PSYCH 257 (Psychopathology) Exam 2
1/96
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
97 Terms
What are mood disorders? (Unipolar vs Bipolar)
Mood disorders involve experiences of depression and/or mania
Unipolar mood disorders have only lows (depression)
Bipolar mood disorders have highs and lows (Mania and Depression)
Is bipolar 1 unipolar or bipolar
Bipolar 1 would only be mania but still classified under bipolar; they should experience depression at some point.
Most people with Bipolar I will eventually experience depressive episodes at some point in their life — it's just not required for the diagnosis.
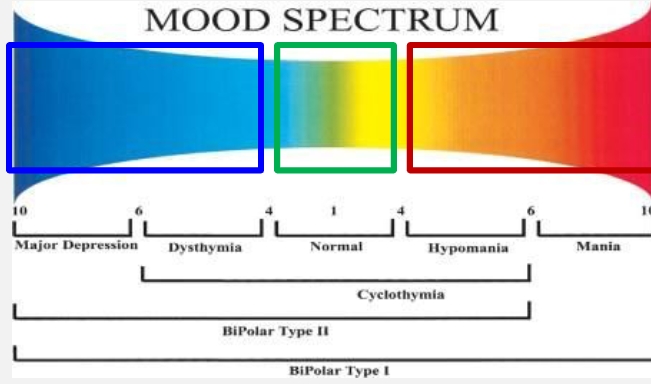
Mood Spectrum
goes from left/blue/low to right/red/high
Blue - Depression, dysthymia (longer less severe depression)
Red - Hypomania (less intense mania), mania
Major Depressive Episode
2 week period with depressed mood every day and/or diminished interest in almost all activities.
Symptoms: (must have 1 or 2)
1. Depressed mood most of the day, nearly everyday
2. Diminished interest or pleasure in all, or almost all, activities
Changes in sleep patterns/insomnia
Fatigue/reduced psychomotor
Concentration difficulty
Irritability
Changes in appetite and weight
Recurrent thoughts of death/suicide, guilt and worthlessness
*1 episode means 50% chance of another episode which would then be considered MDD recurrent 2 = 70%, 3 = 90%
Dysthymic disorder aka persistent depressive disorder
Depressed mood most of the day, more days than not for at least 2 years with consistent symptoms that don’t stop for more than 2 months.
(less severe but lasts longer)
2 or more symptoms:
Poor appetite/overeating
Sleep issues
Low energy
Poor self-esteem/hopelessness
Poor concentration/decision-making skills
During 2-year period, person has never been without symptoms for > 2 months at a time
Double Depression
a combination of persistent depression and major depressive episode; like someone with dysthymia experiencing a depressive episode
patient already has persistent depression and has a triggering incident pushing them into major depression.
Manic Episode
Distinct period of abnormally and persistently elevated, expansive or irritable mood; increased goal-directed activity or energy.
3+ symptoms or 4+ if mood is only irritable:
Big self-esteem/grandiosity
Less need for sleep
Lots of talking and racing thoughts
Distractibility
Increased goal-directed activity
Excessive involvement in pleasurable activities with potential for negative consequences
Marked impairment in social and occupational functioning
When is an episode considered manic?
Considered a manic episode when it goes on for a week or longer or the person is hospitalized
Hypomanic episode
a distinct period (4 days) of abnormally and persistently elevated, expansive or irritable mood; abnormally and persistently increased activity or energy.
How do you know it is hypomania?
a distinct period (4 days) of abnormally and persistently elevated, expansive or irritable mood; absnormally and persistently increased activity or energy.
4 days and not hospitalized
3+ symptoms or 4+ if mood is only irritable:
Big self-esteem/grandiosity
Less need for sleep
Lots of talking and racing thoughts
Distractability
Increased goal-directed activity
Excessive involvement in pleasurable activities with potential for negative consequences
No marked impairment
Mania
Mania:
Impairment of functioning and hospitalization
Abnormally and persistently elevated, expansive, or irritable mood
Abnormally and persistently increased goal-directed activity or energy
Week+
During mood disturbance, 3 (+) symptoms have persisted, or 4 (+) if mood only irritable:
1. Inflated self-esteem or grandiosity
2. Decreased need for sleep
3. More talkative than usual, or pressure to keep talking
4. Racing thoughts (“flight of ideas”)
5. Distractibility
6. Increase in goal-directed activity
7. Excessive involvement in pleasurable activities with potential for negative consequences
Work Examples: Take on unrealistic projects, quit job
Sleep Examples: Not sleeping days at a time
Marked impairment in social & occupational
Hypomania
Hypomania:
4+days
No marked impairment and no hospitalization
Work example: Working long hours, take on a new project
Sleep examples: sleep less than usual but still functioning normal
Distinct period of abnormally and persistently elevated, expansive, or irritable mood and Abnormally and persistently increased activity or energy
During mood disturbance, 3 (+) symptoms have persisted, or 4 (+) if mood only irritable:
1. Inflated self-esteem or grandiosity
2. Decreased need for sleep
3. More talkative than usual, or pressure to
keep talking
4. Racing thoughts (“flight of ideas”)
5. Distractibility
6. Increase in goal-directed activity
7. Excessive involvement in pleasurable activities with potential for negative consequences
Examples of hypomanic and manic behavior
Hypomanic:
Spending extra money on clothes and gadgets (still within budget)
More talkative
Feeling confident and believing that you can accomplish a lot
Manic:
Talking non-stop, interrupting conversations, nonsensical speech
Invincible and famous
Driving recklessly
Starting multiple creative projects but not finishing any or writing nonsensical works
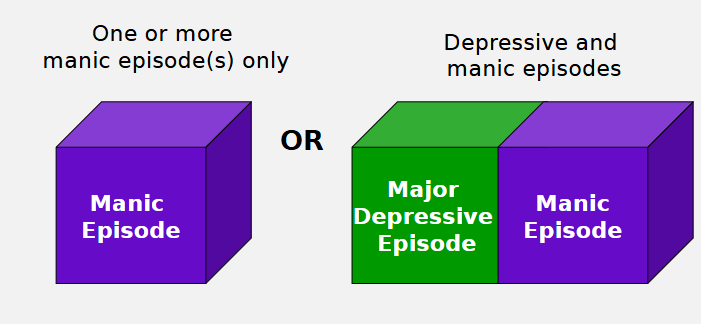
Bipolar 1
Bipolar 1: At least 1 manic episode lasting 7+ days (or requiring hospitalization)
Diagnosed based on mania alone
Can be only mania (we assume they will eventually have a depressive episode but it is not mandatory) and ranges to major depression
More focus on mania - if they have ever had one full episode
Bipolar 1 = Mania + Maybe Depression
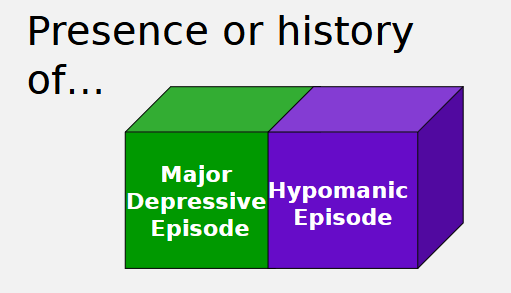
Bipolar 2
Bipolar 2: At least 1 hypomanic episode (4+ days) AND 1 major depressive episode
Depression is required for this one
ranges from major depression to hypomania, requires a presence or history of major depressive episode and a hypomanic episode.
hypomania alone is not generally impairing
Often misdiagnosed as depression - hypomanic episodes can go unrecognized “feeling better”
More focus on depression
Bipolar 2 = Depression + Hypomania
Cyclothymic Disorder
milder, long-term version of bipolar disorder
hypomanic and depressive symptoms with patterns that last at least 2 years (1 year for children).
Frequent hypomanic & depressive symptoms, but not severe enough for Bipolar I/II or MDD
Combination of persistent depressive disorder and hypomania
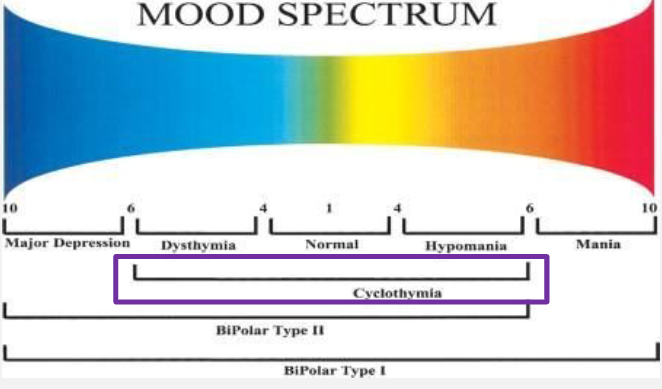
Cyclothymic disorder vs Bipolar 2
Cyclothymia is not full blown depression, going back and forth between hypomania and depression quickly. Generally bipolar 1 or 2 does not go between the episodes as quickly.
Biological causes of mood disorders
Genetic predisposition
Neurotransmitter imbalances (seratonin, norepinephrine, dopamine)
Too much = mania
Too little = depression
Endocrine system; cortisol
Sleep disruptions
Amygdala and Hippocampus
Amygdala; mood
Hippocampus; causing memory loss (some people claim to have no memory of their depressive episode)
Genetic predispositions for Bipolar vs MDD
Higher genetic influence in Bipolar (70-80)
Lower in MDD (unipolar) (30-40)
Neurotransmitter imbalances in Bipolar and MDD (cortisol, dopamine and norepinephrine)
Bipolar: Excess dopamine and norepinephrine (fight or flight) in mania with deficit in depression
MDD (unipolar): Chronically elevated cortisol (stress hormone)
Endocrine System in Bipolar and MDD (cortisol)
Bipolar: Fluctuating cortisol levels between episodes (lower in depressive)
MDD (unipolar): Chronically elevated
Sleep Disruptions in Bipolar and MDD
Bipolar: Poor sleep = disruptions in hormones = manic episodes
Sleep deprivation increases dopamine activity, which fuels manic symptoms
MDD: Poor sleep = hormonal imbalances = poor mood regulation = low mood
Stressful life events and learned helplessness in Bipolar and MDD (MD)
Bipolar
Stressful life events can trigger depressive and manic episodes. High stress = less mood stability, impulsive coping, sleep disruption
Learned helplessness can contribute to depressive episodes
MDD (Unipolar)
Major stressors can trigger depressive episodes, chronic stress mantains depression by increaseing negative thought patterns and hopelessness
Learned helplessness = persistant failures or uncontrolable negitive thoughts leading to lack of motivation, powerlessness, often the cause of short-term episodes
Major Depressive Disorder
Depressed mood or loss of interest for at least 2 weeks and 5 total symptoms the list
No history of mania/hypomania
1 Depressive Episode = MDD single episode
Greater than 1 = MDD Recurrent
Pessimism vs Neuroticism
Pessimism is a way of thinking: expect the worst outcome / negative viewpoint
"Things will probably go wrong"
Persistent in depressive phases of bipolar
Fuels hopelessness and depression through negative thinking patterns (e.g., “Nobody likes me”
Neuroticism is a personality trait that influences emotional regulation (experience a lot of negative things)
Neuroticism makes individuals emotionally reactive and prone to anxiety, depression, and mood swings - "I feel anxious or upset a lot"
Individuals with high neuroticism tend to ruminate and experience
Medicating Depressive Disorders and Bipolar disorders
Depressive Disorders:
Meds generally inhibit reuptake of neurotransmitters (helps keep serotonin, dopamine and norepinephrine available)
Trycyclic Antidepressants
Monoamine Oxidase Inhibitors (stop an enzyme called monoamine oxidase from breaking down certain neurotransmitters in the brain)
Selective Serotonin Reuptake Inhibitors
Bipolar disorders
Lithium: regulates rate of nurostransmission
Valproate: Increases GABA, a calming neurotransmitter
Cognitive Targets
Cognitive Targets: Negative bias thinking
Looking at how people interpret things (if they always think of the bad side balance with evidence and using all of the information)
Behavioral Activation
Behavioral Targets: often people don’t feel motivated to do anything and therefore don’t receive the dopamine from doing something making them feel more down – you need to get them up and moving (have to start really small)
Often you would start with mastery (something they can accomplish easily – listening to a song or lighting a candle)
Medical Adherence and regularity
Medication Adherence: Especially important for bipolar
Not taking them can cause bad side effects that can cause difficulty
Staying on them even if the side effects are bad
Regularity: sleeping, routines and medication even if it doesn’t feel good it helps a lot – even sleeping in can cause you to not sleep well the next night spiriling, etc.
Really important for bipolar as well as avoiding stressors
Suicide and heightened risk factors
Risk of suicide is significantly increased among those with mood disorders
Bipolar is especially at risk (feeling depressed but often too down to do it – then become manic and can follow through with plans)
Heightened Risk Factors:
Male gender
History of previous suicide attempts
Combined substance use
Periods of severe depression or mania
Feelings of hopelessness or worthlessness
Lack of social support (wouldn't leave children)
With the right support and treatment, individuals with mood disorders can find relief and live fulfilling lives (most people who have mood disorders do not die by suicide)
Over the last 3 months, Jay has not felt like their usual self. They are no longer interested in socializing and they take little pleasure from activities they used to enjoy. They have difficulty sleeping and eating. Jay appears to meet criteria for:
MDD
For the last week, Chandra has been irritable and on edge. She has not been sleeping more than two hours per night and has been flying into fits of rage when anyone suggests she sleep. She says she’s working on a project that will change the course of human history. Chandra’s symptoms are most consistent with
Bipolar 1
Anorexia Nervosa
Dietary Restrictions that lead to low body weight - severity is based on weight
Intense fear of weight gain, becoming fat or behaviors that interfere with weight gain
Disturbed perception of body
or undue influence of body in self-evaluation
or denial of seriousness of low weight
Restrictive vs binge purge type
Subtypes of Anorexia Nervosa
Restrictive: (AN-R)
Restrictive eating as a hallmark
Absence of regular bingeing or purging
Compulsive exercise is common
Binge-purge type (AN-BP)
Recurrent bingeing AND OR recurrent purging
Issues with BMI Criteria
Weight/BMI is an important factor as very low weight is medically dangerous, BUT this is only one factor in severity
Rapid weight loss can be very unhealthy, even if BMI is still in "normal”
range
Using weight as the primary measure of severity can delay diagnosis, discourage treatment, and overlook serious cases
Many individuals with eating disorders do not receive help because they “don’t look sick/thin enough”
Those in larger bodies may even be praised for weight loss, reinforcing disordered behaviors
What are better approaches to only using BMI criteria
Assessing physical symptoms (heart rate, electrolytes)
Asses psychological distress
Asses behaviors
binge/purge frequency should be considered as ________ can cause cardiac failure and death
electrolyte imbalances
Bulimia Nervosa
Recurrent binge eating (1 time or more a week for three months)
Recurrent inappropriate compensation: laxitives, fasting, vomiting, excessive exercise after a binge
Overevaluation of shape and weight – self-image is connnected to weight
AN criteria not met (weight) - difference is the weight category, typically heavier than AN bc of binging
Often restrited eating outside of binging
Clinical binge and three essential parts of a binge
Clinical binge: eating a unusually large amount of food within a two hour period (at least two or more meals in a very short period of time – high fat or calories)
often start when you try and eat a small amount of a cheat food and then physically cannot stop (sometimes people schedule their binges
I've had a hard day I am going to go home and binge)
Time Frame
Quantities
Loss of Control
Binge Eating Disorder
Just the binge part of Bulimia Nervosa
Recurrent binge eating episodes – at least once a week for three months
Marked distress about binge eating
No recurrent inappropriate compensation
Associated Risks with Eating Disorders
Mortality – Highest of all psych disorders
Suicide is the most common cause of death, followed by cardiac arrest
Cardiac problems – Electrolyte imbalances, prolapse, reduced muscle mass, slowed heart rate
Dental problems
Anemia
Comorbid psych disorders
Prevalence of eating disorders in men
Around 25% of individuals with eating disorders are men, though under diagnosis is common
Men are less likely to seek treatment due to stigma and misconceptions
Differences in presentation of Eating Disorders in Genders
More likely to focus on muscle gain, leanness, and control over physique – fine line in athletics
Especially true in gay community and athletes
Gay and bisexual men: 7x more likely to develop an ED
Body Dysmorphic Disorder with Muscle Dysmorphia Specifier (obsession with muscularity) is more common in men
May engage in excessive exercise, supplement use, and rigid dieting
Barriers to treatment
Social stigma-eating disorders are seen as a "female issue"
Medical professionals may overlook symptoms in men
Less research and targeted treatment approaches for men with EDs
Sociological factors and diet culture
Idealization of a slim body type as the epitome of beauty, particularly among North American white women*
Fat-phobia
People with larger bodies are frequently depicted in a negative light, if represented at all in the media
employment discriminations
Healthcare Bias: Individuals with higher body weight face discrimination from medical professionals
Media and Advertising
Health and fitness culture - emphasis on aesthetics rather than health
Nutrition and exercise goals often based off of staying slim and lean
Cultural and social rewards
Why does dieting have a counter effect on the dieter
(they aim to lose weight and then the opposite effect occurs)
Food restriction can lead to subsequent food obsession, binge eating, and rapid weight gain
Restraint of eating increases the risk of loss of control overeating, thereby undermining dieting efforts (Polivy and Herman, 1985)
Dieting can impair cognitive functioning, which makes effective decision-making regarding food choices more challenging
Adolescent girls who diet have 18 times the chances of developing an ED within:
6 months
Language that disguises eating and dieting as health or wellness related
Intermittent Fasting
Clean Eating – there aren't acc clean vs dirty just different kinds
Detoxes and Cleanses - “toxins” what are these toxins
Keto, Paleo, Low-Carb
“Mindful Eating” Apps – contains a lot of diet culture
Biological factors of ED
Twin studies on AN and BN provide strong evidence for a genetic component in eating disorders
Key Findings from Twin Studies:
Anorexia Nervosa: ~50-80% heritable.
Bulimia Nervosa: ~50-60% heritable.
Higher Concordance in Monozygotic (Identical) Twins than in Dizygotic (Fraternal) Twins
Genetic factors contribute to personality traits linked to EDs (e.g., perfectionism, impulsivity, anxiety)
Developmental contributions to ED
Parental attitudes and modelling around food, weight, and body image
High control or enmeshed family relationships may contribute to restrictive eating
Criticism or pressure regarding weight/appearance increases risk
Trauma and Abuse: Trauma survivors may develop eating disorders due to shame, negative body image, and/or as a way to cope
Restriction may create a sense of control or emotional numbness
Bingeing may provide temporary emotional relief
Some may try to manipulate their body size to feel safer or avoid
attention
Peer pressure and comparison culture, especially during adolescence
Emotional and personality factors of an ED
Personality:
Perfectionism – High self-expectations, fear of failure/criticism/rejection
Anxiety sensitivity – Avoiding risk, strong need for control, obsessiveness
Impulsivity - more common in bulimia/binge-eating disorder
Emotional Regulation Difficulties:
Difficulty coping with distress
Restriction = emotional numbing; bingeing = emotional escape
Cognitive patterns in ED
Black-and-white thinking about food, weight, and self-worth
Distorted perception of body image
Low self-esteem and identity struggles
Barriers to help in ED
Functions being served by the eating disorder may deter help-seeking EG; emotion regulation, trauma avoidance, social reward
Shame and denial common deterrents
Barriers related to access
Using CBT to treat ED
Phobias, OCD have similar treatments
Exposure is necessary
Weight restoration
Eating fear-foods
Regular eating schedule
Moderate exercise
Mindfulness/DBT (DBT has skill building components like emotion regulation skills)
Other factors to consider - The development of:
New ways of coping with emotional distress
Identity outside of the eating disorder
More compassionate ways of relating to one’s feelings and body
Social circles with positive culture around food and body image
Sleep occurs in repeating cycles, progressing through different ______ and ____ stages
REM and non-REM
What is a sleep cycle and what are the stages
Each cycle lasts approximately 90 minutes, with multiple cycles per night
Stage 1 and 2: You first fall asleep, but are not yet in a deep sleep
Stage 3 and 4: You are in a deep, restful sleep your heart rate and breathing slow and your body is still
1-4 = nonREM
Stage 5: Your brain is active and your dreaming, your eyes move under your eyelids in REM
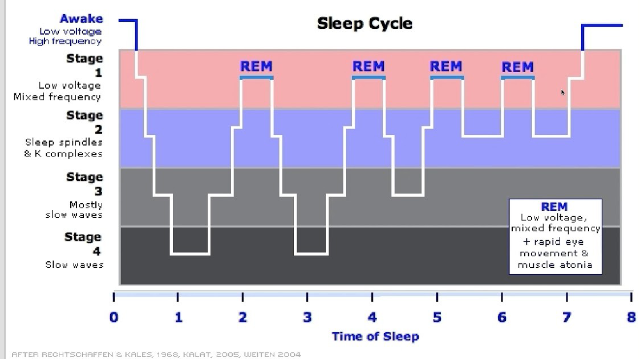
The first half of the night has what
More deep sleep (stages 3 and 4)
REM becomes longer and more frequent in later cycles
What is different about stage 4
Stage 4 disappears after the first few cycles, while REM dominates toward morning
If you go to bed late (~12pm) your body will prioritize REM sleep and you won’t get as much deep sleep which is important for physical recovery
Why if you go to bed late you have crazy dreams
Your body physically restores itself in the first half
Why is REM sleep important
crucial for memory consolidation and emotional processing
You are filing away emotions and experiences which is often why you have nightmares
Why do we sleep - restoration theory
Suggests sleep is essential for repairing and rejuvenating the body and brain. It helps in muscle growth, tissue repair, and protein synthesis.
Evolution theory
Proposes sleep evolved as a survival mechanism:
It conserves energy (don’t need to eat or drink or stress) and protects individuals from predators during parts of the day when there's little value or danger in being awake.
It preserves energy so we don’t need to eat as much as well. Exposed to more risks (conservation)
Information conservation theory
Sleep plays a crucial role in processing and consolidating memories from the day.
It strengthens neural connections and supports learning and memory formation.
Waste Clearance theory
(Glymphatic System)
Sleep facilitates the clearance of waste products from the brain, including toxins associated with neurodegenerative diseases (e.g., dementia), through the glymphatic system.
We deal with our fears and phobias in different contexts through dreams
What are some of the effects of Sleep Deprivation
Impaired Immune System
Severe yawning
Hallucinations
Symptoms similar to ADHD
Risk of Diabetes type 2
Increased heart and risk of heart issues
Decreased time reaction
Tremors
Aches
Growth Suppression
Obesity
Decreased temp
What happens when you loose sleep for even one night
lead to deficits equivalent to having a blood alcohol concentration of 0.1%, which is above the legal limit for driving in many jurisdictions
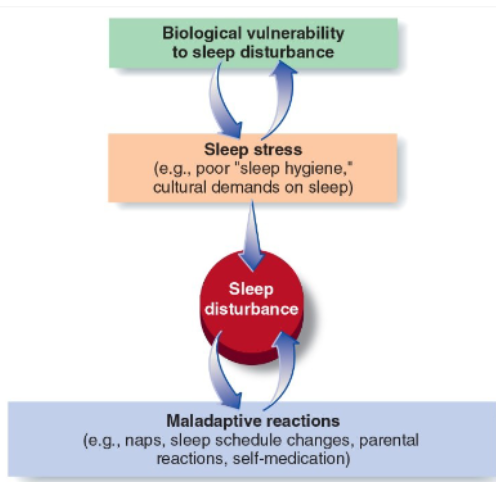
What are the three main factors of sleep disturbance
Biological Vulnerability to sleep disturbance
Sleep stress (poor sleep hygiene, cultural demands)
Maladaptive reactions (someone reacting to stress making it worse): Naps, sleep schedule changes, parental reactions, self-medication)
Sleep-Wake disorders
Dyssomnias – difficulties getting enough sleep, problems in the timing of sleep, and complaints about the quality of sleep
Insomnia Disorder
Hypersomnolence Disorder - being too sleepy
Narcolepsy - falling asleep during the day
Breathing-Related Sleep Disorders (apnea)
Circadian Rhythm Disorders
Parasomnias – abnormal events that occur during sleep
Nightmare disorder, sleep terrors, sleep-walking
Dyssomnias
Any type of sleep disturbance: Difficulties getting good quality sleep - people often develop maladaptive reactions
Insomnia disorder
Hypersomnolence disorders
Narcolepsy
Breathing-related sleep disorders
Sleep apnea
Circadian rhythm sleep-wake disorders
Insomnias
Dissatisfaction with sleep quantity/quality associated with at least one of the following difficulties:
Initiating sleep; or
Maintaining sleep (frequent awakenings); and/or
Early morning awakenings with inability to return to sleep
Clinically significant distress/impairment
Occurs at least 3 nights/week for at least 3 months
Occurs despite adequate opportunity for sleep
Insomnia doesn’t mean not sleeping at all. Problem is experince of chronically unsatisfying sleep
CBT for sleep disorders
Individualized treatment outlining triggers and thought processes. Without needing medication. It focuses on changing negative thoughts, emotions, and behaviors that keep people from sleeping well.
Keeping journal
Improve sleep hygiene
Changing ideas about sleep
Medications for sleep disorders
Sedative and or benzodiazepines
Can cause dependance
Rebound insomnia
Temporary worsening of sleep problems that happens after stopping sleep medication or certain substances like alcohol or drugs.
Is melatonin good?
Only if you only need help getting to sleep initially (doesnt help sustained sleep)
People with insomnia are more likely to
Have distorted perception of sleep length and sleep quality
Experience increased intrusive worries when they try to sleep
Endorse unhelpful, negative beliefs about sleep:
Unrealistic expectations
Catastrophizing
Endorse positive meta-beliefs about benefits of worrying in bed
Try to conserve energy during waking hours (e.g., cancel appointments, avoid exercise, avoid social events, etc.)
Things that help sleep hygiene:
Stick to the same bedtime and wake up time, even on the weekends.
Practice a relaxing bedtime ritual.
Avoid naps, especially in the afternoon.
Exercise daily.
Design your sleep environment to be conducive to sleeping.
Sleep on a comfortable mattress and pillows.
Use bright light to help manage your circadian rhythms.
Avoid alcohol, cigarettes, and heavy meals in the evening.
Wind down. Your body needs time to shift into sleep mode, so spend the last hour before bed doing a calming activity such as reading.
If you can't sleep, go into another room and do something relaxing until you feel tired.
Disorders that develop after a stressful or traumatic life event includes:
Post-traumatic stress disorder (PTSD)
Acute stress disorder
Adjustment Disorder
NEW Complex PTSD
PTSD
Emotional disorder one month after a traumatic incident:
War
physical/sexual assault, particularly rape
Car accidents
Natural catastrophes
And more
Criterion A stressors
Exposure to actual or threatened death, serious injury, or sexual violence through:
Direct exposure
Witnessing the trauma
Learning that the trauma happened to a close relative or close friend
Indirect exposure to aversive details of the trauma, usua;;y in the course of professional duties (eg. therapists, first responders)
PTSD - Re-experiencing
nightmares, intrusive memories, flashbacks
A car accident survivor hears a car horn and suddenly feel as though they are back in the crash
A sexual assault survivor experiences sudden distressing memories when seeing someone who resembles the assailant
Avoidance - PTSD
Avoidance of the intense feelings or reminders of the event through emotional numbing, avoiding people/places/circumstances
A domestic violence survivor avoids dating or forming close relationships because intimacy reminds them of past abuse
A first responder who witnessed a tragic event at work starts avoiding certain parts of town where it occurred
Negative changes to mood/cognition and reactivity in PTSD
Negative changes to mood/cognition: these symptoms affect thoughts, emotions, and beliefs about oneself, others, and the world
A police officer feels emotionally detached and unable to feel joy, even in positive situations
Reactivity: disturbed sleep, hypervigilance, increased startle response
A shooting survivor jumps or panics when hearing fireworks or loud noises
A first responder entering room and surveilling the whole thing, or not allowing their kids to do the whole thing
Specifiers in PTSD: Delayed expression
Additional information added to the diagnosis
Delayed expression: PTSD symptoms do not fully appear until at least 6 months after the event
WHY? Some individuals suppress or disconnect from the trauma until a trigger (eg. life stress, new trauma) brings symptoms to the surface
Trigger onset may be a lack of distraction (eg. retirement)
Dissociative, Depersonalization, Derealization
Not a single disorder but a symptom that may appear in various disorders:
Dissociation: a disconnection between thoughts, memories, identity, emotions, and perception of reality
Dissociation is a coping mechanism that helps survivors manage extreme distress or overwhelming emotions
Ranges from normative (eg. daydreaming, zoning out) to disordered
Depersonalization: feeling detached from oneself (“I feel like I’m watching myself from the outside”)
Derealization: Feeling like the world isn’t real (“everything looks foggy or dreamlike”)
PTSD Causes:
Anxious predisposition (makes it more likely)
Intensity and severity of trauma
Resnick et al. (1993) found that likelihood of developing PTSD increased as a function of the severity of the trauma
Most likely to get PTSD
both life threat and injury, then injury only
Least likely to get PTSD: no life threat of injury, life threat only
Stress changes in the brain from PTSD
Overactive amygdala: excessive fear responses, hypervigilance, and emotional dysregulation
Shrinking in hippocampus: flashbacks, memory gaps, difficulty separating past/present
These brain changes explain why PTSD patients feel “stuck” in their trauma and react strongly to reminders
Lack of social support with PTSD
Talking about traumatic events help file them away
Neuroplasticity in PTSD
Trauma causes the brain to:
Strengthen fear pathways in the amygdala
Weaken memory regulation in the hippocampus
➔ This can help or harm us, depending on the situation
Repeated stress keeps fear circuits active, making emotional regulation harder
Avoidance behaviours reinforce these brain changes by:
Preventing the brain from reprocessing traumatic memories
Confirming that the fear is justified and as scary as we believe
Imaginal Exposure with Relaxation Training
Clients mentally revisit traumatic events in a safe setting while practicing relaxation techniques (eg. deep breathing)
Helps reduce avoidance, desensitize emotional distress, and reprocess trauma
Eye movement desensitization and reprocessing (EMDR)
Dont know why it helps but it does
Clients recall traumatic memories while following bilateral stimulation (eye movements, tapping)
Helps the brain reprocess trauma and reduce emotional intensity
Biological Treatments in PTSD
SSRIs: regulate brain’s overactive fear response and mood alterations
Repetitive Transcranial Magnetic simulation
Repetitive Transcranial Magnetic Stimulation
(RTMS): magnetic pulses stimulate underactive brain regions associated with PTSD symptoms
Strengthens connections between the prefrontal cortex (thinking brain) and the amygdala (fear center) to improve emotional regulation and reduce hyperarousal
Acute Stress Disorder
occurs up to 1 month after a traumatic even
Can be short-term PTSD precursor
May resolve and not lead to PTSD, but is a significant risk factor (40-80%)
Adjustment disorder
emotional and/or behavioural reactions to life stress (divorce, job loss, move) that is out of proportion to the stressor
May include depression, anxiety, and conduct problems (eg. aggression, rule breaking)
Complex PTSD
NOT currently recognized in DSM-5-TR, but IS in the ICD-11
Caused by prolonged exposure to traumatic events, often interpersonal in nature, such as long term abuse
Includes the symptoms of PTSD plus:
Emotion dysregulation
Interpersonal problems
Complex changes in self-concept (eg. feeling “othered”, lacking identity)
Impact on relationships: problems with trust, intimacy, and a tendency to avoid relationships or to seek out unhealthy relationships
Treatment for Complex PTSD
may require longer-term psychotherapy that focuses not only on coping with traumatic memories but also on improving emotional regulation, self-concept, and relationship skills (eg. DBT)