Neuro Physio
1/265
Earn XP
Description and Tags
Neuron, Synapse, CSF/BBB, reflexes, UMN/LMN, control of movement
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
266 Terms
what is the functional unit of the nervous system?
neuron
what are the 4 parts of the neuron?
dendrites, cell body, axon, presynaptic terminal
what do neurons contain as a results of an ion pump?
resting electrical membrane potential
what pump is important in maintaining the resting electrical membrane potential
Na/K pump
what can change the membrane potential?
synaptic signals
what is the path of an axon potential?
begins at the axon’s initial segment and travels along the length of the axon
what is the purpose of the nervous system?
to receive sensory information, integrate that information to plan a response, then to initiate a motor response
what is the function of the dendrite?
it is the receptive region of the neuron and receives the chemical signals from other neurons
what does the cell body contain?
the nucleus, DNA/RNA, and organelles that create proteins for the cell
what is the function of the axon?
conducting unit of the neuron; rapidly transmits an electrical signal over distance from initial segment to pre-synaptic terminal (carries action potential); bidirectional
what are some larger axons surrounded by? and what is the purpose for this?
myelin; increases the conduction velocity in the axon
what is located at the distal end of the axon?
presynaptic terminal
what is the function of the presynaptic terminal?
stores and releases neurotransmitters in response to an action potential propagated down the axon
what does the Na/K pump do?
a ATP dependent pump that forms a resting membrane potential by pumping Na out of the neuron and K into the neuron, against the concentration gradients
what is the ratio of Na to K pumped across the membrane and what does this cause?
For every 3 Na molecules pumped out of the cell, 2 K molecules are pumped into the cell; CAUSES a net NEGATIVE charge in the interior of the cell
what can disturbances of the resting membrane potential cause?
misfiring of the neurons leading to seizures or other neurologic diseases
how is the membrane potential altered?
changed by synaptic messages from other neurons or in response to environmental stimuli with sensory organs
what is the impact of signal messages on the neuronal membrane?
open or close ion channels in the membrane changing the potential
what occurs if the change reaches a certain threshold?
action potential
what is the mV of the threshold for an action potential to occur?
-50 mV
what is the type of synaptic message that causes the membrane potential to become more positive?
excitatory postsynaptic potential (EPSP)
EPSP ______ the chance that the membrane potential reaches the threshold required to trigger an action potential.
increases
what ion is increased during an EPSP?
influx of Na
what is the synaptic message that causes the membrane potential to become more negative?
inhibitory postsynaptic potential (IPSP)
IPSP_______ the chance that the membrane potential reaches the threshold required to trigger an action potential.
decreases
what ions can be involved during an IPSP?
Cl influx or K efflux
True/false: a single EPSP can initiate an action potential.
false; a single EPSP is not sufficient to cause the membrane potential to reach the threshold to induce an action potential
what is required for an action potential to be triggered?
summation of EPSPs and IPSPs; if more EPSPs present than IPSPs than the membrane potential can become positive enough to reach the threshold potential to trigger an action potential
what are the two types of summation?
spatial summation; temporal summation
what is spatial summation?
multiple excitatory neurons giving the same signal
what is temporal summation?
a single excitatory neuron that repeatedly fires
what does an action potential consist of?
immediate and massive opening of voltage gated Na channels that allow a large influx of Na ions causing the inside of the cell to become more positively charged; followed by the Na channels quickly closing and voltage-gated K channels open to allow K to leave the cell causing the inside of the cell to become more negative
what is the path of the action potential?
initiate of AP when stimulus reaches threshold, fixed amplitude, uniform shape, not graded; begins at axon’s initial segment, rapidly spreads down axon
what are the two stages of action potentials
depolarization stage; repolarization stage
what occurs during the depolarization stage?
depolarization above threshold triggers all-or-none response; opening of voltage-gate Na channels (cell becomes more positive)
what occurs during repolarization stage?
Na channels close and voltage-gated K channels open; rapid diffusion of K out of cell (cell gets more negative)
how does an action potential travel down the axon?
action potential is actively propagated down the entire length of the axon, the dramatic influx of Na at the initial segment depolarizes the adjacent segment of the membrane and this continues down the axon
what increases the conduction speed of an action potential?
larger diameter; myelination
what are the junctions between the myelinated segments (schwann cells)?
node of Ranvier
what are located at nodes in increased density?
Na channels (where action potentials occur)
what is the process in which the action potential jumps from node to node?
Saltatory conduction
what are the two types of synapses?
electrical, chemical
where are the electrical synapse usually located?
smooth muscle, cardiac muscle
how do electrical synapse function?
ionic current flows from one cell to another via gap junctions
where are chemical synapses located?
majority of CNS and neuromuscular junction (skeletal muscle)
how does a chemical synapse function?
neurotransmitter release from presynaptic cell in response to an action potential; chemical diffuses across space between cells and binds to receptors on post-synaptic cell to generate a postsynaptic potential
what are the three anatomical parts of a NMJ?
presynaptic terminal
synaptic cleft
postsynaptic muscle membrane
what is the purpose of a NMJ?
important to transmit a chemical message from the neuron to the muscle cell; allows the nervous system to control muscle contractions and movement
where is the presynaptic terminal located?
distal end of the axon
what does the presynaptic terminal contain?
synaptic vesicles containing neurotransmitter, mitochondria, and enzymes that synthesize neurotransmitter
what is the excitatory neurotransmitter at the NMJ?
acetylcholine (in the synaptic vesicles)
where is the synaptic cleft located?
narrow space between the presynaptic terminal of the neuron and the muscle cell (about 50 nm wide)
where is the post synaptic muscle membrane located?
the on the membrane of the muscle cell the nerve is acting upon
what are the invaginations on the postsynaptic muscle membrane and what is their function?
junctional folds; increase surface area
what are located within the junctional folds on a postsynaptic muscle membrane?
acetylcholine receptors
how is muscle innervated?
one nerve can innervate several muscle fibers; each muscle cell can only have 1 neuron
what does an action potential trigger at the NMJ?
action potential in the motor neuron triggers release of Ach that induces an action potential in the muscle cell
what are the steps in neuromuscular transmission? (7)
action potential in the motor neuron arrives at the presynaptic terminal
this opens the voltage gated Ca2+ channels and Ca enters the presynaptic terminal; critical for triggering release of Ach
synaptic vesicles fuse with the presynaptic membrane, release Ach into synaptic cleft
Ach diffuses across cleft to bind to nicotinic acetylcholine receptors; must reach threshold
Ach receptor contains a Na ion channel; when receptor is bound to Ach, the ion channel opens, allowing Na to enter the muscle cell, creating an EPSP in the muscle cell
once enough receptors are bound with Ach, an all or nothing action potential is triggered in the muscle cell that leads to a muscle fiber contraction
Ach binds briefly to the receptor; it is then destroyed by an enzyme called acetylcholinesterase
what is Ach broken down into by acetylcholinesterase?
acetic acid and choline molecules that are transported back into the presynaptic terminal to be recycled in acetylcholine synthesis
what does the breakdown of Ach prevent?
to only allow 1 muscle contraction; prevents unwanted muscle contraction after action potential passes
what is the role of calcium in NMJ?
increase in Ca causes synaptic vesicles to fuse to the membrane to release Ach
what is the disease of the NMJ that is characterized by decreased number of Ach receptors?
Myasthenia gravis
what are the two causes of myasthenia gravis?
mutation in Ach receptors (congenital myasthenia/puppies); immune destruction of Ach receptors (acquired myasthenia)
what does myasthenia gravis cause?
failure in neuromuscular transmission
what is a major clinical sign of myasthenia gravis?
exercise-induced paresis; in dogs esophageal dilation and regurgitation can also occur
how is myasthenia gravis treated?
use of drugs that inhibit acetylcholinesterase (pyridostigmine); allows Ach to be present in the cleft longer than normal giving it more time to bind to a receptor; in adults, can suppress immune system
what are the two signals that occur in the CNS nerve-to-nerve transmission?
excitatory (EPSPs) or inhibitory (IPSPs)
what are the CNS excitatory neurotansmitters?
glutamate, norepinephrine, epinephrine
what are the CNS inhibitory neurotransmitters?
GABA, glycine
what do the GABA receptors contain and what is its function?
contains Cl- ion channels; when GABA is bound to GABA receptor, Cl- channel opens allowing Cl- to enter the cell making the inside of the cell more negative inhibiting an action potential
what are examples of types of drugs that utilize GABA receptors and what are their effects?
sedatives and antiseizure meds (diazepam, pheno); act by binding to the GABA receptor and inhibiting neuronal activity
what does the Glycine receptor contain and what is its function?
Cl- channel; after binding, allows Cl- to enter the cell making it more negative, inhibiting the action potential
what disease process inhibit Glycine receptors and what is the effect?
tetanus; toxin inhibits glycine receptors and causes neurons to be more active; binding is irreversible, causes muscle rigidity, treated with antibiotics
What is CSF?
clear fluid, with small amount of protein and few lymphocytes
where is CSF produced?
choroid plexuses at a constant rate
Where is CSF located?
lateral, third, and fourth ventricles of the brain, and the subarachnoid space of the brain and spinal cord
what absorbs CSF?
arachnoid villi in the venous sinuses
what is the function of CSF?
cushioning the brain, regulating pressure and waste removal, protect brain and spinal cord
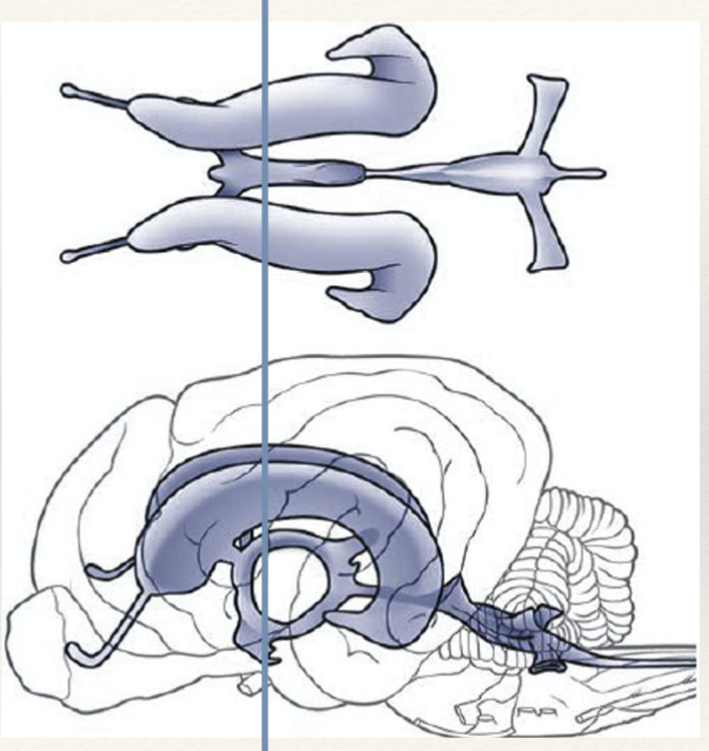
which ventricles is the line passing through?
both lateral and 3rd ventricle
what is the line passing through?
caudal end of the lateral ventricles and the mesencephalic aqueduct
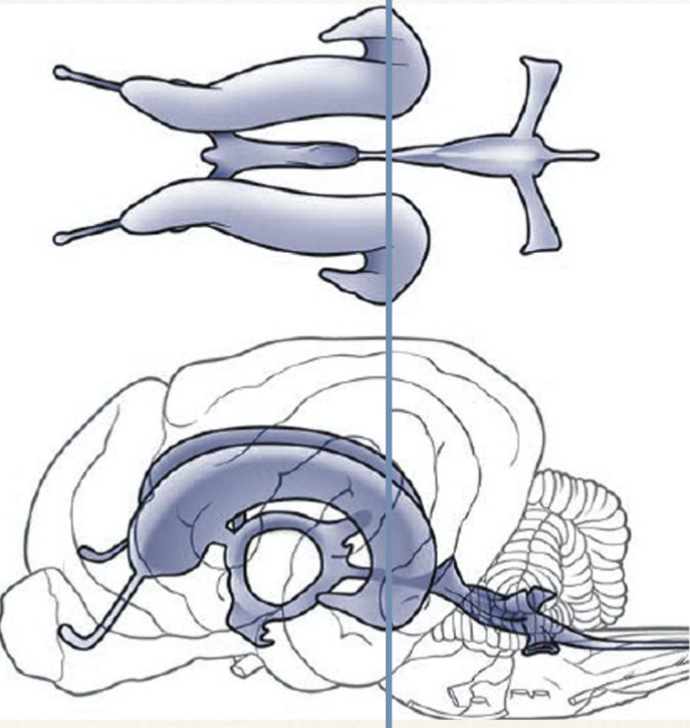
what ventricle is the line passing through?
fourth ventricle
how is the CSF produced?
plasma filtration by active transport of Na+ and requires an enzyme; performed by the choroid plexus in the lateral, 3rd, and 4th ventricles
what is the enzyme required for CSF production?
carbonic anhydrase
T/F; the rate of CSF production changes with the pressure of the brain.
FALSE: CSF is produced at a constant rate (0.03-0.5 mL/min) regardless of pressure
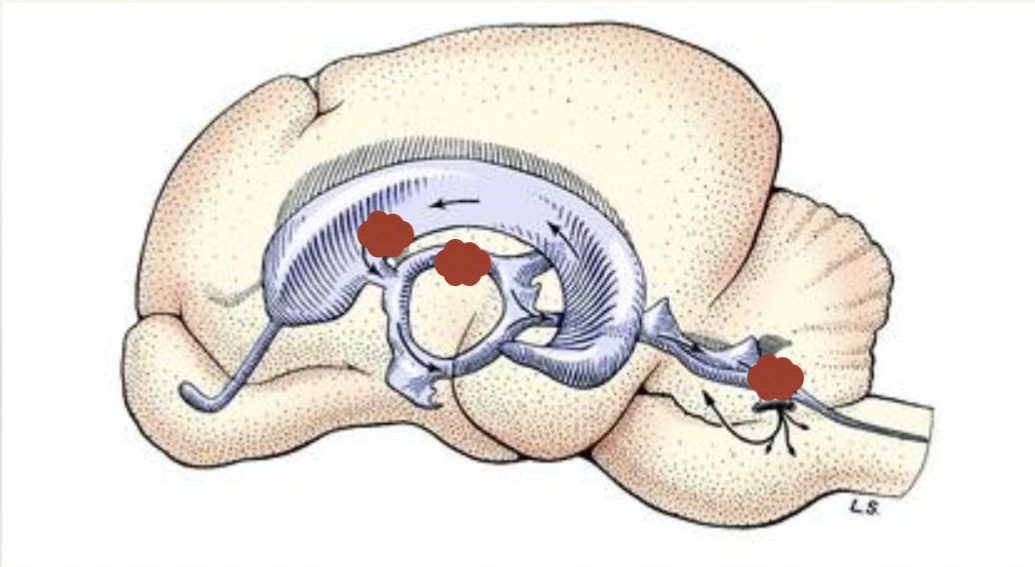
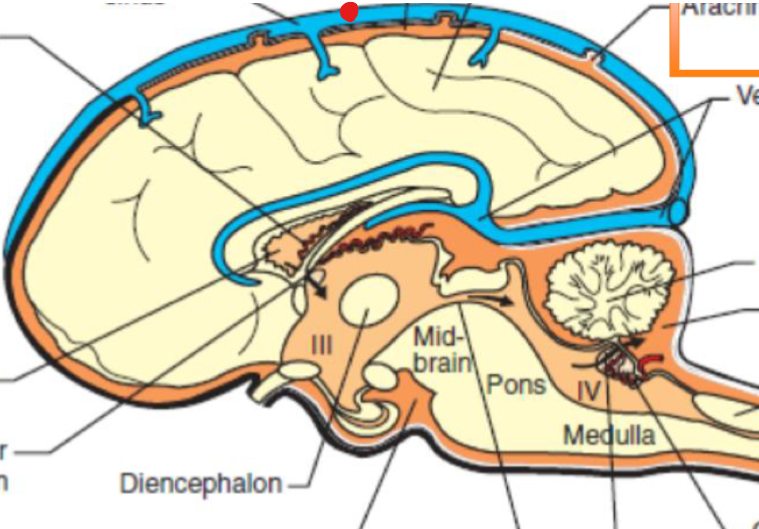
what is depicted by the red marks in this image?
choroid plexuses
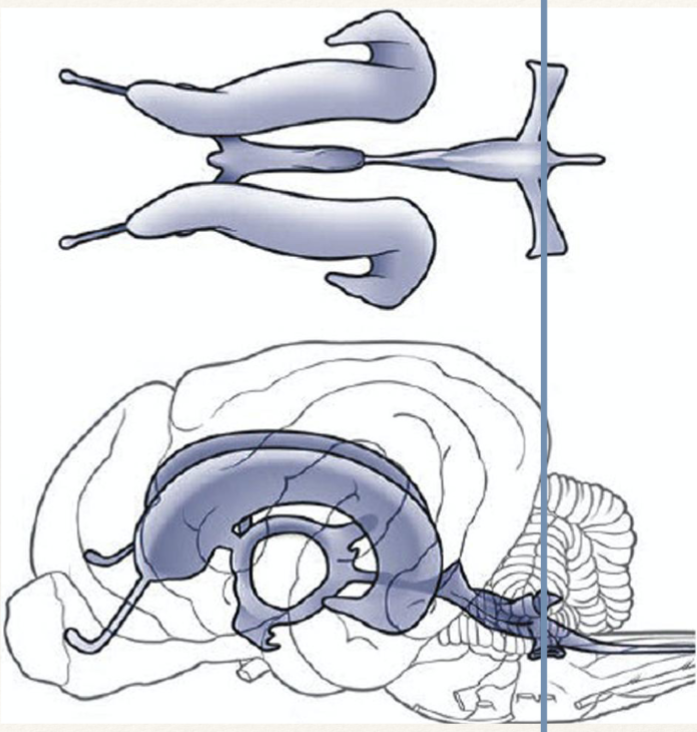
what is the path of CSF flow?
flows from cranial/rostral to caudal; lateral ventricles → 3rd ventricle → mesencephalic aqueduct → 4th ventricle
what is the flow of CSF caused by?
pressure gradient produced by cardiac pulsation of blood in choroid plexus
how is CSF absorbed in to the venous system?
CSF is absorbed into venous sinuses located on the surface of the brain; CSF moves from the subarachnoid space through arachnoid villi
what is indicated by the red dot?
sagittal sinus
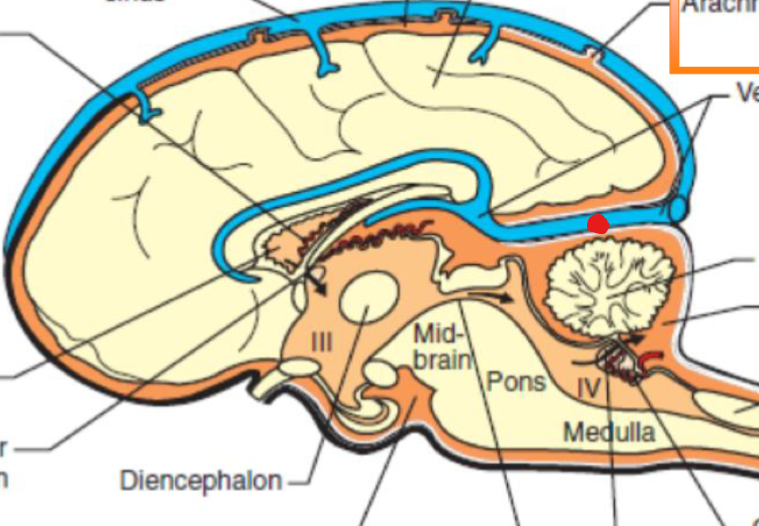
what is indicated by the red dot?
venous sinuses
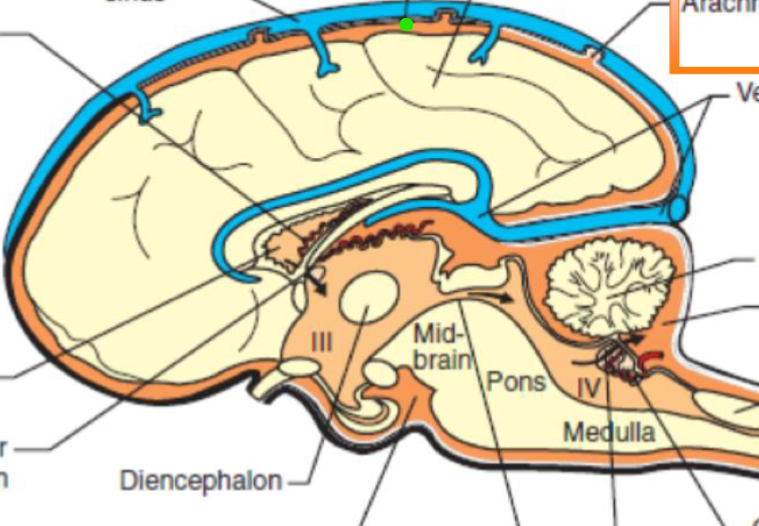
what is indicated by the green dot?
subarachnoid space
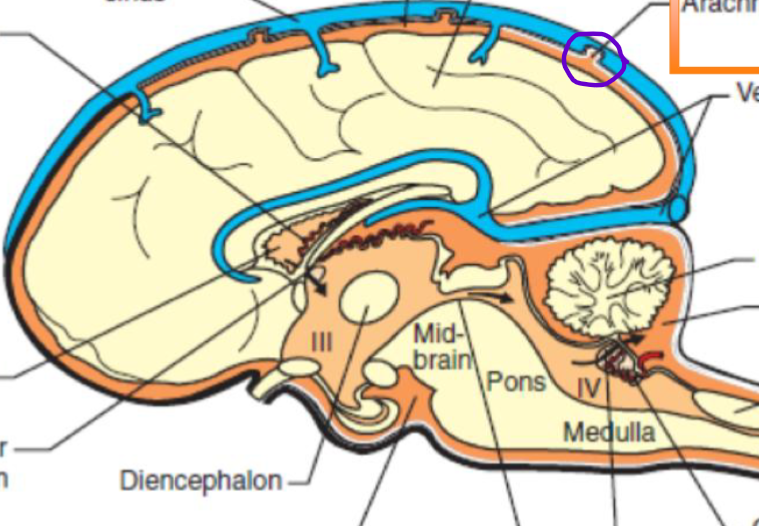
what is circled in purple?
arachnoid villus
what is the structure of the arachnoid villi?
single endothelial cell layer forms tiny projections of the subarachnoid space that protrude through the wall of the sinus; acts as one-way valve
what is the purpose of the arachnoid villi?
regulates CSF pressure; opens when pressure increases to drain fluid, stops draining when pressure decreases
what are the functions of CSF? (4)
cushions and protects the brain, spinal cord
regulates pressure in the CNS
provides a source of nutrition and waste removal
serves as a chemical buffer
what is the condition when there is a dilation of the ventricular system?
hydrocephalus
what is the cause of hydrocephalus?
an obstruction to CSF flow anywhere between its production in the choroid plexus and absorption in the venous sinus causes the fluid to accumulate since production is constant; prevents CSF absorption the ventricular system will dilate and compress the surrounding abnormality in CSF flow
what are the clinical signs of hydrocephalus?
behavior changes, ataxia, seizures, altered mentation, in young animals enlarged dome shaped skull, persistent fontanelle (soft spots in skull in neonates)
how is hydrocephalus treated?
surgically place a ventriculoperitoneal shunt to drain CSF from the ventricular system into the abdomen where is can be absorbed
what is the BBB
selective barrier between systemic circulation and the CNS