Urinary System - A&P II
1/107
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
108 Terms
Why is maintaining a minimal blood pressure essential for kidney function? In other words, what does GFR have to do with RBF?
a minimal blood pressure is essential for kidney function as it ensures there is enough pressure to push fluid through the glomerulus.
What are the 2 major functions of kidneys?
filter blood to produce urine and regulate blood pressure
What are the effects of diuretics on kidney function? On blood pressure?
diuretics increase urine output, essentially enhancing kidney function and decreasing blood pressure
to remove liquid wastes from the blood and regulate blood volume (and therefore pressure)
urinary system function
the urinary system excretes these wastes
excess electrolytes and nitrogenous and other metabolic wastes (urea)
main organs of blood filtration
kidneys
carry urine from kidneys to bladder
ureters
stores urine prior to micturition (urination)
bladder
carries urine out of the body
urethra
micturition
urination
kidneys consume roughly 20-25% of ____ used by the body at rest
oxygen
why do kidneys use so much oxygen
they are extremely metabolically active
why do the kidneys filter your entire blood volume roughly 60 times a day
to keep the blood free from waste products and to conserve as much water as possible
kidneys are highly dependent on…
blood pressure
how many layers of connective tissue surround each kidney
three
name the three layers of connective tissue surrounding each kidney
renal fascia, perirenal fat capsule, fibrous capsule
anchors kidney and adrenal gland to surrounding structures
renal fascia
surrounds kidney and protects it from damage
perirenal fat capsule
impermeable connective tissue that protects kidney from infections
fibrous capsule
why are kidneys considered “retroperitoneal”
they are not located within the abdominal (peritoneal) cavity, but in the lining behind the cavity
supplies blood to be filtered
renal artery
filtered blood returns to circulation
renal vein
concave surface (medial surface)
hilum
distal tissue layer (outside layer)
renal cortex
renal pyramids (lobes)
renal medulla
renal medulla drains into the…
renal pelvis
why do the blood vessels in the kidneys get really small
increased surface area allows for rapid filtration
brings blood to kidney - up to ¼ total CO per minute
renal artery
renal artery branches into ____ that branch smaller and smaller, eventually to capillaries around each nephron
segmental arteries
list the three steps to urine formation
“squeeze” liquid from the blood (filtrate)
reabsorb necessary components (still filtrate)
actively secrete wastes into liquid that is left over (urine)
“squeeze” liquid from the blood (filtrate)
step 1 of urine formation
reabsorb necessary components (filtrate)
step 2 of urine formation
actively secrete wastes into liquid that is left over (urine)
step 3 of urine formation
the functional unit of filtration in the kidney
nephron
about _______ nephrons per kidney
1 million
fluid collected from _____ is sent to the renal pelvis via collecting ducts
nephrons
tuft of capillaries that removes wastes from blood via hydrostatic pressure
glomerulus
renal corpuscle
nephron
fluid leaves the capillaries and goes into the…
glomerular capsule
fluid leaves the glomerular capsule and passes into the _____ to be processed into urine
renal tubules
tuft of fenestrated capillaries inside the Bowman’s capsule
glomerulus
fenestrated capillaries are very _____, allowing liquids to move out under pressure
porous
fenestrae (holes) are restrictive, meaning…
only very small solute molecules should pass through (H20, sugars, salts, etc.), not large ones (e.g. proteins)
form a network of spaces surrounding the capillaries that limits diffusion of large molecules
podocytes (“foot cells”)
visceral layer clings to the capillaries and contains podocytes
glomerular capsule
collected filtrate from the glomerular capsule is transported via the collecting duct called the…
renal tubule
blood (hydrostatic) pressure gives the glomerular capillaries high enough pressure to squeeze liquid out of the blood and enhance filtrate formation
outward pressure
capsule pressure and osmotic pressure in blood hinders filtrate formation
inward pressure
describe the sum of glomerular pressures
high pressure forces liquid out of the blood (~+55), osmotic pressure making liquid go back in the blood (~-30), hydrostatic pressure from capsule forcing liquid back into capillaries (~-15), resulting in ~+10 mm/Hg moving liquid out of the capillaries
explain how altered blood pressure affects glomerular pressures
for instance, if someone were hypotensive, the pressure forcing liquid of the blood would be lower than normal, so there would not be enough pressure to force liquid out of the capsule, meaning there is no urine production
filtration rate factors
pressure, total surface area, filtration membrane permeability
volume of filtrate produced each minute by both kidneys
glomerular filtration rate (GFR)
these factors lead to glomerular filtration rate (GFR)
pressure, total surface area, filtration membrane permeability
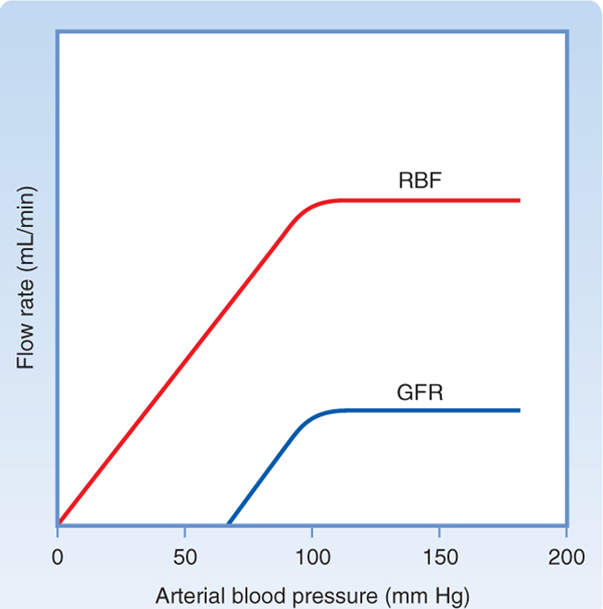
what is the most clinically important feature on this chart
the point at which GFR is 0 (60 mm/Hg) because it shows there is not enough pressure to produce filtrate/urine
what resorbs everything the body needs during step 2 of urine formation
tubules
what do the tubules resorb during step 2 of urine formation
water and other important dissolved solutes
what happens to everything the tubules do not resorb during step 2 of urine formation
becomes urine
what sort of things become urine after tubules do not resorb them during step 2 urine formation
glucose, vitamins, electrolytes, etc.
how is reabsorption in step 2 urine formation accomplished
by both active diffusion and passive diffusion
what are the three distinct sections of the renal tubule
proximal tubule, nephron loop (loop of Henle), distal tubule
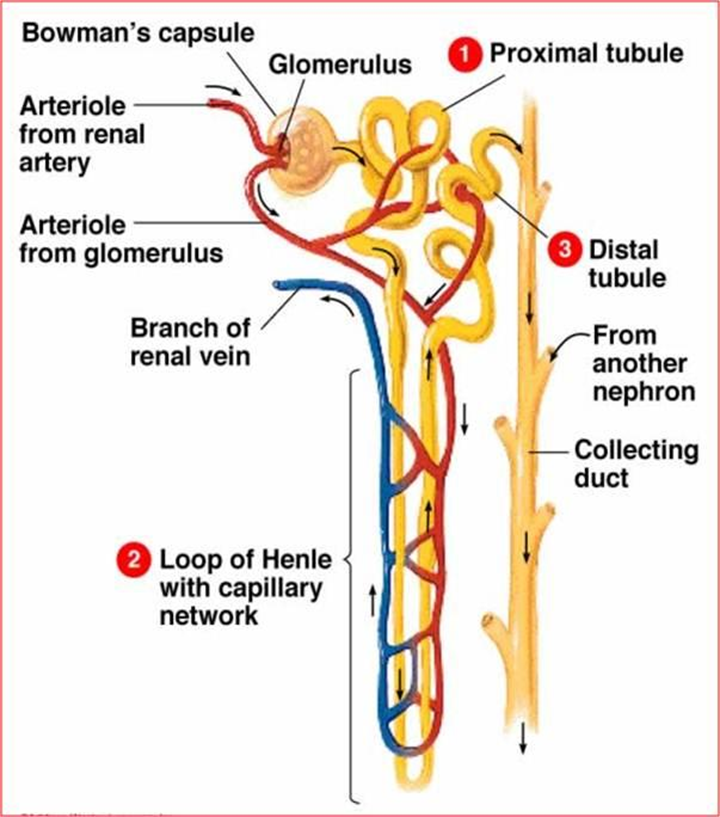
what is the difference between the proximal tubule and distal tubule
proximal tubule is closest to the glomerulus
why is the renal tubule so long
more surface area for diffusion
cling to and readily absorb water and solutes from the filtrate in the renal tubules
peritubular capillaries
peritubular capillaries serve to further…
remove water and useful substances from the filtrate collected from the renal capsule
summarize the glomerular capsule’s role in renal circulation
only arterioles transport blood to the glomerular capsule, very high pressure, allowing water and wastes to be collected in the nephron by diffusion AND physical pressure, producing filtrate
summarize the role peritubular capillaries play in renal circulation
they run along tubules to reabsorb water from waste, under low pressure, longer to produce more concentrated urine, and they reclaim most of the filtrate from the capsule while the rest is excreted as urine
what are the two ways filtrate can be reabsorbed into the renal tubule
transcellular route (across the membrane) and paracellular route (through cellular junctions and interstitial fluid)
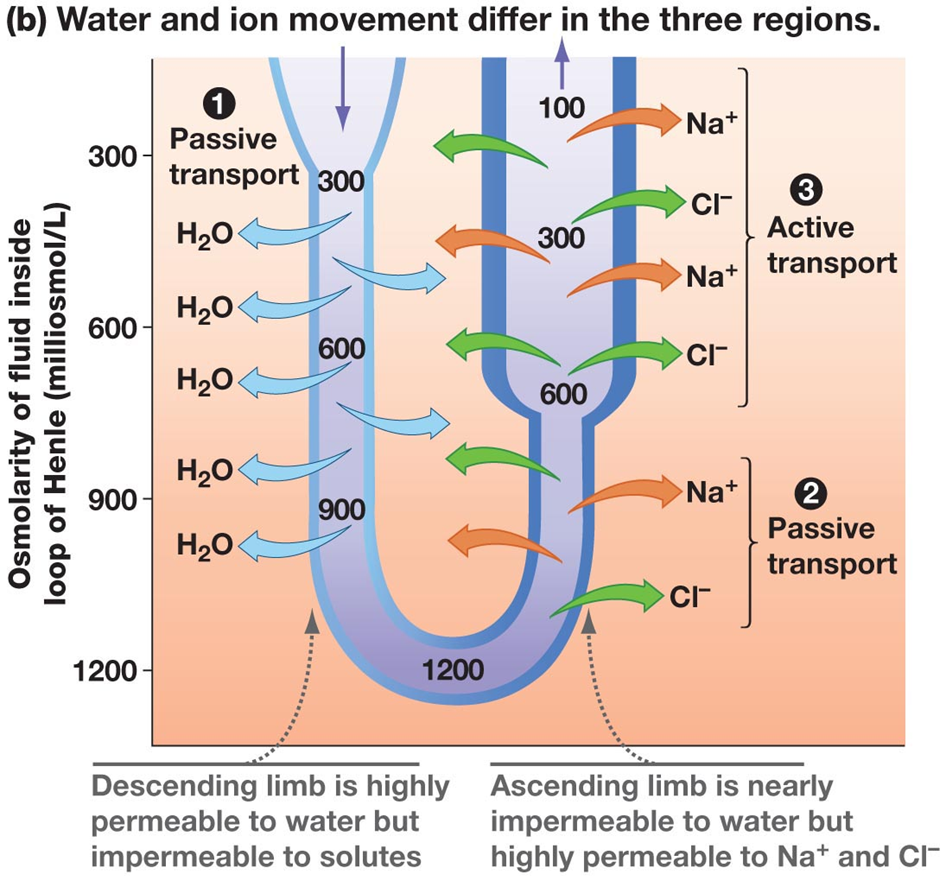
please explain how filtrate from step 1 starts at low concentration, increases in concentration, and then decreases again
during step 1, the concentration increases as the solvent (water) decreases (gets resorbed)
during steps 2 and 3, the concentration decreases as the solutes (Na+ and Cl-) decrease (get resorbed)
reabsorption is limited by the number of…
primary transport proteins for each substance (e.g. sodium- potassium pump)
solutes are co-transported back into the blood with sodium
secondary active transport
water follows solutes into the blood via _____, helping to maintain blood pressure
passive diffusion
these add substances to urine by secreting them during step 3 of urine formation
capillaries
what is the purpose of secreting substances into urine
eliminate drugs and toxic metabolites
regulate K+
control blood pH levels
secretion (step 3) is the opposite of…
resorption (step 2)
increases permeability of the collecting ducts to water, putting water back into the blood
anti-diuretic hormone (ADH)
when ADH is stimulated, it…
increases blood solutes and decreases blood pressure
reduces Na+ secretion (stimulates resorption)
aldosterone
when aldosterone is stimulated, it…
increases K+ and lowers blood pressure (via renin-angiotensin mechanism)
after processing, urine is collected from several nephrons into…
collecting ducts
in each kidney, collecting ducts empty into the…
ureter
reduces urine output resulting in a reduction or stop to urine production
kidney damage
how to treat kidney damage
dialysis, sometimes for life
medication that enhances water excretion
diuretics
how do diuretics enhance water excretion
inhibits ADH secretion and Na+ resorption into the blood
need to test BOTH _____ to clinically evaluate kidney function
blood and urine
urine characteristics
sterile, pale yellow, specific gravity greater than that of water
urine composition
water (95%), urea, uric acid, creatinine, Na+, K+, PO4, SO4
from breakdown of amino acids
urea
transport urine from the renal pelvis to the bladder
ureters
how do the ureters transport urine
peristalsis
what is the diameter of ureters like
VERY thin (1 mm)
precipitated minerals can cause…
kidney stones
three tissue layers of the bladder
mucosa (epithelia), detrusor (smooth muscle layer), adventitia (connective tissue)
allow the bladder to stretch when filling with urine
rugae
flexes and squeezes the bladder to get urine out of the body
detrusor muscle
should have 5 mL or less of urine
empty bladder
what is the danger of having urine stay in the bladder too long
bacterial infection
can hold 500 mL of urine
full bladder
can hold ~1000 mL or urine
distended bladder
what is the danger of a distended bladder
bladder can herniate or rupture