2.2 cardiac muscle dysfunction patholphysiology
1/97
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
98 Terms
What does it mean to have acyanotic defect
still circulating oxygenated blood through arteries (just mixed)
What does it mean to have cyanotic defect
deoxygenated/venous blood is circulated throughout the body
What are the 4 types of acyanotic defects
ventricular septal defect
atrial septal defect
patent ductus arteriosus
coarctation
Describe ventricular septal defect (VSD)
hole between ventricles
describe atrial septal defect (ASD)
hole between atria
describe patent ductus arteriosus (PDA)
extra vessel connection aorta and pulmonary a never disconnects after birth
Decribe coarctation
pinch in the aorta limiting flow out of heart, but still delivers the O2 blood
Why don’t individuals usually notice coarctation until adulthood
HTN arises to compensate for resistance
What are the 3 cyanotic defects
tetralogy
transposition
truncus arteriosus
Describe tetralogy
aorta is taking blood from both ventricles due to 4 defects
What are the 4 defects that combine to lead to tetralogy
VSD
narrowing of pulm artery
aorta lies just above VSD
R ventricular hypertrophy
describe transposition
great vessels are switched
describe truncus arteriosus
aorta and pulm arteries do not fully separate
What are the most commonly occluded arteries in CAD
LAD, RCA, and left circumflex artery
Why does CAD reduce EF
once muscle is damaged a scar forms. Scar reduces contractility
How can we check for a baggy/saggy heart on a lab
check BNP levels
What is a dilated cardiomyopathy
L ventricle is stretched leading to bad contractility
What is a hypertrophic cardiomyopathy
muscle wall of L ventricle have thickened (really good contraction, much smaller volume)
What is a restrictive cardiomyopathy
walls of LV have stiffened due to a metabolic dysfunction (no stretch= smaller volume and less efficient contractility)
What is a sarcomere made up of
actin and myosin filaments
What is the frank-starling law
Changed in contractility will shift the curve in relation to SV and LVEDV leading to positive and negative inotropic effects
What is a positive inotropic effect
Low SV and a high contractility
What is a negative inotropic effect
increased SV with low contractility
What is end diastolic volume (EDV)
blood in LV at end of diastole
What is end systolic volume (ESV)
blood left in the ventricle at the end of systole
what is the equation for ejection fraction (EF)
= (EDV-ESV)/EDV
What is EF
the amount of blood pumped out of the heart with each contraction
What is a normal EF
55-70%
What does HFpEF stand for
Heart failure preserved EF
At what phase does HFpEF occur
diastolic
What does HFpEF look like
stiff and thick chambers (hypertrophic cardiomyopathy)
What causes HFpEF
heart cant fill
What does HFrEF stand for
heart failure reduced EF
At what phase does HFrEF occur
systole
What does HFrEF look like
stretched and thin chambers (dilated cardiomyopathy)
What causes HFrEF
heart can’t pump
What EF correlates with HFpEF
>40%
What EF correlates with HFrEF
<30%
New York Heart Association (NYHA) heart failure classification of I
no limitations, asymptomatic during daily activities
New York Heart Association (NYHA) heart failure classification of II
slight limitation, mild symptoms with ordinary activities
New York Heart Association (NYHA) heart failure classification of III
moderate limitation, symptoms noted with minimal activity
New York Heart Association (NYHA) heart failure classification of IV
severe limitations, symptoms at rest
How many METs can we work a class I pt on the NYHA
6-10, exercise as normal
How many METs can we work a class II pt on the NYHA
4-6, may have lab value activity
How many METs can we work a class III pt on the NYHA
2-3, min activity
How many METs can we work a class IV pt on the NYHA
less than 2
What are common symptoms of Left-sided heart failure
Paroxysmal nocturnal dyspnea
elevated pulmonary capillary wedge pressure
pulmonary congestion
restlessness
confusion
orthopnea
tachycardia
external dyspnea
fatigue
cyanosis
What is the main problem with left-sided HF
trouble with O2 due to blood backup into lungs (cyanotic)
What is the main problem with right-sided HF
swelling due to back up into body
What is right-sided HF caused by
can come from severe LS or HTN of pulmonary artery OR secondary to chronic pulmonary problems
Common side effects of right-sided heart failure
fatigue
increased peripheral venous pressure
ascites
enlarged liver and spleen
distended jugular veins
anorexia and complaints of GI distress
weight gain
Another name for right-sided HF
cor pulmonale
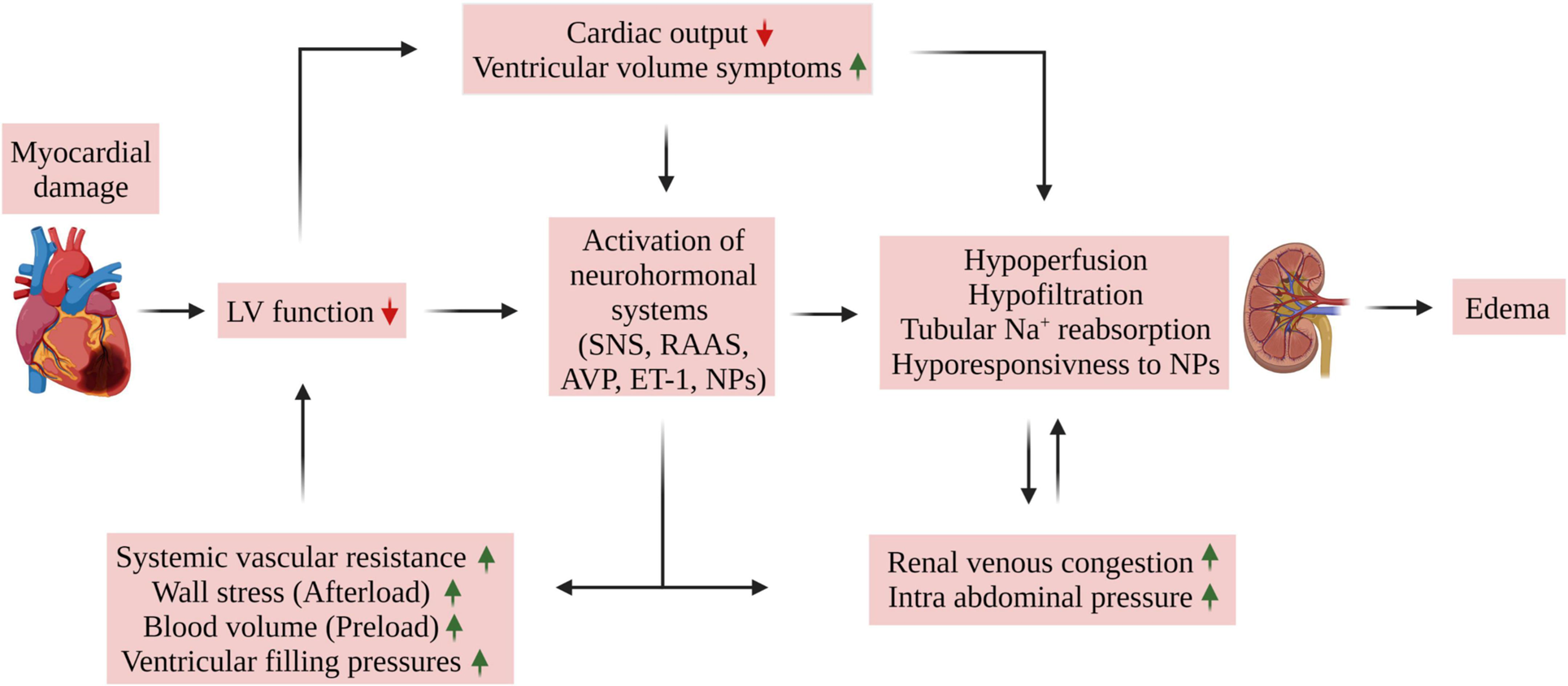
How does peripheral edema occur with myocardial damage
What are medical management options for HF pts
medications
AICD/pacemaker
dialysis/CRRT
intra-aortic balloon pump (IABP)
ventricular assistive device (VAD)
left ventricular muscle flaps
cardiomyoplasty
heart transplant
What are the strong CPG treatments
increase total daily PA
education on disease management
aerobic exercise training
upper and lower body resistance training
inspiratory muscle training (IMT)
neuromuscular electrical stimulation (NMES)
What are the guidelines for PA
150 mins per week of moderate intensity PA
75 mins per week of vigorous-intensity PA
How can we help educate on disease management
daily weight management
recognition of s/s of exacerbation
action planning using red-green-yellow CHF tool
following a nutrition plan
medication management/reconciliation
What weight differences are concerning for HF
>2-3lbs in 24 hrs or 5lbs in 3 days
What are the symptoms within the green zone
no shortness of breath
no swelling
no weight gain
no chest pain
no decrease in ability to maintain your activity
What should we do with pts when in the green zone
continue activity and therapy as tolerated
What are the symptoms within the yellow zone
weight gain of 2-3lbs in 24 hrs
increased cough
peripheral edema: increased distal extremity swelling
increase in SOB with activity
orthopnea (increase in the number of pillows needed)
What should we do with pts when in the yellow zone
symptoms may indicate an adjustment in medications and therefore warrants communication with the physician
What are the symptoms within the red zone
SOB at rest
unrelieved chest pain
wheezing or chest tightness at rest
paroxysmal nocturnal dyspnea: requiring to sit in chair to sleep
weight gain or loss of >5 lbs in 3 days
confusion
What should we do with pts when in the red zone
symptoms indicate overt decompression and an immediate visit to the emergency department or physician office
What are the moderate CPG treatments
high-intensity interval training for selected pts
combined resistance and aerobic training
combined IMT and aerobic exercise
What pts are able to participate in CPG
NYHA class II and III
What are the time guidelines for aerobic exercise training
20-60 mins
What are the intensity guidelines for aerobic exercise training
50%-90% of peak VO2/MET or peak work
What are the frequency guidelines for aerobic exercise training
3-5 times per week
What are the duration guidelines for aerobic exercise training
at least 8 to 12 weeks
What are the mode guidelines for aerobic exercise training
treadmill or cycle ergometer or dancing
What are the time guidelines for HIIT training
>35 total mins of 1-5 mins of high intensity (>90%) alternating with 1 to 5 minutes at 40%-70% active rest intervals, with rest intervals shorter that the work intervals
What are the intensity guidelines for HIIT training
>90 of peak VO2 or peak work
What are the frequency guidelines for HIIT training
2-3 times per week
What are the duration guidelines for HIIT training
at least 8-12 weeks
What are the mode guidelines for HIIT training
treadmill or cycle ergometer
What are the time guidelines for combined resistance and aerobic training
20-30 mins of resistance training added to aerobic exercise training
What are the intensity guidelines for combined resistance and aerobic training
2-3 sets per major muscle group, 60-80% 1RM
What are the frequency guidelines for combined resistance and aerobic training
3 times per week
What are the duration guidelines for combined resistance and aerobic training
at least 8-12 weeks
What are the time guidelines for inspiratory muscle (IMT) training
30 min/day or less if using higher training intensity
What are the intensity guidelines for inspiratory muscle (IMT) training
>30% MIP
What are the frequency guidelines for inspiratory muscle (IMT) training
5-7 days/wk
What are the duration guidelines for inspiratory muscle (IMT) training
at least 8-12 weeks
What are the time guidelines for combined IMT and aerobic exercise training
30 mins/day
What are the intensity guidelines for combined IMT and aerobic exercise training
>30% maximal inspiratory pressure
What are the frequency guidelines for combined IMT and aerobic exercise training
5-7 days/wk
What are the duration guidelines for combined IMT and aerobic exercise training
at least 8-12 weeks
What are the time guidelines for NMES training
30-60 minutes per session
What are the waveform guidelines for NMES training
biphasic symmetrical pulses at 15-50 Hz
What are the intensity guidelines for NMES training
On/off time 2/5 sec
pulse width for larger LE muscles = 200-700 ms
pulse width for smaller LE muscles = 0.5-0.7 ms
20-30% of MVIC
intensity to muscle contraction
What are the frequency guidelines for NMES training
5-7 days/week
What are the duration guidelines for NMES training
at least 5-10 weeks
What other conditions can result HF
HTN
CAD
cardiac arrhythmias
renal insufficiency
Heart valve abnormalities
cardiomyopathy
pericardial effusion
PE
pulmonary HTN
SCI
age-related changes
What is valvular heart disease
any valves could have stenosis, insufficiency, or both leading to needing a more forceful contraction which can cause hypertrophy
What are the effects of PE
can lead to R ventricular strain from high PA pressures
What should we do if pt is diagnoses with an acute PE
Emergency!! do not mobilize until pt receives medical treatment
What is pulmonary hypertension (PH)
mean pulmonary artery pressure (mPAP) >20 due to increased work to get blood from RV to lungs