Exam 1 - Renal
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
61 Terms
what is an acute injury (AKI)?
rapid loss of renal function due to damage to the kidneys
why are AKIs significant?
wide range of life-threatening metabolic complications can subsequently occur:
- metabolic acidosis
- fluid and electrolyte imbalances
what are the 2 diagnosis requirements for AKI?
1. 50% or greater increase in serum creatinine above baseline (normal creatinine is < 1 mg/dL)
2. urine volume may be normal OR could be:
- nonoliguria (>800 mL/day)
- oliguria (<400 mL/day)
- anuria (<50 mL/day)
what causes AKI?
reduced blood flow to kidneys
what are some potential causes of AKI?
- hypovolemia
- hypotension
- reduced cardiac output
- heart failure
- obstruction of kidney or lower urinary tract (tumor, blood clot, stone)
- obstruction of renal arteries or veins
what are the 3 AKI categories?
1. prerenal (hypoperfusion/reduced blood flow coming to kidney)
2. intrarenal/intrinsic (actual damage to kidney tissue)
3. postrenal (obstruction to urine flow beyond the kidney)
what causes prerenal AKI?
impaired blood flow leads to hypoperfusion of the kidney
- volume depletion (burns (3rd spacing), hemorrhage, GI losses)
- hypotension (sepsis and shock)
- obstruction of renal vessels (clots, trauma)
what finding would you see in a patient with prerenal AKI and what does it mean?
decreased GFR (less filtration is occuring in the tubules)
what causes intrarenal AKI?
acute parenchymal damage to glomeruli or kidney tubules
what is acute tubular necrosis (ATN)?
- damage to kidney tubules
- most common type of intrinsic AKI
what findings would you see in a patient with ATN?
- decreased GFR
- progressive azotemia (increased nitrogen in bloodstream which increases BUN/Cr)
- F & E imbalances
what causes postrenal AKI?
obstruction distal to the kidney, which causes pressure to rise in the kidney tubules
- renal calculi
- strictures
- blood clots
- BPH
- malignancy
- pregnancy
what are the 4 phases of AKI in a healing patient?
1. initiation
2. oliguria
3. diuresis
4. recovery
what occurs in the initiation phase of AKI?
initial onset
what occurs in the oliguria phase of AKI and what is the patient at risk for?
- decreased urine output: < 400 mL/day (400mL/day is the minimum amount of urine needed to rid the body of normal wastes)
- increase in serum concentration of substances
- uremia symptoms appear (confusion, reduced appetite, seizures, N/V, coma)
- RISK FOR HYPERKALEMIA
what occurs in the diuresis phase of AKI and what is the patient at risk for?
- gradual increase in urine output (GFR is trying to recover)
- lab values stabilize
- urine output may return to normal or be elevated (DEHYDRATION RISK)
what occurs in the recovery phase of AKI?
- improvement of renal function!
- lasts 3-12 months
- lab values are normal!
what are the CNS clinical manifestations of AKI?
- drowsiness (d/t decreased cerebral perfusion)
- H/A (d/t dehydration)
- muscle twitching (d/t hypocalcemia)
- seizures (d/t hyponatremia)
what is one of the earliest signs of AKI?
low urine specific gravity - urine is not being concentrated
what are potential assessment and diagnostic findings for AKI (11)?
- urine changes: volume changes, hematuria, low specific gravity, abnormal sodium levels
- azotemia (in prerenal and intrarenal)
- ultrasonography: structural/anatomical changes
- BUN increases steadily (d/t protein breakdown)
- Cr increases (d/t glomerular damage)
- GFR decreases (d/t glomerular damage)
- serum K+ increases as GFR decreases because it is not being excreted
- cardiac arrhythmias: peaked T-waves d/t hyperkalemia, VTach and cardiac arrest
- metabolic acidosis (renal buffering system fails)
- other electrolyte imbalances
- anemia (erythropoiesis begins in the kidneys!)
how can AKI be prevented (4 ways)?
1. limit exposure to nephrotoxic agents and environmental toxins
2. avoid nephrotoxic medications
3. assess PMH to identify risk factors
4. pre-hydration with IV NS before contrast (helps flush contrast out)
what are 4 conditions that put you at risk for AKI?
- cirrhosis
- HF
- pre-existing kidney disease
- diabetes
what are 2 major nephrotoxic medication families?
1. aminoglycosides (gentamicin, tobramycin, vancomycin, cyclosporine)
2. NSAIDs (cause interstitial nephritis)
what are the 2 medical management goals for AKI?
1. restore normal chemical balance
2. prevent complications until repair of tissue and restoration of function can occur
how do we medically manage AKI (3 things)?
1. eliminate underlying cause
2. maintain fluid balance
3. RRT/dialysis
what do we need to monitor closely for when administering fluids to AKI patients?
FVO!
- HTN
- tachycardia
- coughing
- crackles
- dyspnea
- HTN
- JVD
how do we assess for hyperkalemia, and how do we treat it?
assessment:
- serum levels
- ECG (peaked T wave)
- abdominal cramping
treatment for ECG changes:
- IV dextrose 50%, insulin, and calcium replacement (insulin shifts K+ and glucose into cells, dextrose stabilizes blood sugar, and calcium stabilizes cells)
what medications (4) are likely to require dose changes for a patient with AKI?
- aminoglycosides
- digoxin
- phenytoin
- ACE inhibitors
how do we treat severe metabolic acidosis in an AKI patient?
- sodium bicarbonate therapy or dialysis
- ventilatory support
what 3 dietary changes are made when a patient has AKI?
- protein replacement
- restrict sodium, potassium, and phosphorus
- high-protein, high-calorie diet
what are the 6 components of nursing management of AKI?
1. monitor fluid and electrolyte balance (I&O, heart and lung sounds)
2. reduce metabolic rate (reduce fevers)
3. promote pulmonary function (supplemental O2, coughing and deep breathing)
4. prevent infection (avoid catheters and IVs)
5. skin care (edema = prone to pressure injuries)
6. psychosocial support (requires long-term treatment, pt and family may be anxious and scared)
what is end-stage kidney disease (ESKD)?
the final stage of chronic kidney disease (CKD), where kidneys lose nearly all function, requiring dialysis/RRT permanently or a kidney transplant for survival as they can't filter waste effectively, and the end product of protein metabolism (uremia) accumulates in the blood
what 3 things is the rate of decline in ESKD directly related to?
1. underlying disorder
2. urinary excretion of protein
3. presence of HTN
what are 4 clinical manifestations of ESKD?
extensive complications!
- cardiovascular disease (predominant cause of death)
- peripheral neuropathy
- pain and discomfort
- restless leg syndrome r/t uremic peripheral neuropathy
how do GFR and BUN/Cr change with kidney injury?
- GFR decreases
- BUN/Cr increases
what are 7 assessment and diagnostic findings for ESKD?
- decreased GFR
- increased BUN/Cr
- sodium & water retention (edema, HF, HTN)
- sodium & water loss (hypotension, hypovolemia)
- acidosis
- anemia (kidneys don't make enough EPO)
- electrolyte imbalances
what are 5 complications of ESKD?
1. anemia
2. bone disease
3. hyperkalemia
4. HTN
5. cardiac complications: pericarditis, pericardial effusion, pericardial tamponade
what is our treatment goal for ESKD?
- maintain homeostasis & treat the underlying cause
- we want to regulate intravascular volume so that we have enough fluid to perfuse the kidneys, but not enough to cause HTN and worsen the issue
what does medical management of ESKD include?
pharmacological:
- calcium and phosphorus binders
- antihypertensive agents
- erythropoietin
nutritional therapy:
- protein!
- fluid intake
- restrictions
dialysis
what does nursing management of ESKD include (4 components)?
1. assessing fluid status
2. ensuring adherence to dietary plan
3. supporting family and patient
4. collaborating with interdisciplinary team
what are the 3 types of renal replacement therapy (RRT)/dialysis?
1. hemodialysis (HD)
2. continuous renal replacement therapy (CRRT)
3. peritoneal dialysis (PD)
what is acute/urgent RRT used for vs. chronic/maintenance RRT?
acute/urgent: pulmonary edema, hyperkalemia, etc
chronic/maintenance: kidney failure
what is hemodialysis (HD) used for and what does it do?
- used for acutely ill and long-term RRT
- does not cure kidney disease (just does the filtering for the kidneys because they cannot)
- removes waste (nitrogenous substances) and extra fluid by sending blood through a dialyzer where it is cleaned by diffusion, then returned to the body
how does hemodialysis work?
- access site (AV fistula, AV graft, or CVC)
- blood travels through tubing and is pumped into the dialyzer which is a canister containing thousands of tiny semipermeable fibers (it's basically a kidney!)
- blood flows inside these fibers while dialysate (cleaning fluid) flows outside them in the opposite direction
- waste products like urea and extra water pass from the blood through the fibers into the dialysate
- dialysate is discarded
- cleaned blood is returned to the body through the vascular access
cleans the blood quickly a few times a week
what are HD vascular access devices, what are the 3 types, and what must you assess daily?
allow blood to be removed, cleansed, and returned to vascular system at rapid rates of 300-500 mL/min
3 types:
- AV fistula
- AV graft
- double-lumen, cuffed HD catheter
feel for the "thrill" (a buzzing sensation) and listen for the "bruit" (a swooshing sound) to ensure the access is working
what are 6 complications of HD?
1. rapid fluid shifts (fluid and wast are removed from the body very quickly: can cause patient to feel ill, N/V)
2. complication of co-morbidities (cardiac, diabetes)
3. fluid overload between treatments (fluid builds up between dialysis sessions)
4. intolerance of fluid removal during dialysis (hypotension - too much fluid is removed too fast and circulating blood volume drops)
5. exanguination (severe blood loss if access or tubing becomes disconnected)
6. air embolism (air enters bloodstream and blocks blood flow to vital organs)
what is CRRT and when is it used?
continuous renal replacement therapy:
- “gentle, nonstop dialysis for unstable patients”
- continuous, slow form of dialysis used in critically ill patients who cannot tolerate rapid fluid shifts
- better BP control
- can be initiated quickly in a critical care unit
- requires a CVC (no AV fistula or graft)
- blood passes through artificial filter (hemofilter)
what are the goals of peritoneal dialysis (PD)?
1. remove toxic substances and metabolic wastes
2. re-establish normal fluid and electrolyte balance
why choose peritoneal dialysis?
1. patient preference (can be done at home)
2. if you are susceptible to HD complications
3. high benefits (independence and control)
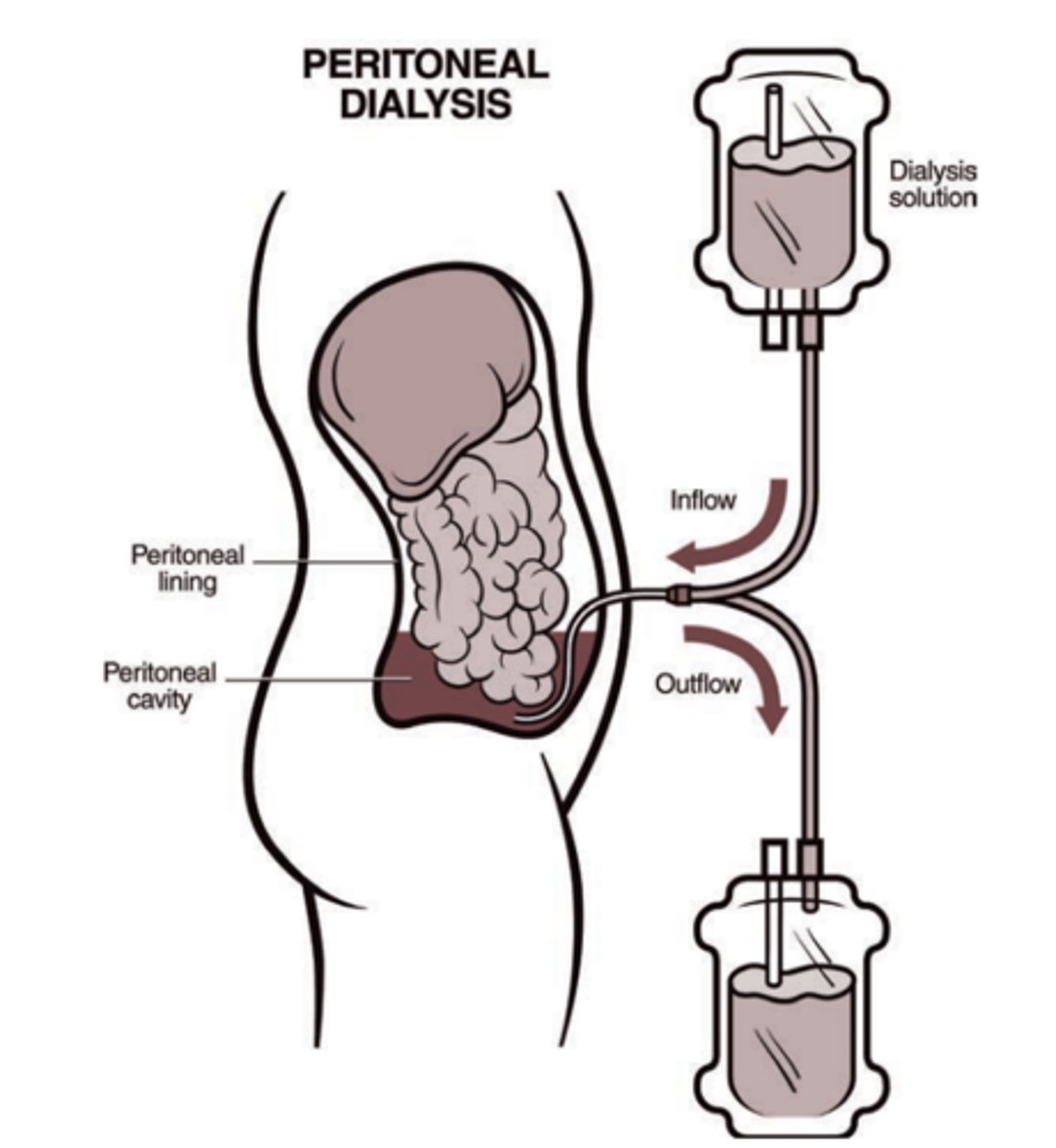
what are 4 potential complications of peritoneal dialysis?
1. peritonitis
2. leakage
3. bleeding
4. hypertriglyceridemia
what is a sign of peritonitis in a patient undergoing peritoneal dialysis and what should you do if you see this sign?
- discoloration/cloudiness of dialysate drainage
- obtain a specimen for C&S!
what does nursing management for peritoneal dialysis patients include?
- equipment and process
- psychosocial needs (altered body image, altered sexual patterns)
- assess for electrolyte imbalances
- assess for fluid overload
- prevent infection
what are 3 key things to know about kidney transplantation?
1. select and screened patients
2. not a cure for ESKD (kidneys do not last forever)
3. long waiting lists
what 3 things are required preop for a kidney transplant?
- normal metabolic state (diet, dialysis, medical management)
- free of infection
- education for postoperative plan
what does medical management for both the recipient and donor in a kidney transplant include (5 things)?
- tissue and blood typing
- antibody screening
- infection management
- recipient prescribed anti-rejection medications (immunosuppressant)
- psychosocial evaluation
what does nursing management for a kidney transplant include (6 things)?
- pulmonary hygiene
- pain management
- dietary restrictions
- IV fluid administration and maintenence
- early ambulation
- psychosocial support
what are signs of rejection and failure following a kidney transplant, and when can rejection occur?
- fever
- malaise
- changes in urine output
can occur within 24 hours, 3-14 days, or many years later
why are the kidneys at risk for trauma?
anatomical placement - they are not protected!
what are the 2 types of renal trauma and some potential causes?
1. blunt renal trauma: MCV, falls, assaults
2. penetrating renal trauma: gunshot wounds, stabbings
what 5 things does medical management of renal trauma include?
1. control hemorrhage
2. control pain
3. control infection
4. preserve and restore renal function
5. surgery (laceration management, often exploratory)
what should you assess in a patient following renal trauma (6 things)?
frequent assessments:
- pain (flank, abdomen, muscle spasm)
- swelling, bruising, redness over flank
- surgical incision
- fever
- hematuria
- decreasing kidney function (serial labs)