Immuno Exam 3: Pregnancy
1/75
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
76 Terms
what test is done on the first prenatal visit
maternal blood tests
3 Types of maternal Blood tests
-HCG (pregnancy confirmation)
-Anitgen typing of RBC (AOB and RH)
-Indirect Coombs test
Indirect Coombs test
screen for antibodies that can cause hemolysis of fetus/newborn
what does it mean if Indirect Coombs is postive
mother is already sensitized bad
what does it mean if Indirect Coombs is negative
mother is not sensitized
can be given rhogam if needed
3 types of RBC antigens
- ABO
-Rh-D
-Atypical antigens
6 possible ABO genotypes
AA, AO, BB, BO, AB, OO
4 types of ABO phenotypes (Blood types)
Type A, B, O, or AB
type A
AA or AO
type B
BB or BO
type O
OO
Type AB
AB
what blood type is a universal donor and which is a universal recipeint
universal recipient: AB
universal donor: O
type A blood
A antigens present on red blood cells (self)
body makes anti-B antibodies (recognizes non-self if exposed)
type B blood
B antigens present on red blood cells (self)
body makes anti-A antibodies (recognizes self if exposed)
why is type O a universal donor
blood could be accepted by people wth other blood types without rejection
type O blood
do NOT have A or B antigens
body makes anti-A and anti-B antibodies (recognizes non-self if exposed)
why is type AB blood a universal recipient
people with type AB blood can be given type A, B, and O blood without rejection
Type AB blood
A and B antigens present on red blood cells (self)
body does NOT make anti-A or anti-B antibodies
what is the root cause of blood transfusion errors
a problem with documentation
ABO blood transfusion incompatability
A and B antigens are very immunogenic
corresponding antibodies (anti A and B) are strongly hemolytic
wif the mother's blood type is incompatible with the blood type of the fetus
• mother's immune system can recognize the fetal tissue as "non self
"• mother creates antibodies against the fetus' RBC
• RBC antibodies can cross the placental barrier and damage/kill fetal RBC
why are A and B antigens less immunogenic during gestation than in children/adults
because they're not well developed during gestation
transfusion vs fetal hemolytic disease
fetal/newborn hemolytic disease is MILD compred to adult transfusion reactions because antigens are less well developed during fetal/newborn
Rh antigens
RBC surface antigens (Rh factor= Rhesus factor)
is there a prophylatic therapy for blood type incompatibility?
no
Rh-D antigen
most immunogenic of Rh antigens
only Rh antigen with a medical prophylatic therapy
possible Rh-D phenotypes
Rh-D "positive": Dd, DD
Rh-D "negative": dd
Rh-D incompatibility
occurs when an Rh-d (negative) mother ispregnant with an Rh-D (positive) fetus.
The mother's immunesystem recognizes the Rh-D antigen as non-self.
chances of contributing D if father is Dd vs DD
DD then 100% chance of contributing D•
Dd then 50% chance of contributing D, 50% chance ofcontributing d (lack)
alloimmunization
immune response to foreign antigens after exposure to genetically different cells or tissues
process of alloimmunization
1. maternal sensitization
2. maternal production of IgG antibodies
3. Maternal antibodies cross placenta to fetus
4. antibody mediated hemolysis in fetal RBC
how does maternal Rh-D sensitization occur
mom exposed to "non-self" antiges BEFORE or DURING pregnancy/delivery
Rh- mom exposed to Rh+ blood AT ANY POINT in her life
Rh- mom initial exposure to Rh-D antigen and after exposure
primary immune response is slower and weaker compared to future exposures IgM anti-D does not cross placenta
secondary conversion to anti-D IgG production (immunoglobulin class switching), crosses placenta
when are anti-D IGM found in ciruclation after Rh- mom is exposed to Rh-D antigen
anti-D IGM found in ciruclation 8 weeks-6 months after exposure
if exposure and Rh-D sensitization is durig pregnancy/delivery...
the baby is UNAFFECTED
• IGM response occurs first and IGG response is weeks/months later (IGG crosses the placenta and can affect fetus)
• The lag in maternal immune response to fetal antigen often means the pregnancy is over before the fetus is affected (it has already been born!).•
if exposure and sensitization of Rh-D occurs before pregnancy/delivery...
the baby is AFFECTED earlier in gestation and more severely
• Subsequent pregnancies after 1st Rh-D baby
• FIRST pregnancy if mother was previously exposed/sensitized in another way
4 risk factors affecting maternal sensitization
-volume of blood exposure
-extent of maternal immune response
-fetus homozygous vs heterozygous for D antigen (Dd or DD)
-concurrent presence of ABO incompatability
how does volume of blood exposure affect risk of maternal Rh-D sensitization?
smaller embryo/fetus--> less blood volume
complication types of the fetus of blood type incompatability in pregnancy
-anemia--> erythroblastosis fetalis
-juandice--> kernicterus
-hydrops fetalis
anemia (low RBC count) results in
-decreased oxygen carrying capacity
-increased cardiac workload; tachycardia
-erythroblastosis fetalis
erythroblastosis fetalis
an anemic blood disease of a fetus or newborn, characterized by erythroblasts in the circulating blood
jaundice
yellowing of the skin and whites of the eyes caused by excess bilirubin (product of heme breakdown ) in the blood
kernicterus
a life-threatening form of brain damage caused by excessive jaundice
hydrops fetalis
a severe, life-threatening edema in the fetus/newborn
bilirubin during pregnancy
bilirubin from breakdown of fetal hemoglobin can be cleared via placenta to maternal circulation → bilirubin is conjugated and excreted by mom
bilirubin after delivery
infant has low levels of glucuronyl transferase enzyme→ cannot conjugate and clear the bilirubin as efficiently
baby with high serum bilirubin--> jaundice
what is required for determining the risk of Rh incompatability for each pregnancy
good prenatal care
when can alloimmunization be prevented
If Rh- mom has not been exposed to Rh antigen because this means she hasn't been sensitized
when is it too late to prevent alloimmunization?
Rh- mom is already exposed and sensitized to Rh antigen
who should be treated with Rh IgG injections
all unsensitized Rh- moms possibly carrying an incompatible fetus
what does Rh IgG do
-provides passive immunity
-supresses the immune response to Rh+ blood in non-sensitized Rh- females
-prevents maternal sensitization and formation of active Rh-D antibodies
-prevents Rh hemolytic disease in Rh+ neonates
ONLY effective for current pregnancy, not future ones
routine administration of Rh IgG in Rh- moms at risk
• mid-pregnancy (around 28 weeks gestation)
• within 72 hours after delivery (can admin up to 2 weeks after delivery if initial window missed)
as needed administration of Rh IgG in Rh- moms at risk
•Post-miscarriage/termination
• Post-ectopic pregnancy
• After prenatal tests such as amniocentesis and chorionic villus biopsy -(puncture/rupture)
• After injury to the abdomen during a pregnancy
contraindications to Rh IgG
Rh+ individuals
brands of anti-D immune globulin
rhogam, rhoplac, rho-sdf, hyperrho S/D, micrhogam
route of admins for anti-D immune globulin
brand specific IM or IV
which conditions would you give 300mcg of anti-D immune globulin
antenatal and postpartum, 2nd and 3rdtrimester pregnancy miscarriage/terminations,transplacental hemorrhage
which conditions would you give 50mcg of anti-D immune globulin
1st trimester pregnancy miscarriage/terminations
how do you know when alloimunization occurs after maternal sensitization?
maternal and fetal montioring
maternal monitoring of alloimmunization
antibody titers
invasive fetal monitoring of alloimmunization
-amniocentesis
-percutaneous cord blood
non-invasive fetal monitoring of alloimmunization
-ultrasound
-cerebral artery doppler ultrasound
-non-stress test (NST)
maternal antibody titers, what do higher levels mean? what do lower levels mean?
higher levels--> greater immune response against a specific antigen
lower levels--> rarely result in severe hemolytic disease
what info is obtained in invasive fetal monitoring
fetal antigen status, presence of anemia or increased levels of bilirubin
what info is obtained in non-invasive fetal monitoring methods (like ultrasound)?
assess fetal grwoth, development, and presence of hydrops
middle cerebral artery dopplr ultrasound
-assesses fetal anemia
-faster flow with fewer RBC (less viscous)--> increased HR
non-stress test (NST)
-not harmful to fetus
-used after 28 weeks gestation
-uses monitors on maternal abdomen to measure fetal heart rate and maternal contractions
goal of non-stress test
-measure fetal HR in response to own movement
-increase movement ocrrelates with increased HR
reactive vs non-reactive non-stress test results
reactive- blood flow, O2 is adequate
non-reactive: rule out other causes (asleep, meds, etc) but O2 may not be adequate
when is early delivery
~32-35 weeks gestation
betamethasone
administered in anticipattion of an early delivery to induce production of surfactant in the fetal lungs
lubricates air sacs of the lung--> hasten lung development, imrpoves survival outsdie of the womb
betamethasone also decreases the risk for...
-brain bleed (intraventricular hemorrhage)
-necrotizing enterocolitis (severe intestine infection)
-mortality
corticosteroid
will suppress meternal immune system to lead o reduced alloimmunization effects
dose of betamethasone
12mg x2 doses
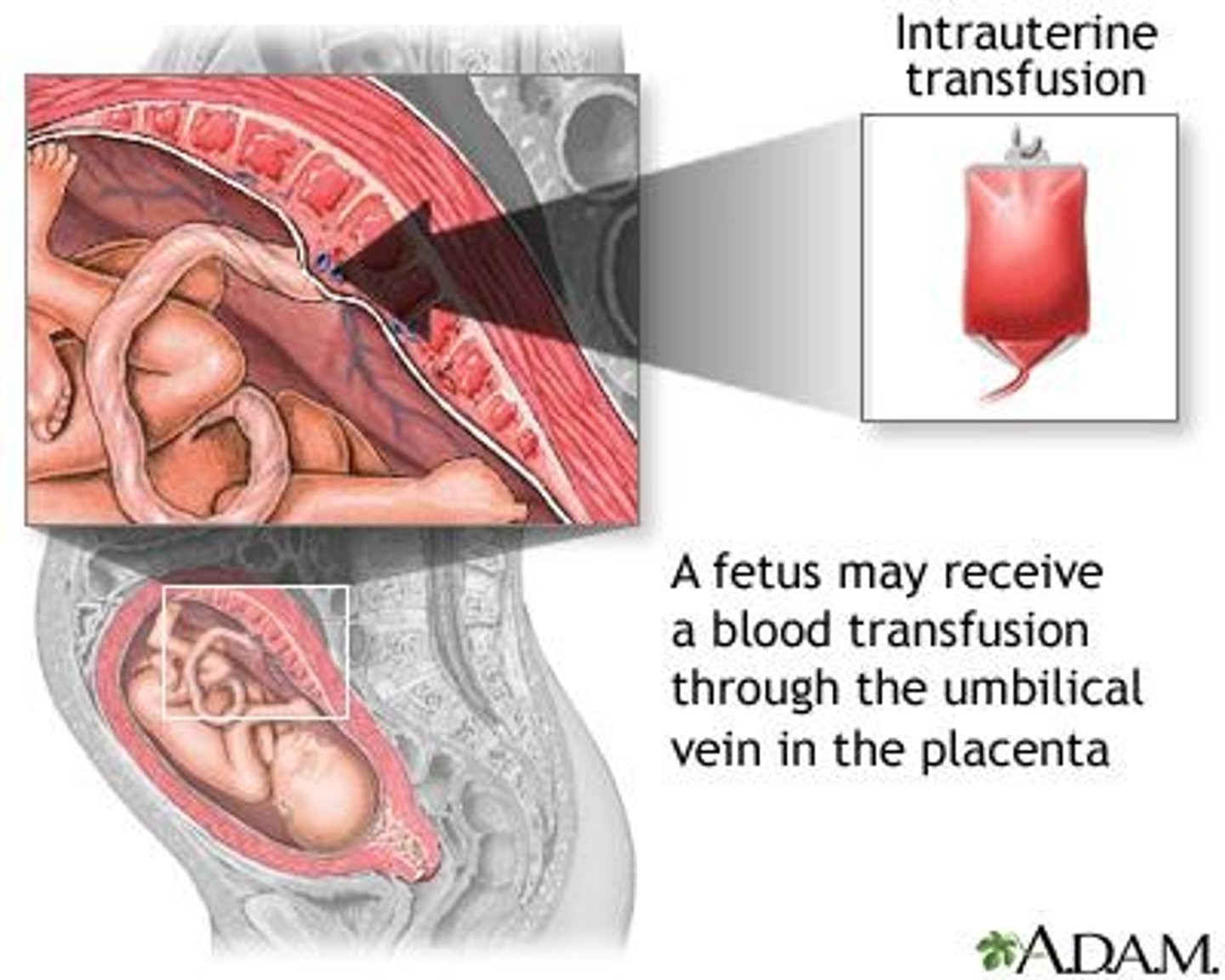
intrauterine transfusion use
used when possibility for severe anemia at <35 weeks gestation