5.2 differentiating between ACSs
1/16
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
17 Terms
Patients with suspected ACS are typically categorized into two main diagnostic groups based on the initial ECG findings
a working diagnosis of STEMI.
categorized under non–ST-elevation ACS (NSTE-ACS).
Patients with acute chest pain or equivalent symptoms and persistent ST-segment elevation or its ECG equivalents
are given a working diagnosis of STEMI.
Most of these patients experience myocardial necrosis and elevated troponin levels,
meeting the criteria for myocardial infarction, although not all will have a final diagnosis of STEMI.
Patients with acute chest pain or equivalent symptoms without persistent ST-segment elevation or its ECG equivalents
re categorized under non–ST-elevation ACS (NSTE-ACS).
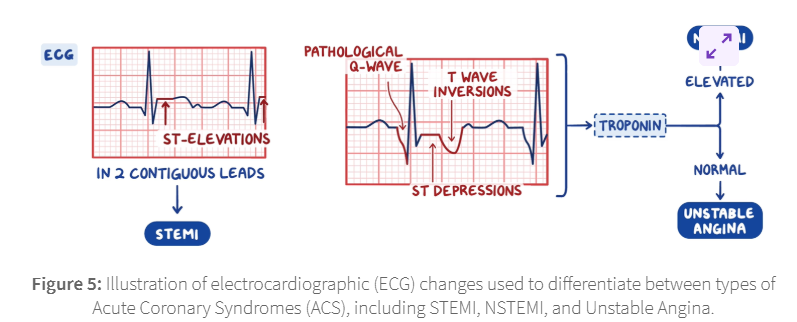
Within NSTE-ACS patients, findings suggestive of NSTEMI include transient ST elevation, ST depression, or new T wave inversions.
ECG should be repeated at predetermined intervals or if symptoms return. Unstable angina on the other hand presents without sustained ST-segment elevation
Once STEMI and very high-risk NSTE-ACS are ruled out
biomarkers become essential for confirming the diagnosis, assessing risk, and managing suspected cases of ACS.
Measuring a biomarker of cardiomyocyte injury, such as high-sensitivity cardiac troponin (hs-cTn),
is recommended for all patients with suspected ACS.
If the clinical presentation aligns with myocardial ischemia,
an elevation or decrease in hs-cTn levels above the 99th percentile of a healthy population supports the diagnosis of myocardial infarction
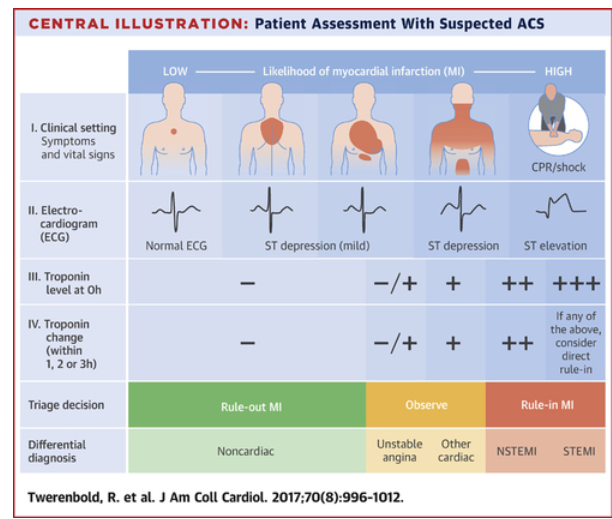
Hs-cTn assays offer greater sensitivity and diagnostic precision for detecting myocardial infarction upon presentation,
allowing for a shorter interval between the first and second troponin measurements.
Timely serial measurements lead to faster diagnosis and reduce emergency department stays, healthcare costs, and patient diagnostic uncertainty.
The preferred approach is the 0-hour/1-hour algorithm, with the 0-hour/2-hour algorithm as an alternative.
The management of ACS aims to provide supportive care and pain relief, and to prevent progression of cardiac injury.
Treatment should be started as soon as an ACS is suspected but should not delay transfer to hospital.
Pain relief should be offered as soon as possible with glyceryl trinitrate (sublingual or buccal).
. Intravenous opioids such as morphine may also be administered, particularly if acute myocardial infarction (MI) is suspected.
A loading dose of aspirin (300mg) should be given as soon as possible.
If aspirin is given before arrival at hospital, a note saying that it has been given should be sent with the patient
Other antiplatelet agents should only be offered once the patient is in hospital according to their diagnosis and risk factors
Oxygen should not be routinely administered,
however the patient's oxygen saturation should be monitored (ideally before hospital admission) and supplemental oxygen offered if indicated.
All patients admitted to hospital should be closely monitored for hyperglycaemia.
Those with a blood-glucose concentration greater than 11.0 mmol/litre should receive insulin—consider administration via a dose-adjusted infusion.