GI Infections
1/59
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
60 Terms
is the GI tract sterile?
no because GI tract is topologically exterior
the GI tract is compartmentalized via gates aka…?
sphincters
what are the various defenses to microbes that exist in the GI tract?
barriers
flow
microbiotia
host defensive molecules
what barriers exist in the GI tract to defend against microbes?
Continuous epithelium
Mucus
Constant shedding of epithelial cells
what flow exist in the GI tract to defend against microbes?
saliva, drinking, peristalsis
what microbiota exist in the GI tract to defend against microbes?
Competition for binding sites and nutrients
Microbial Warfare via secreted toxins and surface attack complexes;
Bacteriophages (bacteria-specific viruses
what host defensive molecules exist in the GI tract to defend against microbes?
mouth: Lysozyme; Reactive Oxygen Species; Salivary Peroxidase.
Stomach: Hydrochloric acid (HCl); Digestive Enzymes.
Small Bowel: Bile Acids; Pancreatic juice (degradation enzymes); Antimicrobial Proteins, IgA (secretory antibody).
Large Bowel: Low molecular weight Fatty Acids; IgA
where are lysozymes found?
in secretions (tears, saliva, mucus, milk) and in neutrophils/macrophages
what do lysozymes do?
hydrolyzes carbohydrate strands of peptidoglycan (cell wall) of bacteria
lysozymes are resistant to
chemical stresses, heat, and proteases
lysozymes are multifunctional. what does this mean?
bind carbohydrates on bacteria
recruit antibodies and T-cells
kill even when active site is mutated
what is achlorhydria?
low hydrochloric acid [HCl] production in stomach
what is diverticula?
altered flow
what kind of cells make up most of the material in the colon and % of the mass of feces?
Bacterial
60%
Between 500 and 1000 different species live in the gut. But ~99% of the bacteria are from __ or so species
30
The average human body has ~10^13 cells, but ~__microbial cells live in our GI tract
10^14
What does the intestinal microbiota do?
• Immune stimulation
• Keeps out invaders (competition, direct killing)
• Role in nutrition (eg, vitamin K and biotin production)
• Source of infection (eg, following trauma)
Which one of the following is not a defensive property of the GI tract against intestinal pathogens?
A. Stomach acidity
B. Vitamin production by the gut microbiota
C. Flow of intestinal contents
D. Constant shedding of epithelial cells
E. Microbiota
B. Vitamin production by the gut microbiota
what is the most common stomach pathogen?
Helicobacter pylori
Helicobacter pylori: encounter/spread
Human Reservoir; Spread by Fecal-Oral Route and by Oral-Oral Route
Helicobacter pylori: entry
Motility and cork-screw shape allow it to penetrate mucus gel of stomach and colonizes stomach epithelium
Helicobacter pylori: spread
Can also colonize duodenum
Helicobacter pylori: multiplication
Must buffer pH to grow in stomach. Major mechanism is production of the enzyme Urease
Helicobacter pylori: damage
Ulcers; Secreted toxin and host inflammation damage mucosal layer; Chronic damage can lead to stomach cancer
(5th most common cancer, 4th most common cause of cancer deaths in the world; ~26,500 cases/yr in US)
Helicobacter pylori: outcome
Antibiotic therapy targeted at H. pylori
start 16
Non-typhoidal Salmonellosis: encounter
Oral ingestion in ~95% of cases;
~5% zoonotic (chickens)
Mostly sporadic cases; Infectious dose (ID50) varies (102-109 CFU)
Non-typhoidal Salmonellosis: spread
intracellular Pathogen. Usually localized replication in intestinal epithelium, but can spread deeper in the very young, elderly, or immunocompromised
Non-typhoidal Salmonellosis: outcome
Usually self-limiting gastroenteritis (4 to 7 d). ~5% of cases are invasive, usually in the immunocompromised (bloodstream, organs, bone, CFS)
Non-typhoidal Salmonellosis: entry
Acid-resistant, allowing passage through stomach.
Bacteria swim to epithelium in small and large intestine, adhere to cell via fimbriae, then trigger their endocytosis
Non-typhoidal Salmonellosis: spread
Intracellular Pathogen. Usually localized replication in intestinal epithelium, but can spread deeper in immunocompromised
Non-typhoidal Salmonellosis: multiplication
Multiplies Extensively within epithelium
Non-typhoidal Salmonellosis: damage
injects “effector” protein into host cells via two Type 3 Secretion Systems (T3SSs)
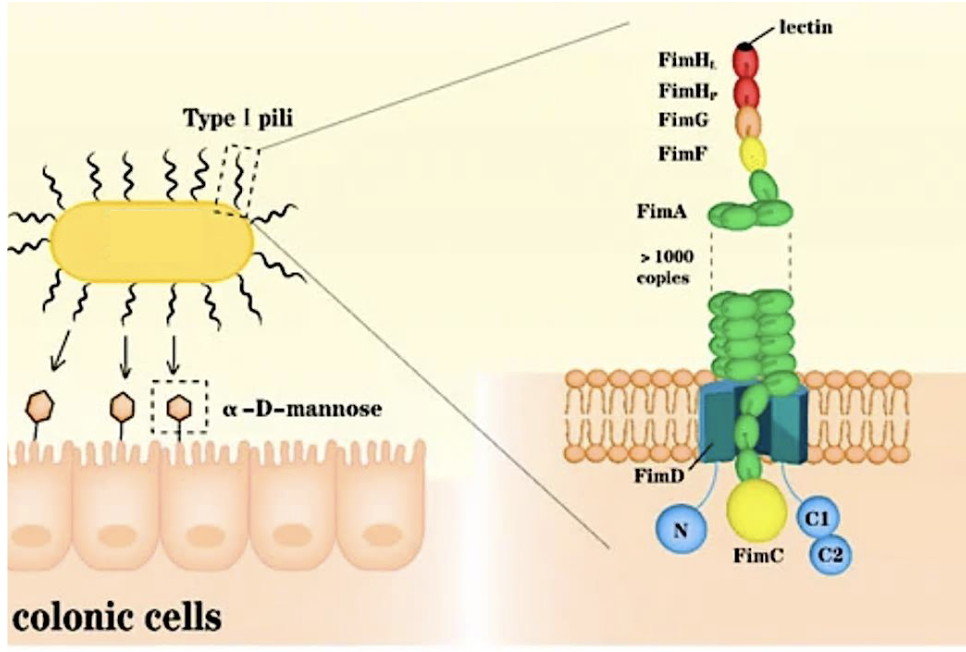
what mediates adherence by binding carbohydrates on host cells?
fibriae
what does T3SS-1 do?
manipulates host cytoskeleton to trigger endocytosis of Salmonella
what does T3SS-2 do?
manipulates host vesicle trafficking, causes cytotoxicity, and apoptosis
inhibits antigen presentation to T-cells and therefore adaptive immunity
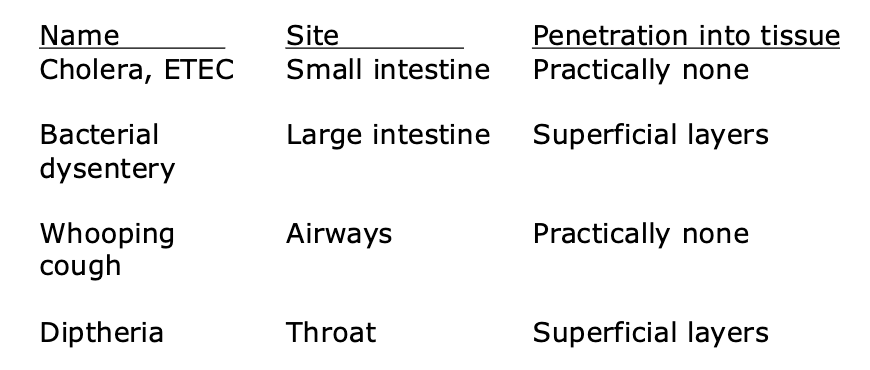
how do some pathogens cause disease without penetrating into tissue?
By secreting exotoxins, some that disseminate to tissues and organs
what are some bacteria that can cause serious disease without entering into the deep tissues of the body?
Harmless commensal, Small bowel pathogen (ETEC), Large bowel pathogen (STEC), or Urinary tract pathogen depending on which virulence genes the strain has. what is it?
E. coli
what is the E. coli pathogen of large bowel?
The invasive, shiga toxin-producing E. coli (STEC
STEC strain of E.coli can cause…?
kidney failure due to toxin production (orally ingested)
STEC: encounter
Undercooked contaminated meat products.
Contaminated vegetables.
Contaminated apple cidar.
Contamination usually occurs on or near farms with ruminants (e.g., cattle)
STEC: entry
Colonization of large intestine
STEC: mulitplication
Directly attaches to intestinal epithelium
STEC: spread
Colonization by bacteria is localized in colon, but damage is systemic due to toxin secretio
STEC: damage
1. Watery diarrhea
2. Bloody diarrhea
3. Hemolytic uremic syndrome (HUS)
why are some E.coli strains pathogenic?
virulence factors that cause damage to organs
extraintestinal colonization capability of some
what are the virulence factors that pathogenic strains of E. coli make?
Toxins (STEC, ETEC)
Factors promoting adherence to host cells
Factors promoting entry into epithelial layer of gut
what are examples of how some strains of E. coli virulence factors allow extraintestinal colonization?
urinary tract infections
meningitis
A 22-month-old child living in an area with unsafe drinking water became febrile and developed watery diarrhea. By the next day, there was less diarrhea, but blood in her stool. The stools were small in volume but increased in frequency and blood content. In the hospital the child was mildly dehydrated with hyperactive bowel sounds and a 40 ̊C fever. Stools contained a large number of white blood cells. The diagnosis was bacillary dysentery (shigellosis) and the child was given IV fluids to rehydrate and antibiotics. Culture of stool grew _________________ the most virulent of the Shigella species, which has the potential to cause severe damage to the large intestine.
Shigella dysenteriae,
what are the species of shigellosis and which is most/least severe?
Shigella dysenteriae (most severe)
Shigella flexneri
Shigella boydii
Shigella sonnei (least severe)
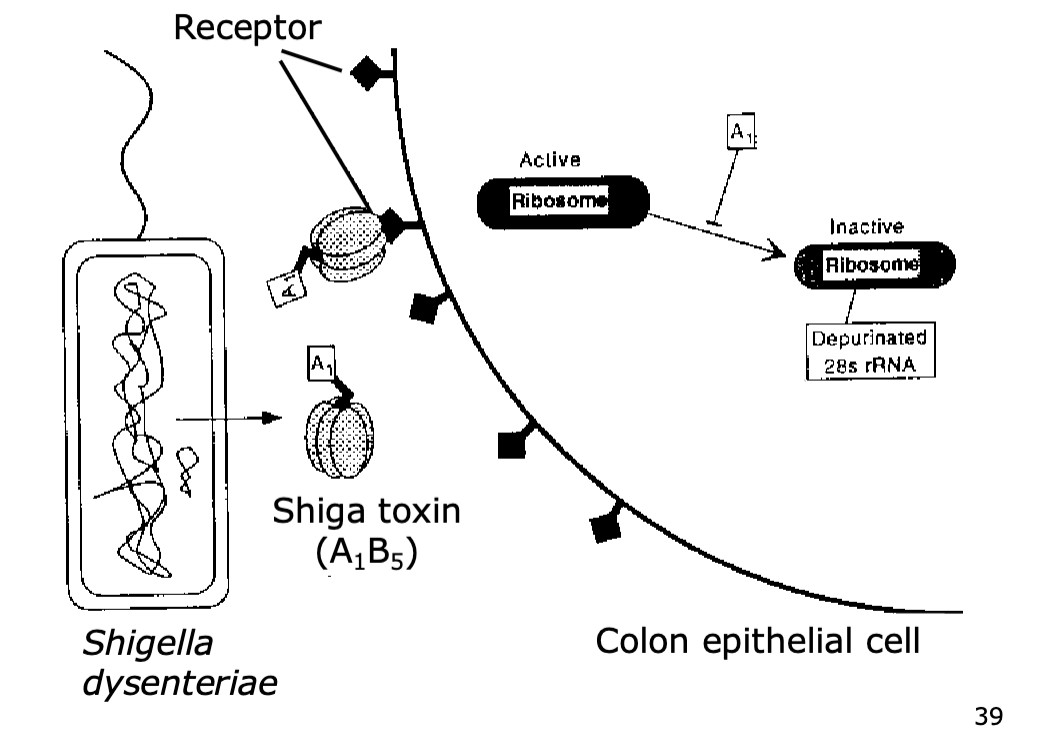
All Shigella species produce what toxin (same one produced by STEC), but to different levels?
Shiga
The more pathogenic strains also produce additional toxins
what type of toxin is shiga toxin?
AB subunit toxin
dysentery (shigellosis); encounter
dysentery (shigellosis); entry
Non-motile; Surface proteins mediate invasion into normally non-phagocytic colon epithelial cells
dysentery (shigellosis); spread
Intracellular pathogen; cell-to-cell spread; like Salmonella, it uses a T3SS to inject effector proteins into host cell. For Shigella, these trigger endocytosis, and lysis of the vacuolar membrane
dysentery (shigellosis); multiplication
Multiplies in cytoplasm of host cells. Spreads cell-to-cell, killing the cells, and ultimately causing ulceration of the epithelium
dysentery (shigellosis); damage
The local ulcerations in colonic epithelium are caused by bacterial toxins and host inflammatory reaction
dysentery (shigellosis); outcome
Rarely severely dehydrating;
Antibiotics are crucial for cases with fever and/or dysentery;
Problem with drug-resistance;
Malnutrition can result from damaged colon
Which one of the following statements concerning diarrheal pathogens is false?
A. A1B5 subunit toxins are made by some but not all intestinal pathogens.
B. Type 3 Secretion Systems (T3SSs) translocate effector proteins from the bacterial cytoplasm into the host cell cytoplasm.
C. Pathogens must invade into deep tissues to cause disease.
D. Many intestinal pathogens are spread via the fecal-oral route.
E. Rehydration therapy is important in the treatment of watery diarrhea.
C. Pathogens must invade into deep tissues to cause disease.