ICU EKG Rhythms
1/14
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
15 Terms
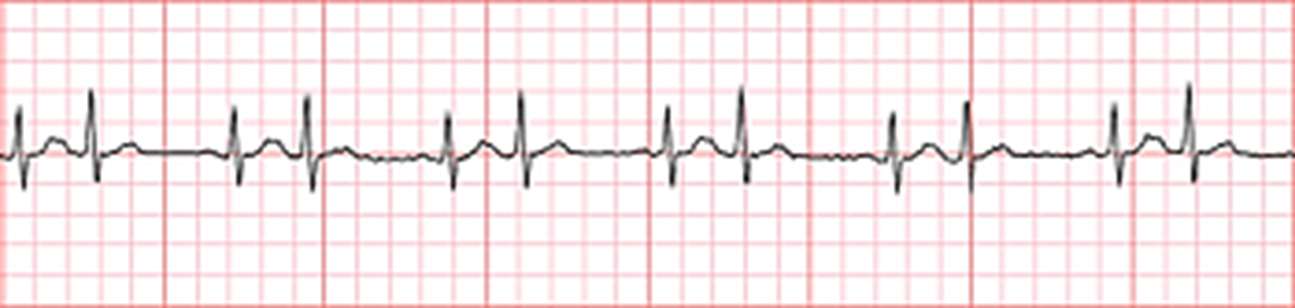
Premature atrial contraction (PAC)
Causes:
stimulants (caffeine or tobacco)
myocardial ischemia
electrolyte abnormalities
myocardial hypertrophy
Interventions:
find the root cause
vital sings, SOB, s/s of decreasing CO
replace electrolytes
typically asymptomatic
may precede afib

Atrial flutter
Causes:
lung disease
ischemic heart disease
hyperthyroidism
hypoxemia
chf
ETOH abuse
electrolytes
Interventions:
vital signs, s/s of cardiac ischemia and low CO
loss of atrial kick (20%)
DO NO let pt become hypovolemic
BLOOD STASIS→ANTICOAGULANTS
cardioversion (anti before and after)
medications: depends on rate/tolerance (same as afib)
ablation, MAZE

Atrial fibrillation
Causes:
ischemic/valvular heart disease
hyperthyroidism
hypoxemia
chf
electrolytes
Interventions:
vital signs, s/s of cardiac ischemia and low CO
loss of atrial kick (20%)
DO NO let pt become hypovolemic
BLOOD STASIS→ANTICOAGULANTS
cardioversion (anti before and after)
medications: depends on rate/tolerance (same as afib)
ablation, MAZE
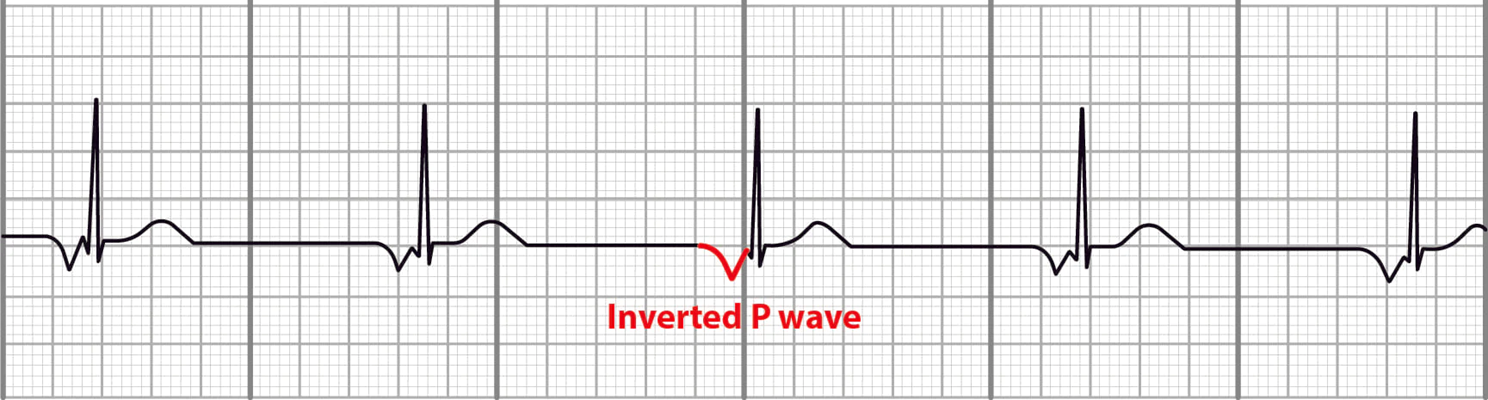
Junctional rhythms
Causes:
any disease or condition affecting the sinus node
can be valvular related/post valve or heart surgery
ischemic heart disease
digoxin
Interventions:
vs, s/s of cardiac ischemia/low CO
typically no tx unless symptomatic (atropine, trans pacing, dopamint)
(dopamine/atropine to restore AV condition)
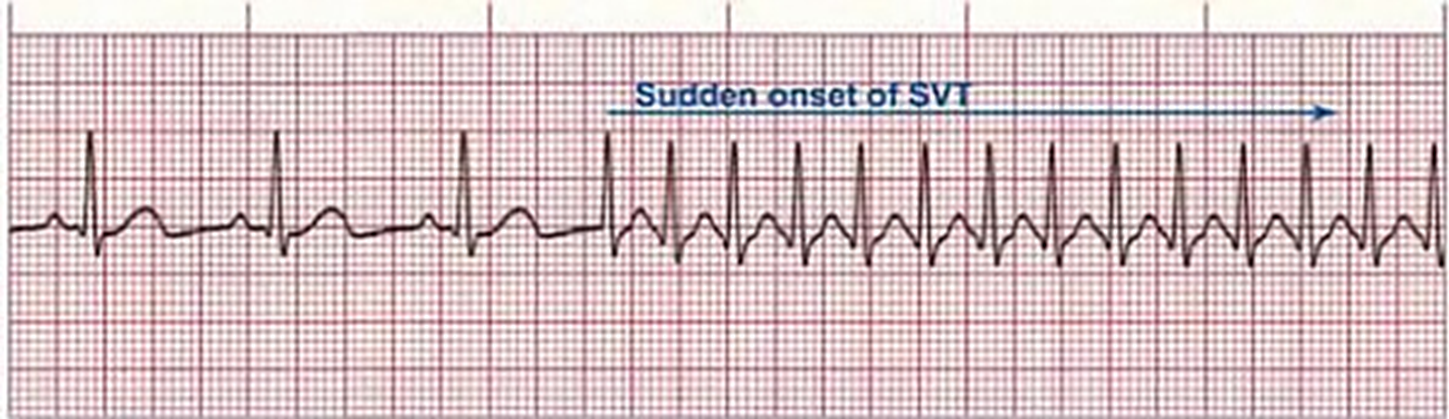
Paroxysmal supraventricular tachycardia (PSVT)
Causes:
can occur in healthy individuals without heart disease
stimulants, catecholamines
electrolytes
chf
Interventions:
vs, s/s cardiac ischemia/low CO
may be abated using vagal maneuver (if stable)
heart rate >150 and symptomatic→ emergent cardioversion
meds: adenosine (2nd/unstable)→ restart the heart
EP study to find cause
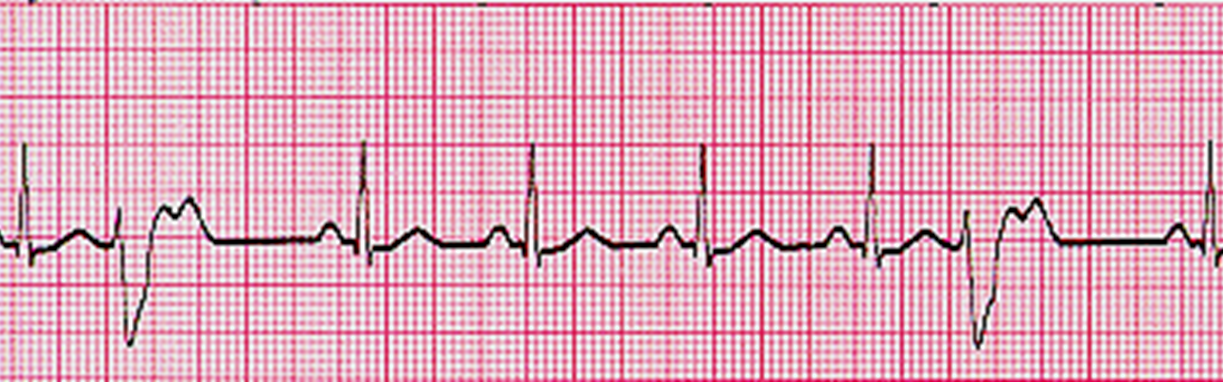
Premature ventricular contraction
three or more is non-sustained vtach
Causes:
hypoxemia
ischemic heart disease
hypokalemia/magnesemia
acid-base imbalance
increased catecholamines
Interventions:
vs, s/s cardiac ischemia/low CO
treat the cause of PVC and correct/eliminate
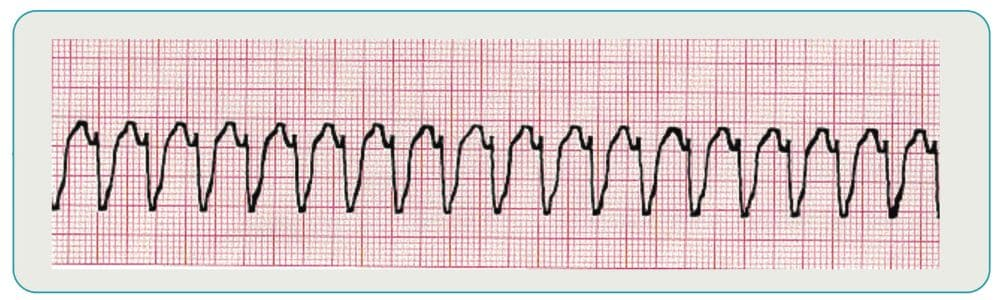
Ventricular tachycardia
Causes:
hypoxemia
acid-base imbalance
exacerbation of heart failure
ischemic heart disease
cardiomyopathy
valvular heart disease
electrolyte imabalance
Interventions:
DETERMINE A PULSE FIRST
pulseless→ emergency resuscitation
pulse: vs, s/s cardiac ischemia/low CO
electrolyte/acid base correction
meds: amiodarone, lidocaine
→both are antiarrythmics
cardioversion in emergency
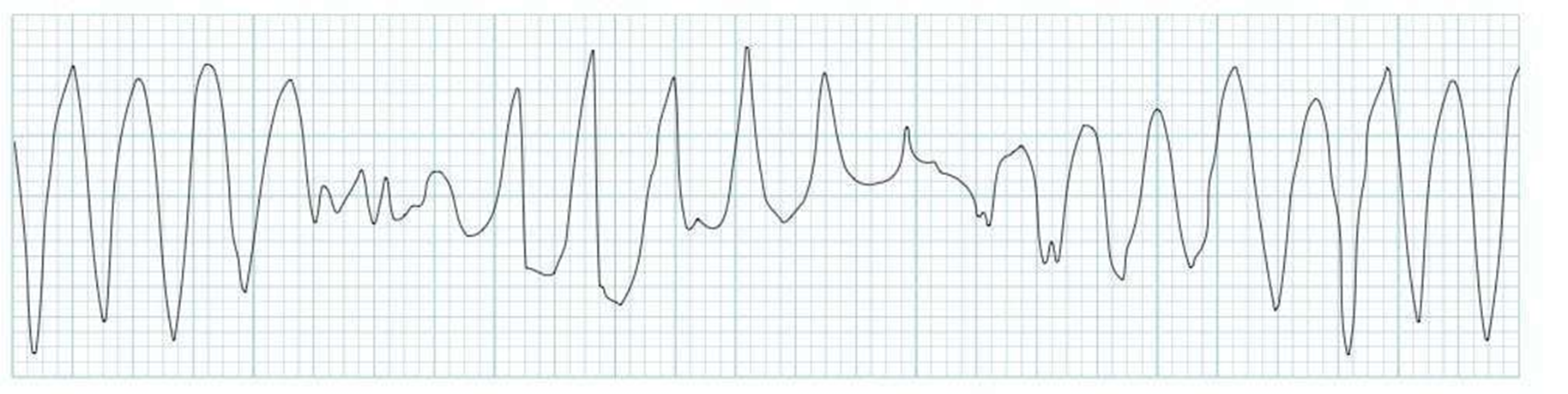
Torsades
type of VT causes by elongated QT
check for pulse→ tx is mag, amiodarone, or lidocaine
cardioversion
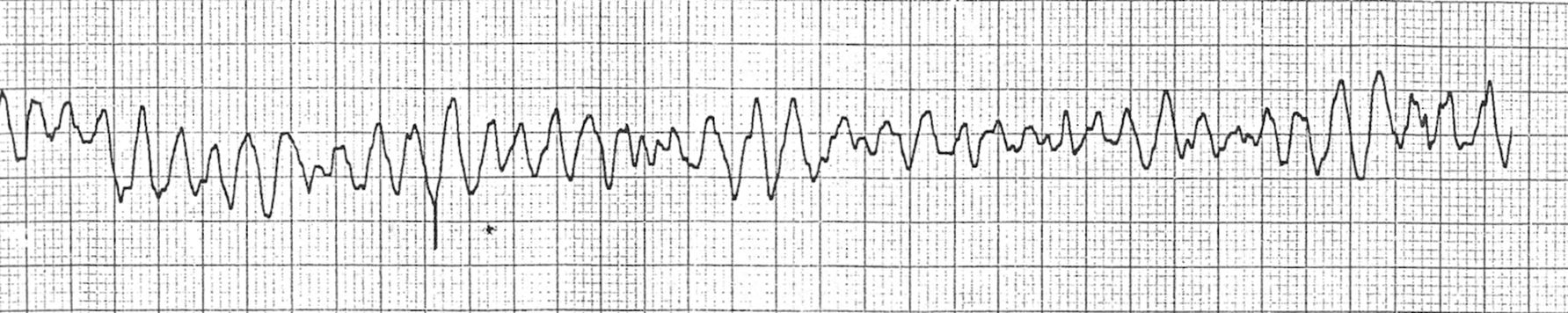
Ventricular fibrillation
Causes:
hypoxemia
acid base imbalance
exacerbation of heart failure
valvular heart disease
electrolyte abnormalities
Interventions:
PULSE FIRST
start emergency resuscitation→ immediate dfib
electrolyte/acid base correction
meds: epi, atropine, amiodarone, sodium bicarb
find and treat the cause
Asystole
no pulse- no CO
cardiac arrest
causes: preceded by another dysrhythmia (VF)
tx: BLS/ACLS

1st degree AV block
“if R is far from P, you have first degree”
Causes:
aging
ischemia valvular related
ischemic heart disease
Interventions:
typically no treatment
trend PR interval and note if it elongates further
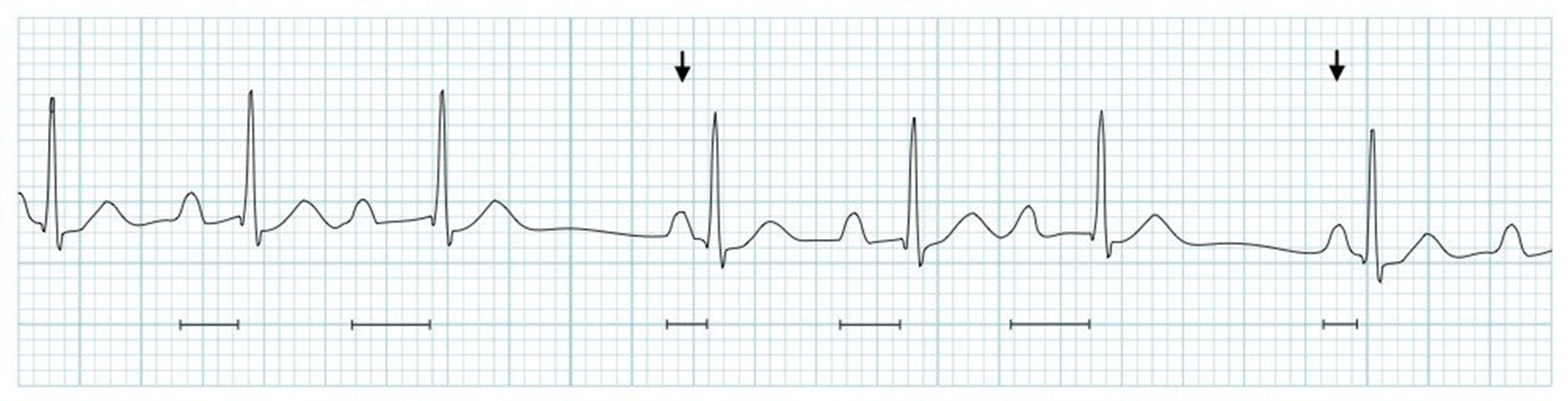
2nd degree type 1 AV block (wenckebach)
“longer, longer, longer, DROP, then you have wenckebach
Causes:
drugs
aging
acute inf wall MI
ischemic heart disease
digitalis toxicity
right ventricular infarct
Interventions:
well treated by pts unless drops are frequent
find and treat cause
typically no tx
trend PR interval
may require pacemaker

2nd degree type II AV block
occurs lower in bundle of HIS or branches
can progress→ 3rd degree
Causes:
heart disease
acute inf wall MI
ischemic heart disease
increased vagal tone
right ventricular infarct
Interventions:
vs, s/s cardiac ischemia and low CO
find and treat cause
trend P and QRS
may require pacemaker or trans pacing in symptomatic pts
meds: atropine if symptomatic or slow
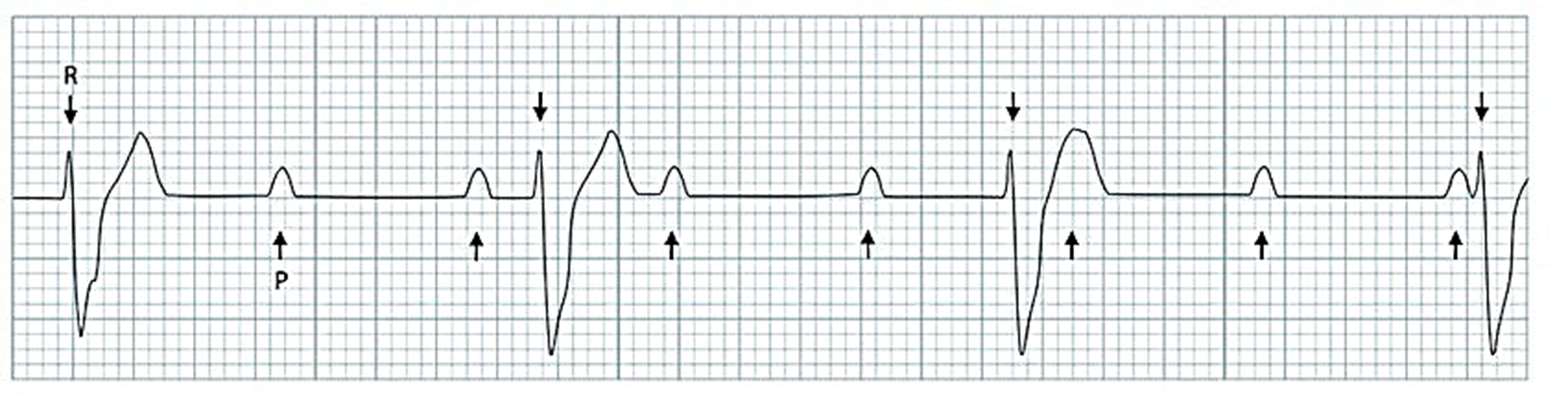
3rd degree AV block (COMPLETE)
no atrial impulses through AV node→ a and v beat independently
P and QRS not synced
“if Ps and Qs disagree you have 3rd degree”
Causes:
heart disease
acute MI
ischemic heart disease
conduction system disorder
Interventions:
vs, s/s low CO and cardiac ischemia
find and treat cause
REQUIRES pacemaker or trans pacing
trend P and QRS
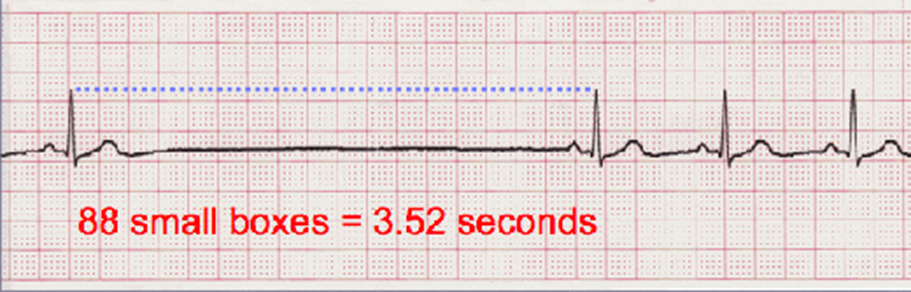
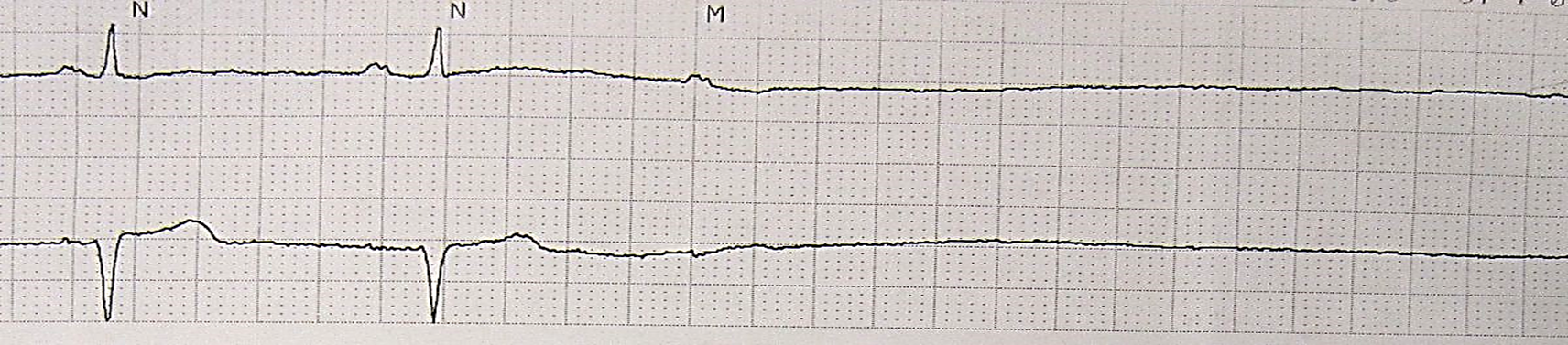
Sinus pause/arrest (atrial standstill)
SA node does not generate any signal→ AV is not stimulated
2 or <2 second pauses are normal (sleeping)
>2 seconds is not normal
Causes:
acute infection
SA fibrosis
increased vagal tone
digoxin and salicylates toxicity
beta blocker OD
Ca channel blockers
myocarditis
MI
sick sinus syndrome
Interventions:
vs, s/s cardiac ischemia/low CO
find and treat cause
FALL RISK- syncope
atropine or epi along with pacemaking
trend P and QRS interval