Week 8 Anatomy and Physiology 2 ELIzabeth's
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
63 Terms
Understand the functions of amylase, lipase, proteases, and brush border enzymes.
Amylases: (complex sugars/starch)
-Salivary amylase in mouth
-Pancreatic amylase in pancreas
Lipases: (fats)
-Salivary lipase in mouth
-Gastric lipase in stomach
-Pancreatic lipase
Proteases (protein):
-Pepsin in stomach
-Trypsin, chemotrypsin in intestine but is made in pancreas
Brush border enzymes:
-Others break really big into smallish
-These break smallish into monomers
Describe the extent to which digestion and absorption occur in the oral cavity
-This is where digestion begins
-mechanical digestion (mostly): Food crushed and ground into smallish chunks (chewing)
-Limited chemical digestion of carbohydrates and lipids:
-Salivary amylase: works immediately, inactivated by low pH
-Salivary lipase: Doesn't work in mouth, activated by low pH
Describe the extent to which digestion and absorption occur in the stomach
-Hydrochloric acid denatures proteins and has some breakdown of carbohydrates and breaking of plant cell walls
-In acid, pepsinogen becomes pepsin; proteins are broken down into long peptides
-Salivary and gastric lipases break down triglycerides into fatty acids (but only on outside of fat droplets)
Summarize the process of hydrochloric acid secretion.
-Done by the parietal cells
-Seperate release of H+ and Cl-, plus a thick mucus layer, means that cells are not exposed to acidic enviornment
Acid:
-Converts pepsin
-Denatures proteins
-Breaks down plant cells
-Kills most microbes
What controls the digestive system?
Neural mechanisms:
-Parasympathetic and local reflexes (like the stretch reflex which is where stretching triggers contractions)
Hormonal mechanisms:
-Enhance or inhibit smooth muscle contraction
Local mechanisms:
-Coordinate response to changes in pH or chemical stimuli
Summarize the cephalic phase of stomach function
-Cephalic means head
-This is a sensory input stage, it prepares the stomach to receive food
Effect:
-Parasympathetic impulses
-Gastric secretion increases (HCl, Mucus, Pepsinogen)
-Hormonal secretion of gastrin (triggers other cells of the stomach to secrete stuff)
-Some increase in peristalsis (stomach growling)
Summarize the gastric phase of stomach function
-Stretch receptors triggered as stomach fills (oh btw no amylases are active in the stomach)
-Causes motility of walls (increased secretion, gastric churning)
-Stimulates all secretory cells (HCl, digestive enzymes)
-Gastrin increases secretion and motility
-Creates chyme: liquid, partially digested food
-This phase lasts for an hour or two.
Summarize the intestinal phase of stomach function
-Enterogastric reflex: lowered stretch receptors, chemoreceptors stimulate:
1. Inhibit vagal stimulation
2. Inhibit myenteric reflex
3. Pyloric valve opens spasmodically (so you don't get a whole bunch of acid in the intestine at once)
-Acidity and nutrients in chyme trigger endocrine cells in the small intestine:
-CCK (inhibit stomach function, secretions, muscular action, also speeds up chyme coming into small intestine)
-gastric inhibitory peptide
-Secretin
Describe the role of Gastrin
-Increases secretion and motility, triggers other cells of stomach to secrete stuff.
Describe the role of CCK and secretin in the activity of the stomach, liver/gall bladder, pancreas, and intestines
Essentially what they do is increase chyme speed, turning off stomach, turning on intestines
-Lower stomach activity (in stomach)
-Increases secretion of bile (triggering smooth muscle contraction of gall bladder), as well as pancreatic juice
-Reduces hunger
Describe the role of VIP and GIP
VIP (vasoactive intestinal peptide):
-Vasodilation of intestinal capillaries, which allos for more blood flow and this allows for:
-Increased nutrient absoprtion
GIP (Gastric inhibitor peptide)
-Inhibits gastrin, stimulates insulin
What are enteroendocrine cells
Secrete digestive hormones in response to chyme as well as pH, stretch reflex, peptides, lipids. It includes Secretin, CCK, VIP, GIP
Explain the function of the pancreas in relation to digestion
1. Pancreatic juice:
-Mostly water
-Sodium bicarbonate-buffer
-Enzymes
2. Whatever we eat, pancreas has an enzyme for it
-Pancreatic amylase
-Pancreatic lipase
-Ribonuclease and deoxyribonuclease mixture
-Poteolytic enzymes (proteins)
-Trypsin (secreted as trypsinogen)
-Chymotryspin (chymotrypsinogen)
-Carboxypeptidase (procarboxypeptidase)
-Elastase (proelastase)
-All are secreted in an inactive form and trypsin is the major protein one that is released as it activates the other ones. It is important that the proteases are inactive because we don't want to have the enzymes digesting our own protein.
Explain the regulation of pancreatic secretions
Neural control: Parasympathetic division of ANS via the vagus nerve
Autoregulation: low pH, Fatty acids, amino acids trigger release
Homronal control: Secretin and CCK
Explain small intestine motility and digestion
-Segmentation (circular muscle of s.m contracting) movements diffuse bolus and mix with digestive enzymes
-Movement in both directions (forward and backwards) slows the passage through jejunum and ileum, and mixes shit up
-Pendular movment (like a pendulum): Entire loop moves back and forth
-Spiral motion: Maximize time of contact between food, enzymes, and villi of intestinal wall
-Stimulated by gastric streching, chyme in duodenum, and enteric hormones
Explain intestinal juice and brush border enzymes and how they help with digestion in the small intestine
Intestinal juice:
-1-2L a day
-Contains water and mucus, slightly alkaline
-Doesn't contain a whole bunch of enzymes
-Keeps digestive enzymes and productsof digestion in solution
-Provide a liquid medium aiding in absorption
Brush border enzyme:
-Inserted into plasma membrane of absorptive cells
-Some enzymatic digestion occurs at surface rather than jsut in lumen
-Med. size to small/monomer
Describe the extent to which digestion and absorption occur in the large intestine (microbiome)
-No digestive enzyems made in large intestine
-BACTERIA DIGEST STUFF
-Convert bilirubin to sterobilin (brown pigment)
-Break down peptides:
-Ammonia
-Indole and skatole (aromatic)
-Hydrogen sulfide
-Break down indigestible carbohydrates
-Makes vitamin K which is needed for blood clotting
-The microbiome may help regulate weight, and insulin sensitivity, inflammation, and a bunch of other stuff
Explain the transport of water and ions through the intestinal wall.
-9 liters of fluid dumped into GI tract each day
-Small intestine reabsorbs 8 liters
-Large intestine reabsorbs 90% of that last liter
-Absorption is by osmosis through cell walls into capillaries inside villi
Explain the defecation reflex
1. Fecal matter held in rectum; stretch receptors activated
2. Short reflex loop:
-Triggers local persitalsis
-Feces moves from sigmoid colon to rectum, relaxes internal sphinctor
3. Long reflex loop
-Spinal reflex of parasympathetic NS
-Peristalsis from descending colon
4. Voluntary relaxation of external sphinctor
Explain the digestion of lipids
-Bile salts form micelles (lipid droplets)
-When the micelle gets broken down into monoglycerides they are diffused into the villi where they are reformed into tryglicerides
-Protein coat forms chylomicrons
-Then they go into lacteals, through lymphatic system and into teh blood.
-Does not go thorugh hepatic protal vein
Understand what is meant by gluconeogenesis.
Gluconeogenesis:
-Anabolic process
-Formation of glucose from proteins and fats
-When triglycerides break down, the glycerol becomes glyceraldehyde 3-phosphate which is in the steps to make glucose.
-Lactic acid as well as certian amino acids (proteins) can be converted into pyruvic acid which is used to create glucose
-The glucose can be secreted or can be stored as glycogen mostly in the liver.
-This process is stimulated by cortisol (long term stress), and glucagon
Understand what is meant by glycolysis
-IT is going to be when glucose is broken down into energy.
-Glycerol becomes glyceraldehyde 3-phosphate which helps create pyruvic acid and helps break down glucose
-Lactic acid and certain amino acids become pyruvic acid which then creates acetyl coA which helps break down glucose
-Stimulated by insulin and thyroid hormone
Describe the structure and function of the lipoproteins, including chylomicrons, VLDL, LDL, and HDL.
-Lipoproteins are single layer of phospholipids which are held together by apoprotiens.
-Chylomicrons form in the small intestine and enter the lymphatic system, then enter the blood when it gets to the liver it is turned into VLDLs (very low density lipoproteins).
-VLDLs: Produced by liver, transport lipids to the adipose tissue for storage, when the triglycerides are removed to be put into the adipose tissue, they become LDLs (low density lipoproteins) which contain mostly cholesterol
-LDLs: bad cholesterol (LDLs can deposit cholsertal where it shouldn't be causing fatty plaques in BVs). They carry 75% of total cholesteral in the blood. They deliver it to body cells for repair and synthesis and can be bad for the reasons I stated.
-HDLs (High Density lipoproteins): Good cholesteral. Remove excess cholesterol form body cells and blood, deliver them to the liver for elimination
Understand what is meant by lipogenesis, and lipolysis and beta-oxidation
-Lypolysis is breaking down trygliceride to make ATP.
-Fats can burn Lots of energy
-Beta oxidation is where every 2 carbosn on the fatty acid tail are turned into acetyl CoA which allows for energy to be made
-Glycerol can turn into glyceraldehyde 3-phosphate ending up with acytel Coa, and fatty acids, through beta oxidation can become Acetyl coa which goes into the kreb cycle to become ATP
-Lipogenesis is Lipid anabolism (building up of lipids), Glucose can turn into glyceral and then into tryglicerides. Certain amino acids can become acetyl coa which through beta oxidation can become fatty acids whcih can become tryglycerides.
Describe the relationship between protein catabolism and urea.
-Anabolism simply means protein translation btw.
-Protein Catabolism:
-Some amino acids enter kreb cycle
-Excess transformed to glucose or triglycerides
-But amino acids have nitrogen with them.
-So the amino acid goes through oxidative deanimation which becomes ammonia and keto acid. The ammonia in the liver is then broken down into urea which is less harmful and excreted out in urine through the kidneys.
What is leptin and ghrelin
-Ghrelin is produced by the cells in the gastrointestinal tract and that causes a feeling of hunger.
-Leptin is produced by adipose cells and suppreses hunger
Explain the major effects of insulin on its target cells.
-When blood sugar rises it trigggers insulin. There is a receptor on pretty mcuh all cells, and it tells cells to take up glucose to be turnewd into ATP, it also does this with lipids.
-Insulin will increase uptake of lipids, adn uptake of amino acids.
-Insulin will also increase the storage of glycogen as well as turn glucose into lipids through lipogenesis
Understand what causes the two types of diabetes mellitus.
Type 1: Pancreas doesn't make enough insulin and it is an autoimmune disorder
Type 2: Cells do not respond to insulin due to down regulation
Diabetes Mellitus causes:
-Elevated blood glucose
-Tissue starvation
-Blood vessel damage
-Nerve damage
Explain the primary effects of glucagon.
-Glucagon is released when blood glucose levels drop, it lowers absoprtion of glucose, lowering ATP production.
-It stimualtes lipids and amino acids to help form glucose
-Stimulates glycogen to turn into glucose
-Also causes adipose tissue to release lipids.
Know the basic effects of cortisol and growth hormone on metabolism.
-Decrease glucose uptake so that it can be saved for brain
-It will increase lipid uptake in cells
-It will cause lipids and amino acids to turn into glucose and then turn into glycogen.
Summarize the function of thyroid hormones on the body.
All we reall yneed to know is that it has a lot of functions and that it increases lipid and glucose utilization which increases basal metabolic rate.
Compare and contrast the absorptive and postabsorptive states.
-The absorptive state occurs for about 4 hours after food enters Small intestine. In the abosrptive state:
-Anabolism and energy storage will occur
-Glucose will be transformed to create ATP
-Liver metabolism: Amino acids deanimated and used for energy or stored as fat.
Postabosrptive:
-The state takes over until the next meal can be abosorbed
-Brain and spinal cord rely on glucose for energy; most other body cells can use fatty acids for energy
-Glucagon dominates, assisted by insulin antagonists (cortisol, TH, Epinephrine, hGH)
Steps;
-Catabolism and replacement of fuels in blood
-fatty acids and ketones, and glucose
-Amino acids are converted to glucose in liver.
Know what ketosis is, and what nutritional states are likely to cause it.
-Ketones are when carbohydrates aren't available, protein and fat must become acetyl coa in the liver. Buildup of acetyl coa in hepatocytes produces ketones (can be used for energy by cells as they can be converted back into acetyl coa)
-Ketosis is this process of turning the ketones into acteyl coa.
-Fasting, starving or high fat meal with few carbohydrates results in excessive beta oxidation adn ketone production.
List the organs of the urinary system and summarize the function of each organ.
1. Kidneys
-Primary functional organ
2. Ureters
-Drains from the kidneys
-Consists of mucosa, muscularis (smooth muscle which allows for peristalsis), and adventitia (containing blood vessels and nerves)
3. Urinary bladder
-Storage of urine
-Posterior to pubic symphesis, anterior to vagina and inferior to uterus; anterior to rectum
4.Urethra
-External tube
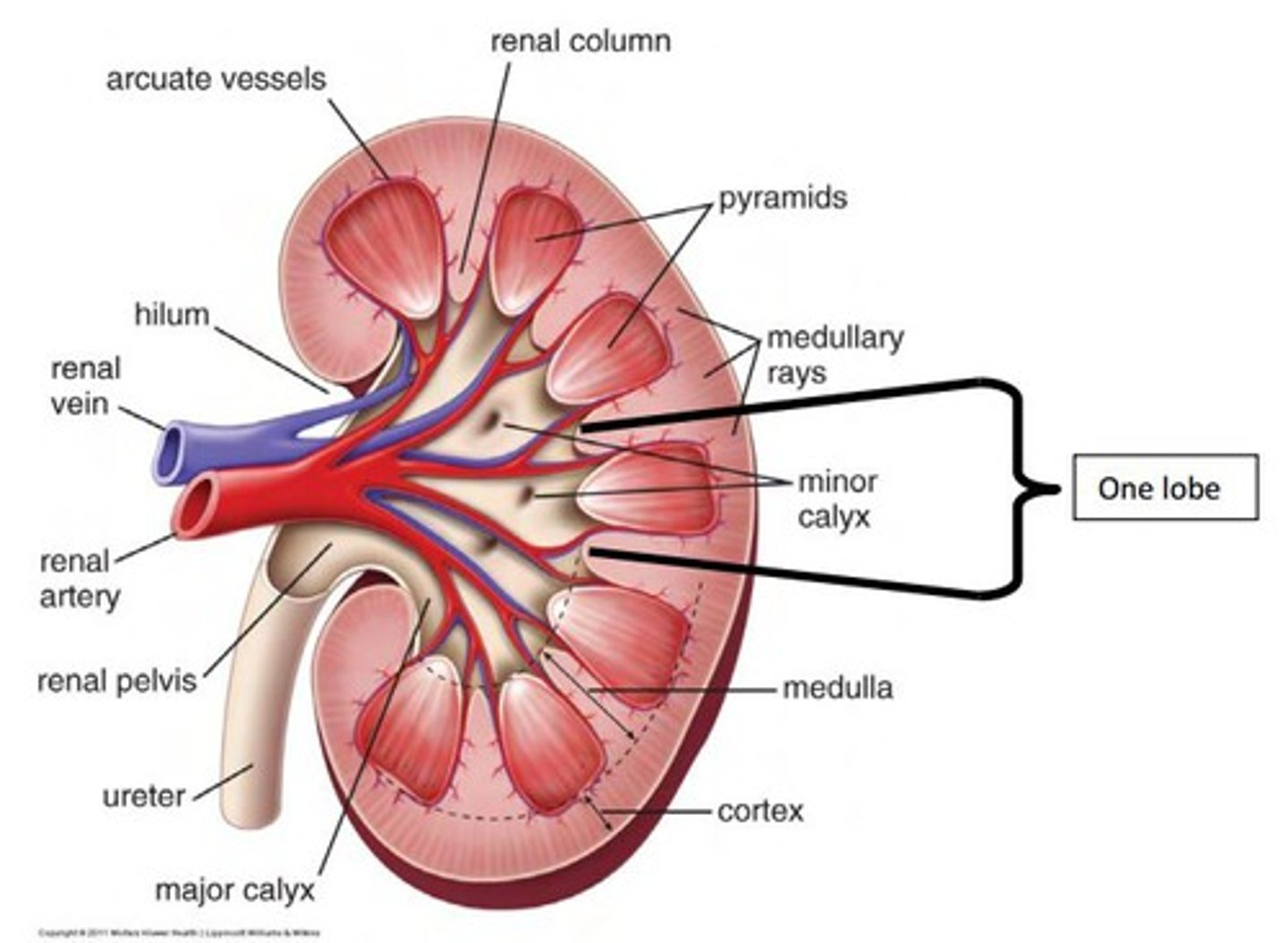
Illustrate the location of the following kidney regions: renal cortex, renal medulla, renal pyramid, renal pelvis, renal lobe
-Renal cortex: Superficial: Outer cortical zone and inner juxtamedullary zone
-Renal Medulla: Inner region
-Several cone shaped renal pyramids
Renal lobe: Renal pyramid, overlying cortex area, and 1/2 of each adjacent renal column
Know the location and purpose of the afferent and efferent arterioles, glomerulus capillary, and peritubular capillary, bowman's capsule (glomerular capsule).
Afferent arterioles: Bring blood into the glomerulus
Efferent arterioles: Bring blood away from the glomerulus to the peritubular capillary
Peritubular capillary: Capillary surrounding the renal tubules
Glomerular capillaries: Arries from afferent aretriole and form a ball before emptying into efferent arteriole
Bowmans Capsule: Where the filtrate goes into. where it then goes into the proximal convoluted tube
Diagram the flow of urine from the collecting ducts to the urinary bladder.
-Collecting ducts drain to minor calyx
-Minors join to beocme major calyx
-Major calyces become renal pelvis
-From the renal pelvis, urin trains into the ureters to urinary bladder and out of the body through urethra.
Explain the functions of the glomerulus, renal corpuscle and renal tubules
Renal corpsucle= Site of plasma filtration. THe glomerulus is capillaries where filtration occurs and the capsule collects filtrate
Renal Tubule: Includes the proximal convoluted tube, loop of henle which dips down into the medulla and distal convoluted tube
List and summarize the three basic processes of urine formation including filtration, reabsorption, and secretion.
1. Glomerular filtration
-Water and solutes moved out of glomerular capillary into tubule
-Filtrate
2. Tubular reabsorption (into the blood)
-Out of tubule back into the blood (peritubular capillaries)
-About 99% of water and many solutes reabsorbed
3. Tubular secretion
-Out of blood into tubule through peritubular capillaries
-Makeup of filtrate changes thorugh nephron
Excretion fo any solute= Glomerular filtration+secretion- absorption
What is the glomerular filtration membrane
-150-180 liters/day filtered from blood at glomerulus
-High surface area, thin membrane
-Fenestrated capillary is covered by podocyte
-Allows fluid and small solutes out (of blood), prevents cells nad proteins from leaving (blood)
What are the things that affect glomerular filtration
1.Hydrostatic blood pressure (main): Increases filtration
-Blood pressure of the glomulerular capillaries (regulated by arterioles)
2. Capsular pressure: Decreases filtration
-Fluid pressure already in the capsular space (back pressure)
3. Blood colloid osmotic pressure: Decreases filtration
-Proteins in blood plasma draws water back into blood.
Define glomerular filtration rate (GFR) and how it is tested.
The glomerular filtration rate (GFR) is the amount of filtrate formed in all the renal corpuscles of both kidneys each minute.
-It is directly affected by glomerular hydrostatic pressure which is controlled by afferent and efferent arterioles.
-It can be tested dby using creatinine:
-Waste molecule from muscles
-Creatinine clearance test: Measures levels in the blood vs. levels in the urine
-Since creatininie is not reabsorbed into blood, it tests the filtration rate.
What happens to GFR rate is messed up?
Too high: Substances pass too quickly and are not reabsorbed
Too low: Nearly all reabsorbed and some waste products not adequately excreted
Explain GFR is changed with vasoconstriction and dilation
-Afferent arteriole Dilation: Increased glomerular hydrostatic pressure which leads to increased filtrate
-Afferent arteriole vasoconstriction: Low glomerular hydrostatic pressure which leads to decreased filtrate
-Efferent arteriole vasoconstriction: Increased glomerular hydrostatic pressure (blood cannot get out very fast), and increased filtrate
Describe hormonal, neural, and autoregulatory mechanisms that affect GFR.
Renal autoregulation:
-Special sensory cells in juxtaglomerular complex sense flow and water/ionic components in blood and filtrate, they can affect the speed of the filtration.
Neural regulation:
-At rest, no sympathetic activity= max. dilation
-Stimulation= Both afferent and efferent arterioles constrict, GFR decreases.
Hormonal regulation:
-Angiotensin 2- Vasoconstrictor of both afferent and efferent arterioles= Reduces GFR (Less urine produced) (low blood pressure)
-Atrial natriuretic peptide: (when we have too high of blood pressure), relaxes cells holding capilllary endothelium, increased capillary surface area and increases GFR
Explain the functions of reabsorption the the proximal convoluted tubule (PCT) Include the major products reabsorbed
-60-70% of reabsorption (filtrate to blood) happens in proximal convoluted tubule.
-Most of what was filtered is immediately reabsorbed
-Lining cells have microvilli to increase absorptive surface area
-Sodium is removed through active pump
-Glucose follows through secondary active transport (very important) and there should be none in the urine. However if levels are too high in the blood it cannot all get removed which creates more solute in filtrate and therefore more water so more urine.
-Amino acids, lactic acid, water soluble vitamins are reabsorbed.
Reabsorption of many ions as well: Sodium, potassium, calcium
-Water moves through osmosis to be reabsorbed if enough solutes are reabsorbed.
-Bicarbonate also here.
Explain the functions of Secretion in the proximal convoluted tubule (PCT) include the major products filtered
-Secretion also occurs in the PCT but mostly in the second half
-Creatinine: While filtration is the source for most, some secretion of creatinine is possible (remember secretion means into the filtrate from the blood)
-Pharmaceuticals
-Uric acid (similar to urea, but from nucleic acid metabolism)
Explain obligatory and faculatative movement in the kidneys
-Solutes reabsorbed by active and passive processes
-Water folows by osmosis
PCT, loop of Henle= Most movement will not vary (in homeostasis)
DCT, collecting duct Hormonal regulation of secretion/reabsorption
Differentiate the function of the descending limb of the nephron loop with the thick ascending nephron loop (The loop of Henle). Include the major products filtered and reabsorbed
Descending (thin) limb: Mostly water reabsorption
-Passive, osmosis
Ascendeing (thick) limb: Na+ reabsorption
-Active pumping
-Other ions through passive if gradient is there
Explain the functions of the distal convoluted tubule (DCT). Include the major products filtered and reabsorbed
-Reabsorption of Na+ and Cl- continues
-Macula densa senses concentration at meeting with loop
-Balanced by K+ secretion
-Regualted by aldosterone
-Not very permeable to water unless ADH is high
-Parathyroid hormone stimulates reabsorption of Ca2+
-Most of this has been reabsorbed but it is fine tuned/regulated here
Summarize the structure and function of the collecting ducts.
-Multiple nephrons drain to collecting duct
-By end of DCT, 95% reabosrbed
-Final adjustments are done:
-Na+ and K+ (aldosterone)
-Bicarbonate, ammonia, H+ mvoement to regulate pH
-Water reabsorption is again variable due to ADH
Diagram the flow of filtrate through the nephron and collecting ducts.
-Essentially what will happen is that in the glomerulus, the glomereular capillaries will undergo filtration by sending out a whole bunch of stuff that is called filtrate and goes into the PCT
-IT goes through te PCT and then the Loop of Henle and then the DCT and out the collecting ducts.
Differentiate "filtrate" from "urine".
Filtrate is what eventually becomes urine when the nephrons have completed reabsorption (into blood) and secretion (into nephron)
Explain the effects of aldosterone, parathyroid hormone, and antidiuretic hormone on urine contents and concentration, including the section of the nephron affected by each hormone.
Aldosterone: It increases Na+ reabsorption to blood, so water follows, so you increase blood pressure. Decreases urine output.
ADH: Allows the movement of water to follow the Na+ to be reabsorbed by blood. It does this by allowing the increased expression of aquaporins. Decrease of urine output, increase in blood volume
-Both of these hormones expressed in the DCT and Collecting duct
Parathyroid hormone stimulates reabsorption of Ca2+ (it is for low calcium): It increases calcium pumps. This is found in the distal convoluted tube.
Explain the concentration gradient of the medulla and relate its relationship to the nephron loop and collecting ducts.
-As collecting duct goes into medulla, extra-tbuular fluid is highly osmotic
-ADH causes aquaporins in membrane
-Osmosis draws water out of urine, making urine more concentrated
-When excess water, ADH not secreted and collecting duct impermeable to water
Look at the picture in your slides to understand more.
Define extracellular fluid (ECF) and intracellular Fluid (ICF).
-Fluid makes up about 55-60% of body mass.
-Intracellular fluid (ICF): About 2/3 of body fluid.
-Extracellular Fluid (ECF): 1/3
-Interstitial fluid- about 80% of ECF
-Plasma in blood-about 20% of ECF
-Also includes lymph and other fluids.
List and describe the relationship between the regulation of fluids and electrolytes.
THe volume of fluid in each is kept constant. Since water follows electrolytes, they must be in balance as well. You can regulate electrolytes to regulate water.
Explain fluid shift between the ECF and ICF and the mechanism that drives water movement.
-ECF/ICF balance shift caused by change in osmolarity (usually Na+ concentration)
-Increasing ECF osmolarity draws water out of cells and the cells shrink
-Decreasing ECF osmolarity causes cells to swell.
Explain what causes hyperhidrosis and why it is damaging to the body.
Hyperhidrosis: Increased intake of NaCl
-Causes increased plasma concentrations of Na+ and Cl-
-INcreased osmosis of water from intracellluar fluid to interstitial fluid to plasma.
-Increased blood volume which causes:
-Increased stretching of the atria of hear and increased release of ANP
-Decreased release of renin and angiotensin which causes increased glomular filtration rate and decreased release of aldosterone.
-All of these things cause reduced reapsorption of NaCl by kidneys
-Increased loss of Na+ and Cl-
-Increased loss of water in urine by osmosis.
Explain what causes water intoxication and why it is damaging to the body.
-Excessive blood loss, sweating, vomiting, diarrhea coupled with intake of plain water causes:
-Decreased Na+ concentration of interstitila fluid and plasma
-Decreased osmolarity of interstial fluid and plasma
-Osmosis of water from interstitial fluid into intracelluar fluid
-Water intoxication (Cells swell)
-Convulsions, coma, and possible death
-Can be treated by replacing lost electrolytes.
Define acidosis and alkalosis.
Acidosis- pH below 7.35
Alkalosis- pH above 7.45
Explain the basic relationship between the partial pressure of CO2 and pH.
INcreasing of C02 whcih can be caused by lowering of the respiratory rate causes increased increased carbonic acid whcih then forms bicarbonate ion as well as a H+, so you decrease pH causing respiratory acidosis.
Explain how the respiratory system and urinary system maintain blood pH.
REspiratory system:
-pH modified by chanign rate and depth of breathing. Faster breathing increases pH, slower breathing decreases it.
-H+ detected by chemoreceptors in medulla oblongata, carotid and aortic bodies
-Respiratory centers inhibited or stimulated by changes in pH
Urinary system:
-Many metabolic reactions prdouce acid. Excretion fo H+ in the urine is only way to eliminate large excesses.
-Kidneys synthesis new bicarbonate and save filtered bicarbonate
-Urine can be up to 1000 times more acidic than blood
-Renal failure can cause death rapidly due to its role in pH balance.