transport in humans
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
double circulatory system
the blood flows through the heart twice in one circuit
ensures that the blood is pumped at low pressure to the lungs so that the blood can be properly oxygenated and the oxygenated blood can be pumped out at high pressure to all body cells at a fast rate
double circulatory system consists of a pulmonary circulation and a systemic circulation:
- pulmonary circulation (lungs): carries oxygenated blood from the lungs to the heart and deoxygenated blood from heart to the lungs
- systemic circulation (rest of the body): carries oxygenated blood from the heart to the rest of the body and deoxygenated blood from the rest of the body to the heart
main veins
- pulmonary vein
- vena cava (superior and inferior)
- hepatic vein
- hepatic portal vein
- renal vein
main arteries
- pulmonary artery
- aortic arch
- hepatic artery
- renal artery
blood
1. plasma (55%)
2. red blood cells (eruthrocytes)
3. white blood cells (leukocytes)
4. platelets
main functions of blood
1. to transport oxygen, food substances (e.g. glucose, amino acids, fats and vitamins), waste material (e.g. carbon dioxide), hormones, heat from one part of the body to another
2. protect the body by preventing the entry of foreign bodies and fighting infections
plasma
- consists of 90% water and 10% dissolved substances
- transports mineral ions, digested food substances, urea, carbon dioxide, hormones, vitamins, plasma proteins and blood cells around the body
red blood cells (erythrocytes)
- transports oxygen from the lungs to other parts of the body
- structure:
- haemoglobin (red pigment) present in cells
- absence of nucleus
- circular and biconcave shape
- elastic and flexible cell surface membrane
haemoglobin (red pigment) present in cells
- binds reversibly to oxygen to form oxyhaemoglobin, which helps to transport oxygen in the red blood cell around the body
- each molecule of haemoglobin can bind up to four molecules of oxygen
- haemoglobin binds to oxygen in places where oxygen concentration is high, but readily releases oxygen in places where oxygen concentration is low
absence of nucelus
more space available for more haemoglobin to be packed inside the cell cytoplasm and more oxygen to be transported per red blood cell
circular and biconcave shape
increases the surface area to volume ratio of the cell, thus allowing quicker diffusion of oxygen in and out of the cell
elastic and flexible cell surface membrane
cell can change its shape (e.g.: bell shape) when squeezing through small capillaries
leukocytes (white blood cells) - in topic 4
- macrophages
- neutrophils
- lymphocytes
lymphocytes - produce antibodies
1. destroying bacteria by attaching to them and causing the bacteria surface membrane to rupture
2. cause the bacteria to agglutinate so that they can be easily ingested by the phagocytes
3. neutralise the toxins produced by bacteria
4. attach the viruses and prevent them from binding to the host cell
phagocytes -> macrophages and neutrophils
engulfing and digesting foreign bodies/pathogens
platelets (thrombocytes) → blood clotting
- play an important role in blood clotting by forming "sticky plugs" at wound sites
- importance of blood clotting:
- prevents excessive loss of blood from the wound
- prevents further entry of pathogens (virus and bacteria) through the wound
mechanism of blood clotting
1. damaged tissue and platelets
- produce thrombokinase (enzyme)
2. prothrombin
- converted to thrombin (enzyme)
- catalysed by thrombokinase and calcium ions
3. fibrinogen
- converted to fibrin threads (insoluble)
- fibrin threads form a mesh to trap blood cells and form a clot
- catalysed by thrombin (enzyme)
ABO blood groups
- named after the antigen: a protein marker found on the cell surface membrane
- when donating blood, only red blood cell (antigen) is donated from donor to recipient
blood group A
- there are Anti-B antibodies in the plasma
- there are antigen A on the red blood cells
blood group B
- there are Anti-A antibodies in the plasma
- there are antigen B on the red blood cells
blood group AB
- there are no Anti-A and Anti-B antibodies in the plasma
- there are A and B antigens on the red blood cells
- universal recipient
blood group O
- there are Anti-A and Anti-B antibodies in the plasma
- there are no A and B antigens on the red blood cells
- universal donor
agglutination
- clumping of red blood cells which is fatal
- occurs when:
- anti-A antibodies in the plasma bind with antigen A on the red blood cells
- anti-B antibodies in the plasma bind with antigen B on the red blood cells
- occurs in the recipient
blood vessels
- arteries
- veins
- capillaries
arteries
blood vessels that carry blood away from the heart
all arteries transport oxygenated blood except the pulmonary artery (brings deoxygenated blood from heart to the lungs)
blood flow in arteries is rapid and under high pressure
thick muscular and elastic walls enable the arteries to withstand the high pressure of blood flowing through it
thick elastic walls allow the arteries walls to stretch and recoil to push the blood along it in spurts, maintaining the high pressure of blood flowing through the artery → high rate of blood flow
arteries branch to form smaller arteries called arterioles
arterioles branch to form many tiny blood vessels called capillaries
veins
- blood vessels that carry blood towards the heart
- all veins carry deoxygenated blood (more waste products) except the pulmonary artery (oxygenated blood from the lungs to heart)
- blood flow in veins is slow and at low pressure
- they have relatively thinner muscular and elastic walls as the pressure of the blood flowing through it is at low pressure
- semilunar valves are present to prevent the backflow of blood in the vein
- the valves ensure that blood flows in one direction in the vein only (unidirectional flow of blood)
- veins are located between large muscles of body
- the contraction of the skeletal muscles (e.g. leg muscles) squeeze the veins and push the blood along, up towards the heart
- before the capillaries leave an organ or tissue, they unite to form small veins called venules
- venules joined to form larger blood veins
capillaries
- microscopic blood vessels that connect the arteries to veins and are found between cells of most tissues
- capillary walls are only one-cell thick and are partially permeable so that certain substances are able to diffuse through their walls quickly
- capillaries branch repeatedly to provide a large surface area for the quick exchange of substances between blood and tissue cells
transfer of materials between capillaries and tissue fluids
- oxygen and soluble food substances (e.g. glucose) diffuse quickly through the wall of capillaries from the blood plasma to the tissue fluids surrounding body cells, as the blood moves along the capillaries, down their concentration gradient
- carbon dioxide and other waste products (e.g. urea) diffuse from the body cells into the tissue fluids, and subsequently into the blood plasma, to be carried away to various organs to be removed from the body, down their concentration gradient
heart
- the heart is a muscular organ that functions to pump blood around the body
- consists of mainly cardiac muscles which contract and relax to circulate blood through the blood vessels
4 chambers of the heart
- 2 atria (singular: atrium) → upper chambers
- have relatively thinner walls to force blood into the ventricles
- 2 ventricles → lower chambers
- right ventricle: has relatively thick muscular walls to move blood into the pulmonary circulation
- left ventricle: has thicker muscular walls than the right ventricle as it has to pump blood into systemic circulation
sides of the heart
- the right side of the heart receive deoxygenated blood (low concentration of oxygen and high concentration of carbon dioxide) from the body (except lungs) and pumps it to the lungs
- the left side of the heart receive oxygenated blood (high concentration of oxygen and low concentration of carbon dioxide) from the lungs and pump it to all parts of the body (except lungs)
median septum
prevents oxygenated blood in the left side from mixing with deoxygenated blood in the right side
valves
- ensure that blood flows unidirectionally (in one direction), hence preventing back-flow of blood. the valves present are:
- semilunar valves (found in pulmonary artery and aorta)
- atrio-ventricular valves
- bicuspid valve (between left atrium and left ventricle)
- tricuspid valve (between right atrium and right ventricle
why are the walls of the ventricles thicker and more muscular than the walls of the atria
the muscular walls of ventricle contract to pump blood to the rest of the body (a further distance), so the walls are thicker and more muscular to exert a higher pressure, ensuring blood reaches all areas of the body. however, the muscular walls of atria contract to pump blood only to the ventricles (short distance), so the walls are thinner and less muscular, as blood can be pumped at a lower pressure
cardiac cycle
- refers to the events that occur during a single heartbeat
- the systole phase → contraction of the walls of the chambers of the heart
- the diastole phase → relaxation of the walls of the chambers of the heart
atrial systole → both muscular walls of atria contract
- muscles surrounding both atria contract, forcing blood into the ventricles
- the tricuspid and bicuspid valves open to allow blood to pass through
- semilunar valves close to prevent backflow of blood into the vena cava and pulmonary vein
- very low pressure in ventricle: very little blood and relaxed
- atria (higher pressure) → ventricle (lower pressure)
ventricular systole → both muscular walls of ventricles contract
- muscles surrounding both ventricles contract and the pressure in the ventricles rises
- blood from the ventricles are pumped out of the heart, into the pulmonary artery and aorta
- the tricuspid and bicuspid valves close to prevent backflow of blood into the atria
- the semilunar valves in the pulmonary artery and the aorta open to allow the blood to pass through
- a 'lub' sound is produced by the closure of these valves
- ventricle (higher pressure) → pulmonary artery and aorta (lower pressure)
diastole → both the atria (during ventricular systole) and ventricles relax
- muscles surrounding both atria and ventricles relax and the pressure in all chambers fall
- blood enters the relaxed atria and ventricles
- the tricuspid and bicuspid valves open to allow blood to pass through
- the semilunar valves in the pulmonary artery and the aorta close to prevent backflow of blood into the ventricles
- a 'dub' sound is produced by the closure of these valves
coronary heart disease
the coronary arteries: supply oxygen and nutrients in the heart muscles
may become narrowed and eventually, blocked by a build-up of fatty deposits (plaque) containing cholesterol, resulting in coronary heart disease
if a coronary artery is blocked, the blood supply to part of the heart muscle is cut off → the heart muscle cells are deprived of oxygen and nutrients, and cannot respire and dies
the part of the heart cannot continue to contract, causing a heart attack
causes of coronary heart disease
1. diet high in cholesterol and saturated animal fats
2. lack of exercise → sedentary lifestyles increase the risk of coronary heart disease
3. stress and smoking
- increases blood pressure
- narrowing of artery walls through buildup of plaque
preventive measures against coronary heart disease
1. diet: reduce intake of cholesterol and saturated animal fats
2. regular physical exercise
- strengthens heart
- maintains elasticity of aterial walls
3. manage stress and avoid smoking
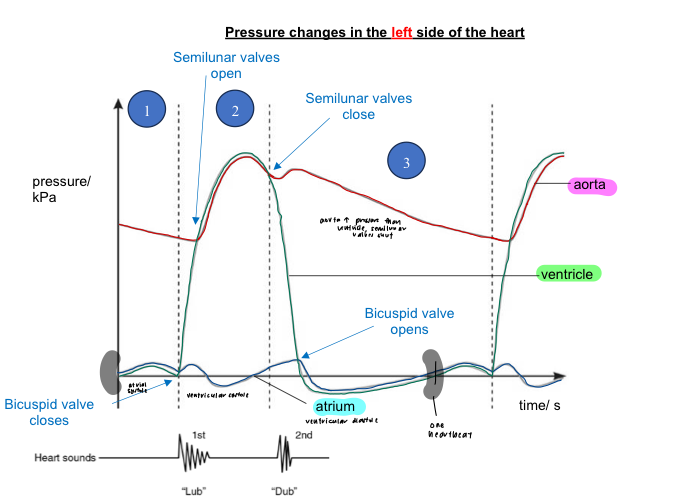
pressure changes in the left side of the heart
1. atrial systole
atrial pressure is higher than ventricular pressure
bicuspid valve is open to allow blood to flow
blood therefore flows from left atrium to left ventricle, down its pressure gradient
aortic pressure higher than ventricular pressure
semi-lunar valves close to prevent backflow of blood from aorta into left ventricle
2. ventricular systole
ventricular pressure rises such that it is higher than aortic pressure
semi-lunar valves open to allow blood to flow through
blood flows from left ventricle into the aorta
meanwhile, atrium undergoes diastole and begins to be filled with blood
bicuspid valve closes to prevent backflow of blood from ventricle to atrium (‘lub’ sound)
3. ventricular diastole
ventricular pressure decreases until it is lower than aortic pressure
semi-lunar valves close to prevent backflow of blood from aorta into left ventricle (‘dub’ sound)
ventricular pressure decreases further until it is lower than atrial pressure
bicuspid valve opens to allow blood to flow
blood therefore flows from left atrium to left ventricle, down its pressure gradient
the cycle repeats