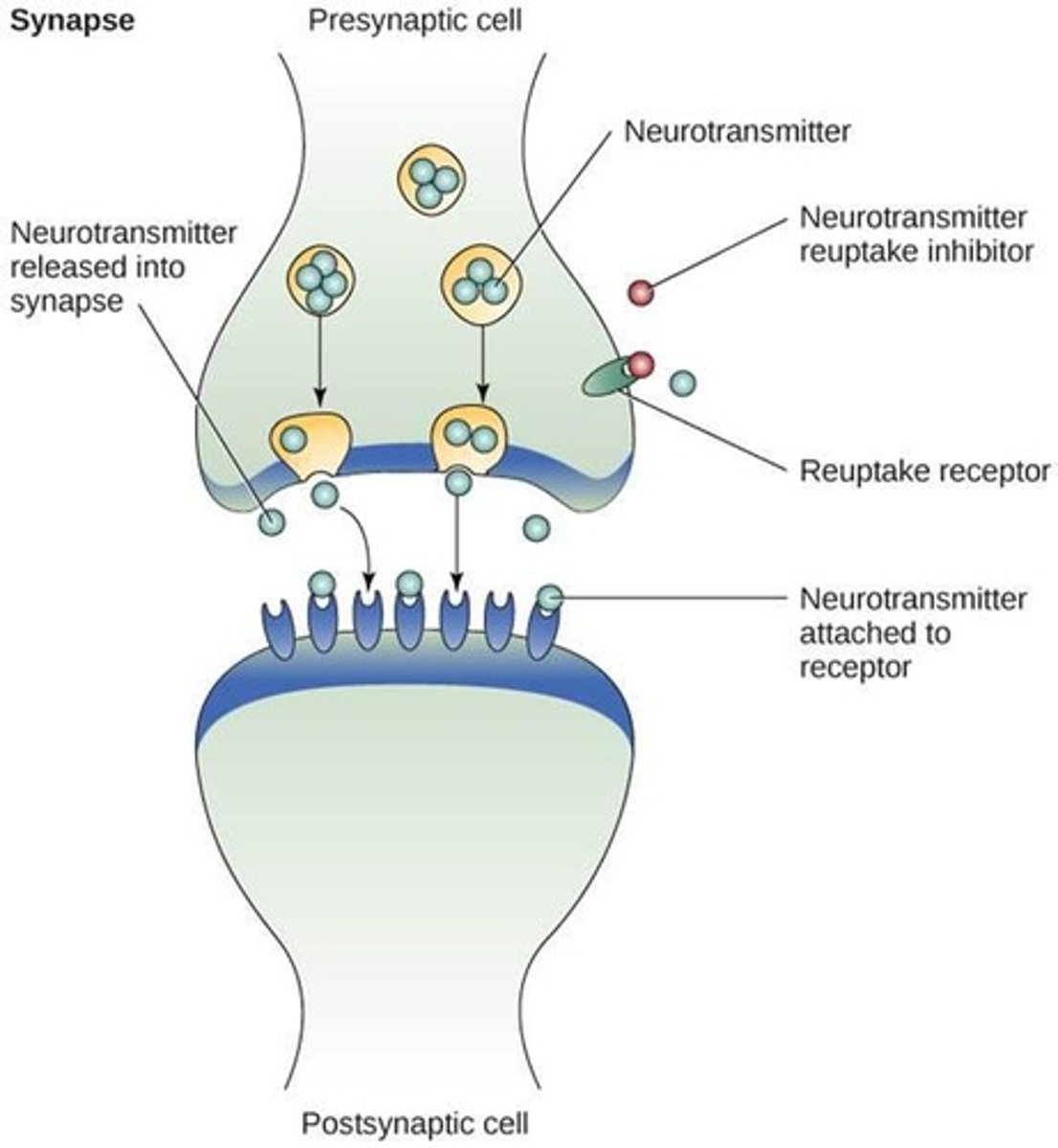
What are the different classes of antidepressants?
1. SSRIs - selective serotonin reuptake inhibitor
2. SNRIs - serotonin and noradrenaline reuptake inhibitor
3. TCAs - tricyclic antidepressants
4. MAOIs - monoamine oxidase inhibitors
5. Receptor blockers
- mirtazapine
- nefazodone
What is the first line antidepressant therapy?
SSRIs
What were the first antidepressants made?
Monoamine oxidase inhibitors
What is the mechanism of action of monoamine oxidase inhibitors?
Traditionally, they irreversibly inhibit monoamine oxidase (MAO). MAO is expressed in
- nerve terminals and regulates the concentration of noradrenaline/ 5-HT
- in the gut. Here it inactivated ingested amines
MAOIs increase 5-HT, NA by inhibiting metabolism
What are the different types of MAOs and their receptor preference?
MAOA - substrate preference = 5HT (serotonin)
MAOB - substrate preference = DA (dopamine)
Give examples of monoamine oxidase inhibitors
Phenelzine, tranylcypromine, iproniazid
What is the cheese action with irreversible MAOIs?
This is when non-selective MAOIs block all MAO. MAOB in gut is therefore blocked.
Tyramine in diet usually is metabolised by MAO. If it is not metabolised, it is absorbed as tyramine and displaces NA in the nerve terminal.
Therefore, ingested tyramine has sympathomimetic effects - significant for CVD symptoms. This is known as the cheese reaction of as cheese has high tyramine content.
This could cause a hypertension crisis, headache, angina or cardiac arrest.
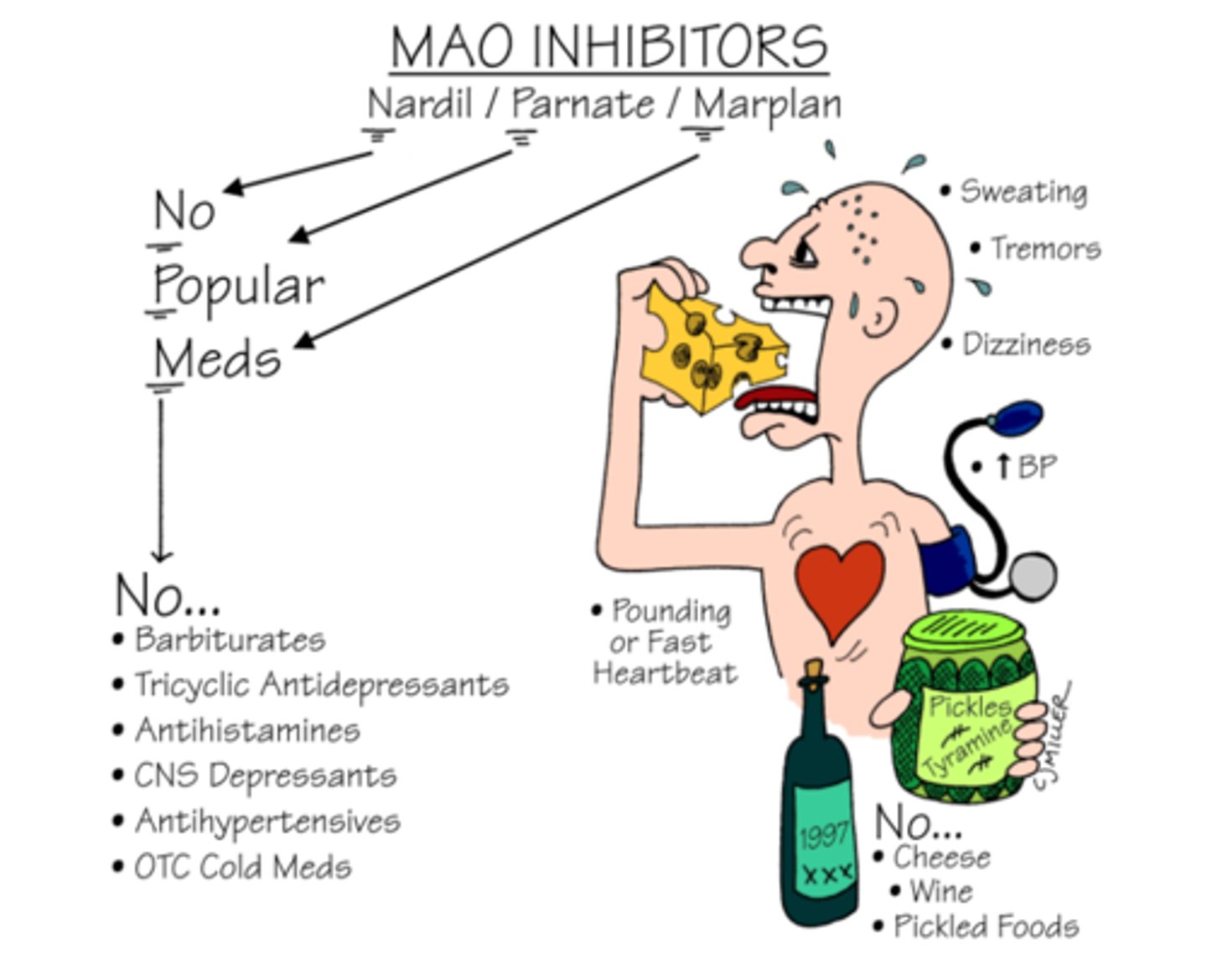
What are major side effects of MAOIs?
- Hypotension (sympathetic block)
- Atropine-like effects
- Hepatocellular jaundice
What is RIMA?
Reversible Inhibitors of MAO A
RIMA is a new type of MAMO inhibitor
These are better than older MAOIs because their inhibition is
- reversible (so high levels of tyramine can overcome MAO inhibition)
- selective (MAOA receptor).
Therefore don't cause the "cheese reaction".
Give an example of a RIMA
Moclobemide
What is the mechanism of action of tricyclic antidepressants (TCAs)?
They block the reuptake of 5HT into nerve terminals. Therefore 5HT levels are boosted in the synapse.
These are relatively non-selective.
TCAs increase 5-HT, NA by blocking reuptake
Give examples of tricyclic antidepressants (TCAs)
Imipramine, amitriptyline, clomipramine
How come TCAs have relatively wide spread side effects?
TCAs are relatively non-selective therefore they can bind to many different receptor types:
- muscarinic receptors
- histamine receptors
- serotonin receptors
Therefore, they cause side effects associated to the receptor they block
What are the major side effects of TCAs?
- Sedation
- Atropine-like (muscarinic blockade)
- Postural hypotension
- Mania and convulsions (rare)
- Dysrhythmia and heart block
What are signs of a TCA overdose?
- Prominent antimuscarinic activity
- Confusion, mania
- Cardiac arrhythmias
- Coma
- Respiratory depression
- Hypoxia
What drugs do TCAs have an interaction with?
- Alcohol
- Hypotensive drugs
- NSAIDs
- MAOIs
What is the mechanism of actions of SSRIs (selective serotonin reuptake inhibitors)?
They are specific to 5-HT receptors and work by blocking 5-HT (serotonin) reuptake. Therefore, more serotonin in the synapse.
The 'emotional' components of depressive illness are sensitive to antidepressant effects on 5-HT systems.
SSRIs increase 5-HT by blocking reuptake
Give examples of SSRIs
Fluoxetine (Prozac), paroxetine citalopram
Compare the use of SSRIs to the use of TCAs
SSRIs are considered safer than TCAs in overdose
- there is no evidence that one is more efficacious than the other
- there is no evidence that one has more rapid onset than the other.
SSRIs arguably have a better side-effect profile.
What is the mechanism for bupropion?
It inhibits the reuptake of noradrenaline and dopamine.
Give examples of monoamine receptor blockers
mirtazapine, trazodone, mianserin, agomelatine
What is the MoA of mirtazapine?
5-HT2c and α2 adrenoreceptor antagonist which directly increases noradrenaline and indirectly increases 5-HT
What is the MoA of mianserin?
Blocks multiple 5HT receptors and α1 and blocks alpha 2 adrenoreceptors
What is the MoA of agomelatine?
Blocks melatonin receptors
- This is useful for depression associated with sleep disturbance
What is the MoA of trazodone?
It blocks 5-HT2a and 2c and blocks α1 adrenoreceptors
Describe the efficacy of antidepressants
< 40% achieve remission from symptoms
Good at preventing relapse in recurrent major depressive disorder (MDD)
How long does it take antidepressant drugs to work?
4-6 weeks to see therapeutic benefit
What are some safety issues related to antidepressants?
- Can make patients feel worse in the first 7-10 days so higher risk of suicide (but this usually subsides short term)
- Older antidepressants are cardiotoxic which is dangerous in an overdose
What are some issues with the monoamine theory?
Boosting neurotransmitters doesn't seem to "fix" depression. It takes longer and a combination of strategies for depression symptoms to get better.
Describe use of ketamine as an antidepressant
- It is licenced for depression
- Mechanism of action is not known
- Safety questioned, what is the consequence of excess ketamine?
- It is not recommended as treatment by NICE
What medications are used for bipolar disorder?
Mood stabilising drugs
1. Lithium
2. Anticonvulsants
3. Antipsychotics
Give examples of anticonvulsant drugs
Valproate, lamotrigine
Give examples of antipsychotic drugs
Olanzapine, risperidone, quetiapine, aripiprazole
Describe the use of lithium for the treatment of bipolar disease
- It is used prophylactically for bipolar disease
- It reduced both depressive and manic phases
- It is used long term to prevent relapse
- Effects are seen 3-4 weeks after treatment
- Has a narrow therapeutic window (0.4 mmol/L - 1.0 mmol/L); if levels rise above 1.5 mmol/L it can be potentially fatal
- Requires plasma concentration monitoring
What are the acute side effects of lithium?
- Polyuria and polydipsia (renal problems)
- Weight gain
- Aggravation/ precipitation of skin disorders
- Tremor, Muscle twitching, Dysarthria
- Nausea, Vomiting, Appetite loss, Diarrhoea
- Sluggishness, Languidness, Drowsiness
- Coma, Hyper-reflexia, Fasciculations
- Choreiform and Parkinsonian motor symptoms
- Limb Hyperextension, Seizure and Convulsions
What are the chronic side effects of lithium?
- Thyroid goitre
- Nephrotoxicity
- Hair loss
What are the proposed theories for lithium's MoA?
1. Li+ (monovalent cation) so can go across voltage-gates Na+ channels
2. Prevents IP3 formation by inhibiting phosphatidyl inositol (PI)
3. Inhibits glycogen synthase kinase 3 (GSK3) involved in apoptosis
Unsure how any of these actions relate to mood disorders