Ischaemia, Oedema and Heart Failure
1/54
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
55 Terms
Define haemorrhage
Escape of blood from the vascular system.
(can be overt i.e. trauma or internal ; acute/chronic)
Define diapedesis
The ability of a WBC to cross into a capillary through the wall.
Define extravasation
The movement of white blood cells from the capillaries to the tissues surrounding them
Define haematoma
A solid swelling of clotted blood within the tissues.
Define rhexis
Rupture of a vessel.
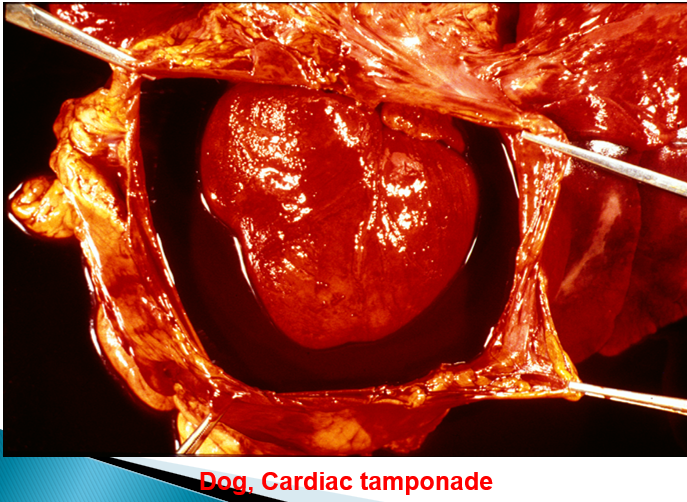
What is a cardiac tamponade?
Compression of the heart via an accumulation of fluid in the pericardium leading to diastolic filling defects.
What are petechial hemorrhages?
Small haemorrhages (1-2mm clots).

What are purpural haemorrhages?
Small-ish haemorrhages (>3mm clots).
What are ecchymoses?
Large haemorrhages (>1-2 cm clots).
How is the anatomical location of a haemorrhage named?
Haemo-[anatomical location]
List at least 3 causes of haemorrhage
physiological
trauma
parasites
bacteria
viruses
toxic agents
clotting deficiencies
neoplastic disease
agonal (as the animal is dying)
Why do agonal haemorrhages occur?
As the heart stops, blood will pool in capillaries which may lead to haemorrhage
What are the outcomes of haemorrhage?
Haemorrhagic (hypovolaemic) shock
Complete recovery
Loss of function
Iron-deficient anaemia
How is haemoglobin degraded?
By macrophages:

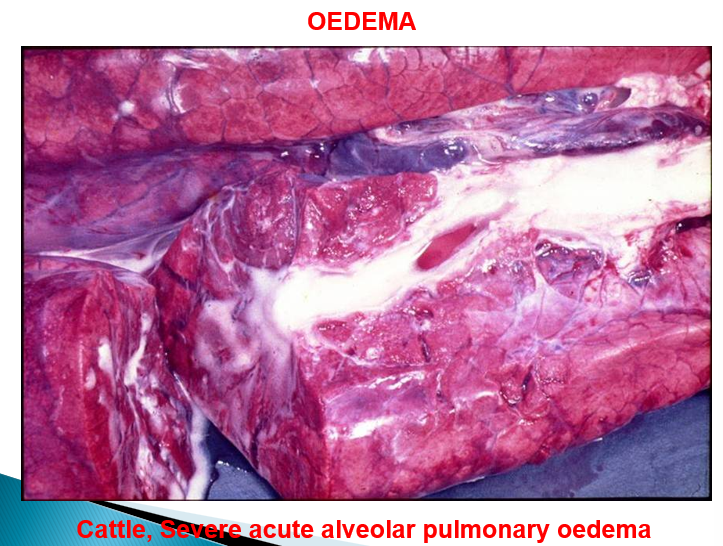
What is oedema?
Fluid accumulates in intercellular tissue space and / or in body cavities from blood.
What is oedema a result of?
Imbalance of forces which are responsible for transudation (with normal capillary permeability).
increased vascular permeability associated with inflammation
fibrinous / purulent exudates
How does non-inflammatory oedematus transudate look?
Colourless fluid (low protein content).
How can impaired venous return cause oedema?
Increases hydrostatic pressure in venous vasculature leading to NET filtration into the ECF from veins.
How can chronic protein loss lead to oedema?
Reduces plasma oncotic pressure and hence NET filtration into ECF from vasculature.
How can lymphatic obstruction lead to oedema?
Fluid in ECF is not absorbed normally and hence builds up instead of being removed.
What is a common cause of increased hydrostatic pressure in vasculature?
Heart failure.
What is a common cause of decreased plasma proteins and hence decreased plasma oncotic pressure in vasculature?
Malnutrition.
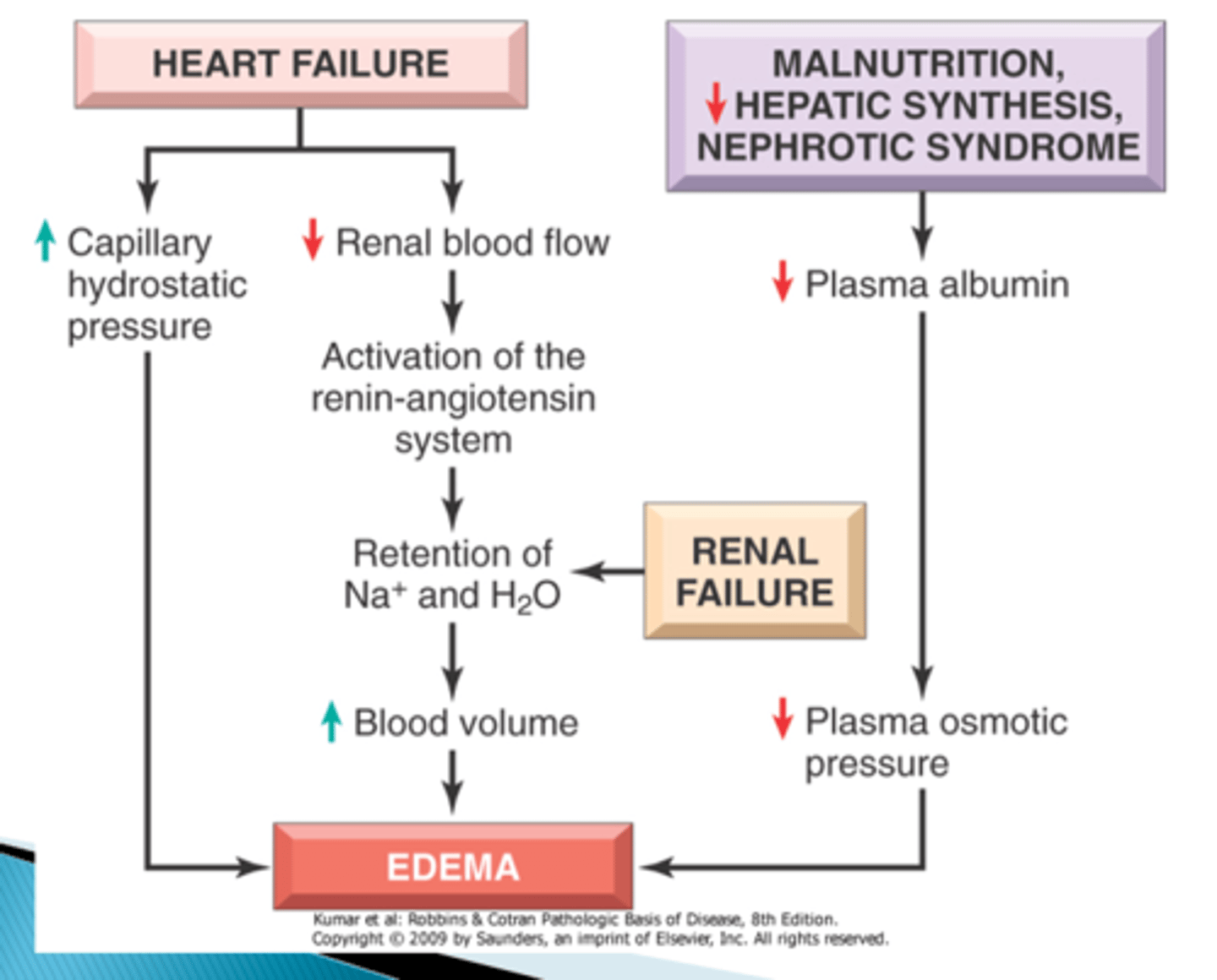
How can sodium retention cause oedema?
Due to diseased renal system leading to increased tubular Na+ reabsorption
Which diseases are characterised by oedema?
cardiac disease - heart failure
chronic liver disease - ↓ protein synthesis
renal disease – protein loss
chronic parasitism – protein loss
protein-losing enteropathy
Define hydrothorax
Fluid in the pleural cavity.
Define hydropericardium
A build up of fluid in the cardiac cavity, the area around the heart (pericardium).
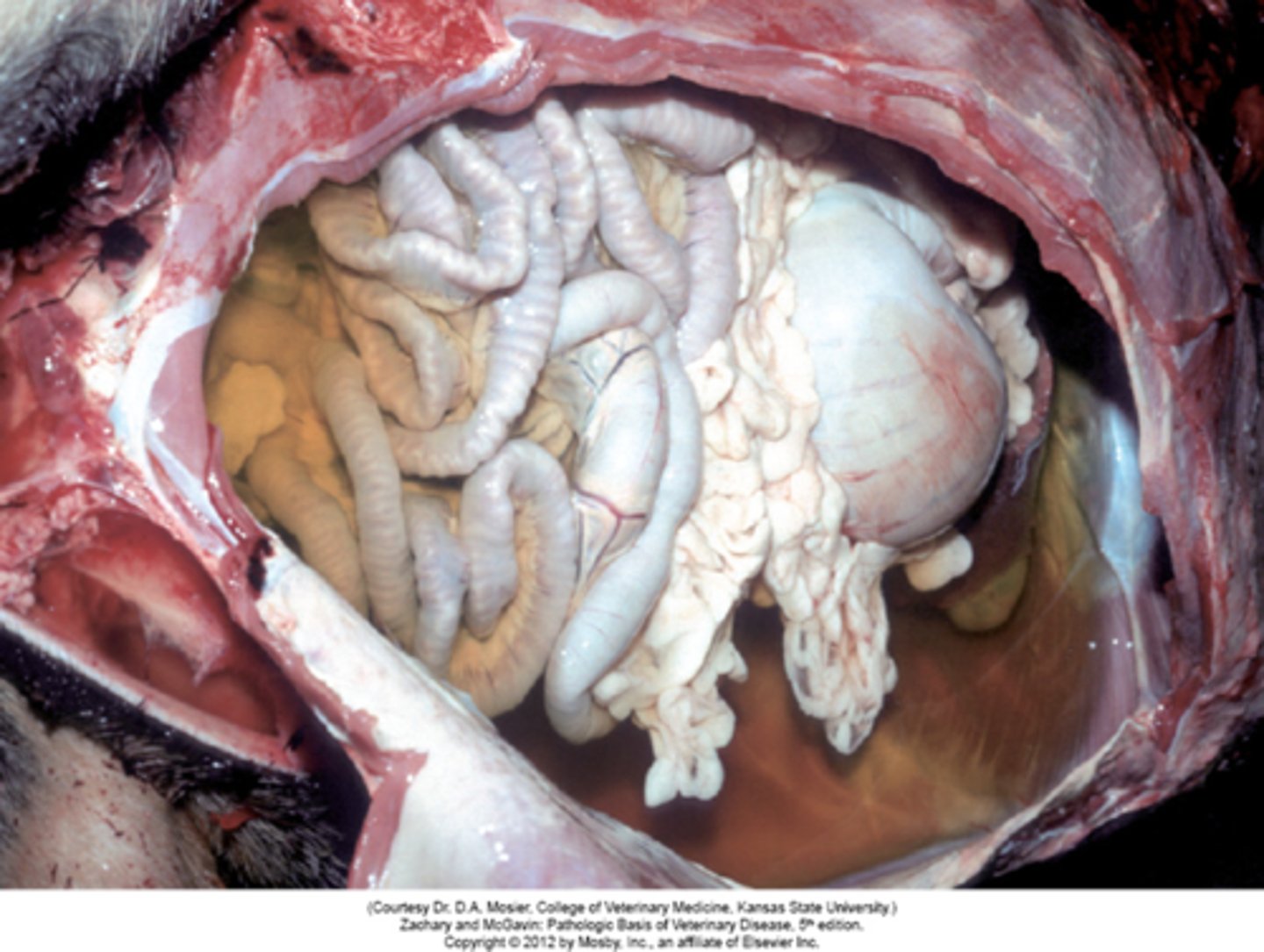
Define ascites
The accumulation of fluid in the peritoneal cavity, causing abdominal swelling.
Define anasarca
Extreme generalised oedema.
What are the main types of oedema?
Localised and generalised (at species predilection sites).
Where is it common to see oedema in a dog?
Peritoneal cavity.
Where is it common to see oedema in a cat?
Thoracic cavity
Where is it common to see oedema in a sheep?
Submandibular space or perioneum.
Where is it common to see oedema in a horse?
Limbs.
Where is it common to see oedema in a cow?
Brisket oedema (subcutaneous oedema)

Describe Bottle Jaw
Subcutaneous, sub-mandibular oedema
Seen in sheep, goats, cattle
Usually caused by hypoproteinaemia

List at least 2 specialist forms of oedema
pulmonary oedema
oedema of the brain
glaucoma
Give at least 2 causes of pulmonary oedema
Left sided congestive heart failure —> passive hyperaemia.
Irritant gases
Inflammation
Toxic e.g. Fog Fever
Agonal change
What is heart failure?
Develops slowly from gradual loss of pumping efficiency, associated with pressure or volume overload or myocardial damage
Heart cannot pump blood at rate needed by the tissue (or can do so only from an elevated filling pressure).
How does the cardiovascular system maintain arterial pressure and perfusion?
Increased preload of dilation —> sustaining of cardiac performance by enhancement of contractility
Myocardial hypertrophy (± chamber dilation) —> increase of mass of contractile tissue
Activation of neurohormonal system —> release of noradrenaline, activation of renin-angiotensin-aldosterone system, release of atrial natriuretic peptide
Why does myocardial hypertrophy occur?
In response to abnormal intra-atial/ventricular pressure increases.
What is congestive heart failure?
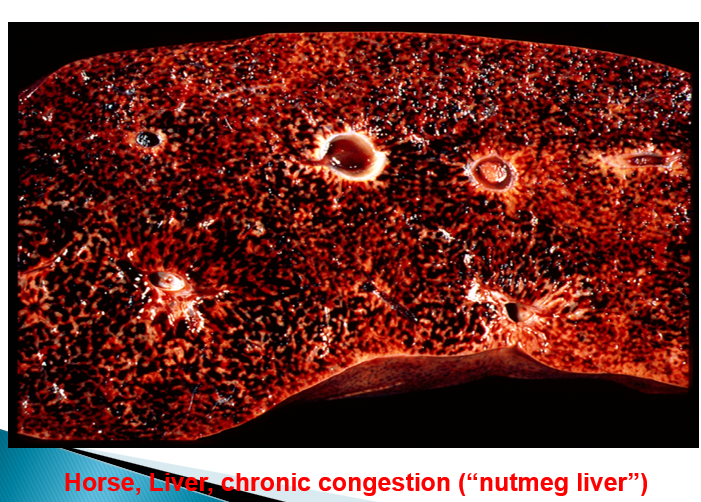
Build-up of venous blood in systemic and pulmonary circulation.
What are the causes of congestive heart failure? Which one causes forward heart failure? What about backwards?
Due to reduced cardiac output and underperfusion (forward)
Due to increased venous pressure (backward)
Give at least 2 consequences of congestive heart failure
a) oedema, tissue hypoxia
b) activation of renin-angiotensin-aldosterone system
c) chronic congestion of lungs and liver
d) fluid accumulation in peritoneal and/or thoracic cavity
What is the difference between left and right sided heart failure?
Depends on the location of the lesion (e.g. if it is the left AV valve affected only, it is left-sided heart failure).
What are the effects of left-sided heart failure on the lungs and kidney?
consequences on lungs – pulmonary congestion and oedema
consequences on kidneys – hypoperfusion → renin etc
What are the effects of right-sided heart failure?
(cause: pressure overload of right ventricle)
usually sequel of left-sided heart failure
increased resistance within pulmonary circulation
consequences on liver, body cavities, subcutaneous tissue
How is the heart itself effected in heart failure?
Cardiac hypertrophy:
Concentric = due to pressure overload meaning the heart wall must thicken
Eccentric = due to volume overload (e.g. due to leaky valves) and the actual size of the chambers increase
What are the roles of angiotensin 2 in the body?
Constricts arteriolar walls
Increases strength of heart beat
Increases sodium retention in kidneys
Increases aldosterone release to increase Na reabsorption
What is the role of ADH with respect to lowered blood pressure?
Causes increased reabsorption of water from the kidneys.
What is the effect of noradrenaline on the heart?
Increased HR, myocardial contractility
What is the function of atrial natriuretic peptide?
Counteraction of renin-angiontension-aldosterone system:
relaxation of vascular smooth muscle (decreased BP) inhibition of Na+ reabsorption in kidney, increased glomerular filtration, increased glomerular filtration, inhibition of aldosterone secretion
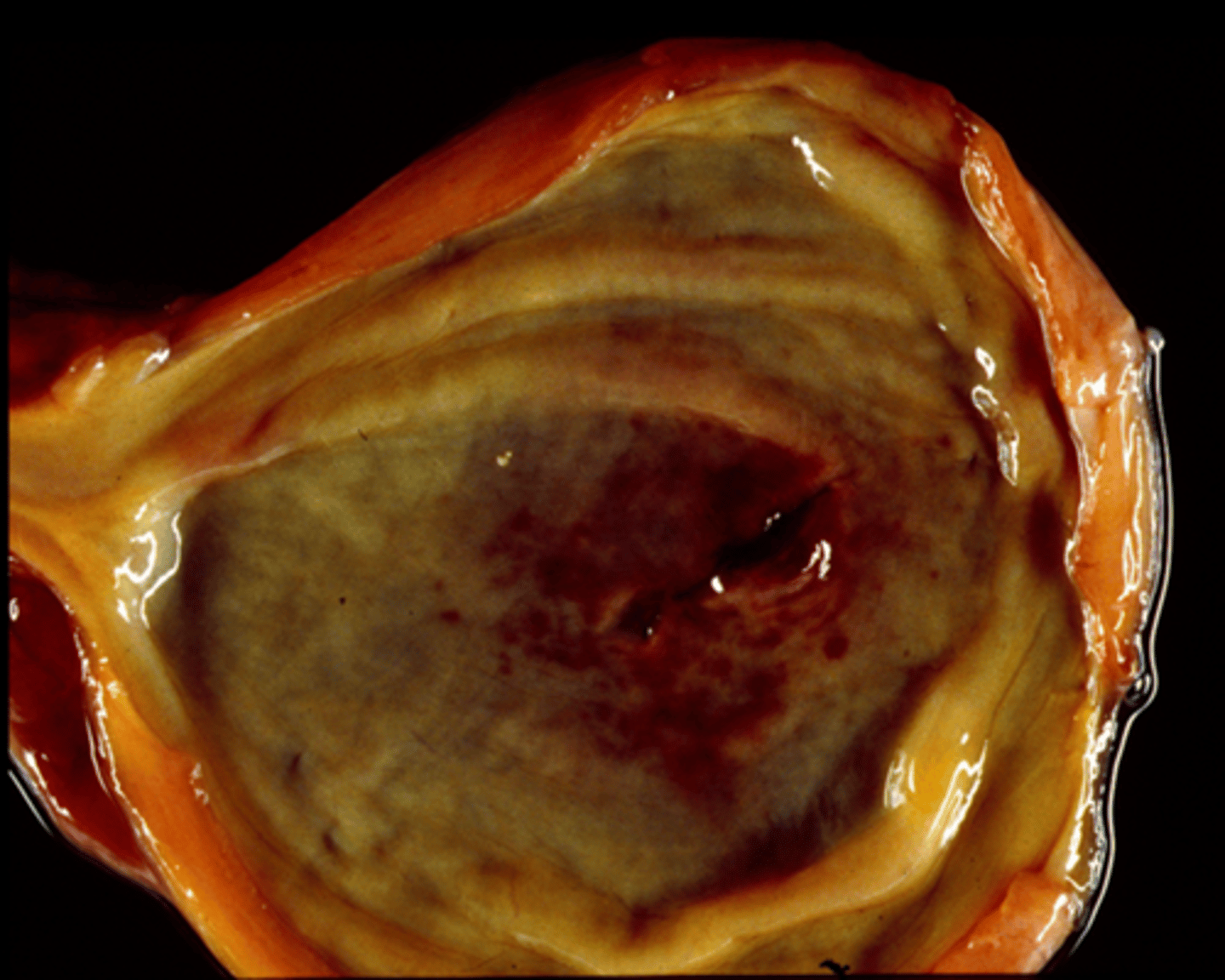
What is “nutmeg liver” caused by?
Right sided congestive heart failure —> passive congestion from central vein
What is the most likely outcome of chronic low-level haemorrhage e.g. blood-feeding parasite?
Iron-deficiency anaemia
Which myocardial change is induced by volume overload?
Eccentric hypertrophy
During heart failure, which hormone is secreted by the kidney which activates a homeostatic mechanism and exacerbates the heart failure?
Renin