Kisner Chap 11
1/77
Earn XP
Description and Tags
bone stuff
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
78 Terms
This is the limitation of a joint without inflammation
Arthrosis
Age of onset for RA
between age 15 and 50
Age of onset for OA
Usually after age of 40
This disease usually develops slowly over many years in response to mechanical stress
OA
This disease may develop suddenly, within weeks or months
RA
The manifestations of RA are?
Inflammatory synovitis and irreversible structural damage to cartilage and bone
The manifestations of OA are?
Cartilage degradation, altered joint architecture, osteophyte formation
True or False:
OA usually affects a many joints and is usually symmetrical
False:
Few joints, Asymmetrical
True or False:
RA affects many joints and is usually bilateral
True
Which joints does OA usually affect?
DIP, PIP, 1st CMC
Cervical and lumbar spine
Hips, Knees, 1st MTP
Which joints does RA usually affect?
MCP and PIP of hands, wrists, elbows, shoulders
Cervical spine
MTP, talonavicular and ankle
How long does morning stiffness last for OA according to Kisner (7th edition)
<30 mins
True or False:
OA and RA can have systemic s/sx
False:
Only RA has systemic s/sx
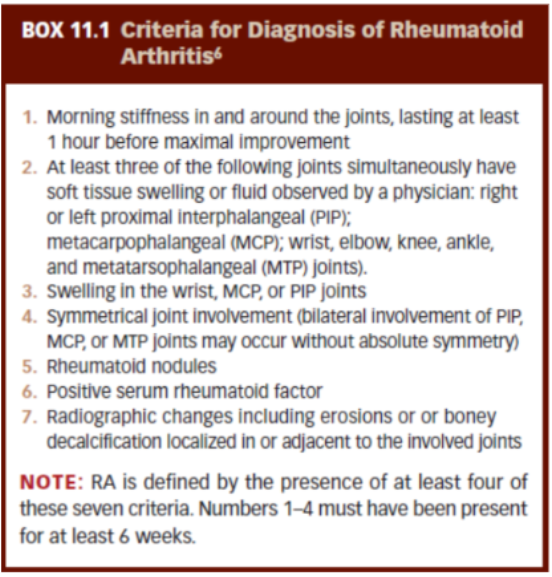
Review Criteria for classification of RA
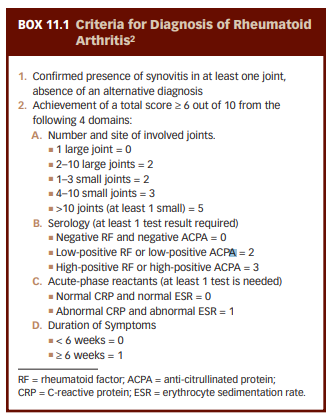
Review Criteria for classification of RA (PPT)
RA is characterized by symmetric, erosive synovitis with periods of ________ and _________
exacerbation (flare) and remission
True or False:
In RA, joints are characteristically involved with early inflammatory changes in the synovial membrane, central portions of the articular cartilage, and subchondral marrow spaces.
False:
peripheral portions of the articular cartilage
True or False:
With progression of the RA, cancellous bone becomes exposed. Fibrosis, ossific ankylosis, or subluxation may eventually cause deformity and disability
True
When using joint mob for treating RA, which grades are used to inhibit pain and minimize fluid stasis?
Grades 1 and 2
Management Guidelines for RA (Active disease period)
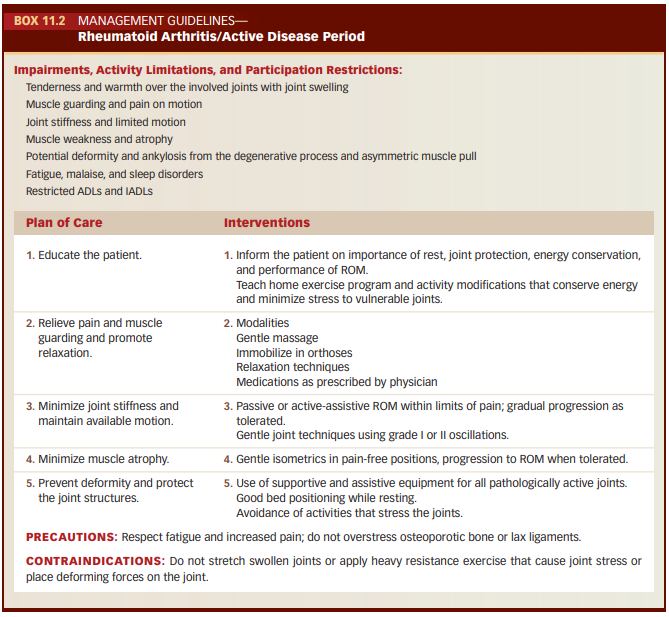
Principles of joint protection and energy conservation

True or False:
With degeneration dt OA, there may be capsular tightness as a result of bone remodeling and capsule distention, leading to hypermobility or instability in some ranges of joint motion.
False
capsular laxity
These nodes are common OA, develops in the DIP joints
Herberden’s Nodes
Which nodes develop in the PIP jts. during OA
Bouchard’s Nodes
True or False:
In the late stages of OA pain usually occurs because of excessive activity and stress on the involved joint and is relieved with rest.
False:
Early stages
Management Guidelines for OA:
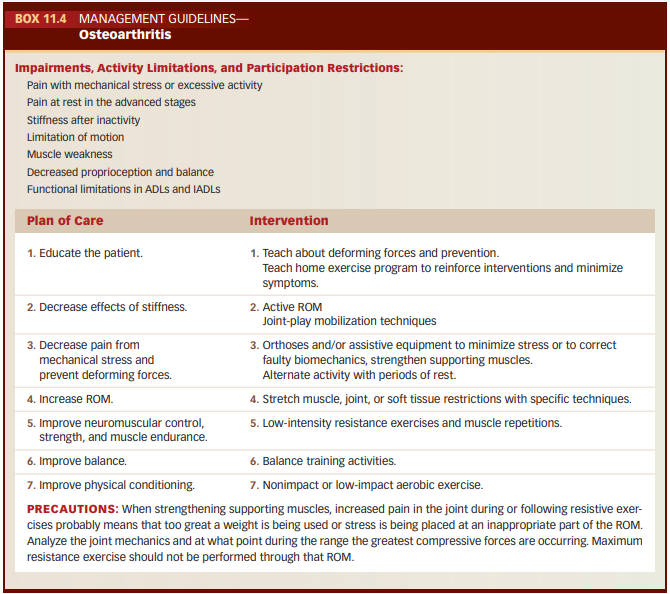
In OA, pain that cannot be managed with activity modification and analgesics is usually an indication for _____________
surgical intervention
True or False:
Nontraditional forms of exercise, such as tai chi, have been found to be effective for improving balance in patients with OA.1
True
True or False:
When prescribing aerobic conditioning to an OA patient, jogging is a good exercise to prescribe.
False:
Avoid activities that cause repetitive intensive loading of the joints, such as jogging and jumping.
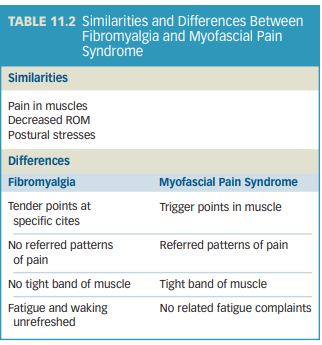
Individuals with ____ process nociceptive signals differently while individuals with _____ have localized changes in the muscle
Individuals with Fibromyalgia process nociceptive signals differently while individuals with Myofascial pain syndrome have localized changes in the muscle
True or False
Fibromyalgia is a chronic condition characterized by widespread pain that affects multiple body regions plus the axial skeleton and that has lasted for more than 5 months.
False:
More than 3 months.
How many tender points at specific sites throughout the body does patients with FM have?
11 of 18 tender points
True or False:
Some symptoms that FM has in common with MPS are nonrestorative sleep, morning stiffness and fatigue with subsequent diminished exercise tolerance.
False:
These symptoms are only found in patients with FM
Similarities and differences of FM and MPS
Prevalence of FM:
Which gender (biological) is more affected?
Which gender (biological) reports longer durations of symptoms?
At what age can you get FM?
Does the prevalence increase or decrease with age?
Which gender (biological) reports more pain intensity?
Prevalence of FM:
Female
Male
Any age but usually appear during early to middle adulthood. (usually 18)
Yes
Female
True or False:
For many of those diagnosed with FM, the symptoms develop after physical trauma such as a motor vehicle accident or a viral infection.
True
In FM, Pain is usually described as ________ in origin
Muscular
In, FM, predominantly reported in which areas?
scapula, head, neck, chest, and low back
True or False:
In FM, there is a significant fluctuation in symptoms. Some days an individual may be pain free, whereas other days the pain is markedly increased.
True
Individuals with FM have a higher incidence of:
tendonitis
headaches
irritable bowel
temporal mandibular joint dysfunction,
restless leg syndrome
mitral valve prolapse
anxiety
depression
memory problems.
Factors that affect the severity of FM symptoms:
Environmental stresses
Physical stresses
Emotional stresses
When managing FM, which type of exercises can reduce the common symptoms of FM
Aerobic exercise
Additional interventions for FM include:
Prescription medication
Over-the-counter medication
Instruction in pacing activities, in an attempt to avoid fluctuations in symptoms
Cognitive behaviour therapy
Avoidance of stress factors
Decreasing alcohol and caffeine consumption
Diet modification
Manual therapy
a hyperirritable area in a tight band of muscle.
trigger point
The pain from trigger points is described as?
dull, aching, and deep.
The trigger points may be ______ (producing a classic pain pattern) or _____ (asymptomatic unless palpated)
The trigger points may be active (producing a classic pain pattern) or latent (asymptomatic unless palpated)
This is defined as a chronic, regional pain syndrome with the hallmark classification being trigger points in a muscle that have a specific referred pattern of pain, along with sensory, motor, and autonomic symptoms.
Myofascial Pain Syndrome
Additional impairments of MPS:
Decreased ROM (when muscle is stretched)
Decreased muscle strength
Increased pain when stretching muscles
Treatment of MPS consists of 3 components
Correct chronic overload
Eliminate the trigger point
Contract-relax-passive & Contract-relax-active stretching
Trigger point release
Spray and stretch
Dry needling or injection
Modalities
Strengthen muscle
Disease of bone that leads to decreased mineral content and weakening of the bone. This weakening may lead to fractures.
Osteoporosis
Women more affected than men
The diagnosis of osteoporosis is determined by the T-score of a bone mineral density (BMD) scan.
Normal: __________
Osteopenia: __________
Osteoporosis: __________
The diagnosis of osteoporosis is determined by the T-score of a bone mineral density (BMD) scan.
Normal: –1.0 or higher
Osteopenia: –1.0 to –2.4
Osteoporosis: –2.5 or less
Cells in bone called _______ resorb bone, especially if calcium is needed for particular body functions and not enough is obtained in the diet
osteoclasts
The cycle of osteoclastic and osteoblastic activity are balanced until when?
Third decade of life
With increasing age, there is a shift to greater resorption
For women, resorption is accelerated during _______ owing to the decrease in estrogen.
menopause
Recommendations for Exercise for osteoporosis:
Aerobic
Frequency?
Intensity?
5 or more days per week
30 mins mod intensity or 20 mins vigorous intensity
3 short bouts of 10 mins per day is acceptable
Recommendations for Exercise for osteoporosis:
Resistance
Frequency?
Intensity?
2-3 days per week with rest days in between
8-12 RM
True or False:
When prescribing exercise to osteoporotic patients, flexion activities and exercise, such as supine curl-ups and sit-ups, as well as the use of sitting abdominal machines, should be avoided.
True
Stress into spinal flexion increases the risk of a vertebral compression fracture.
types of fractures:
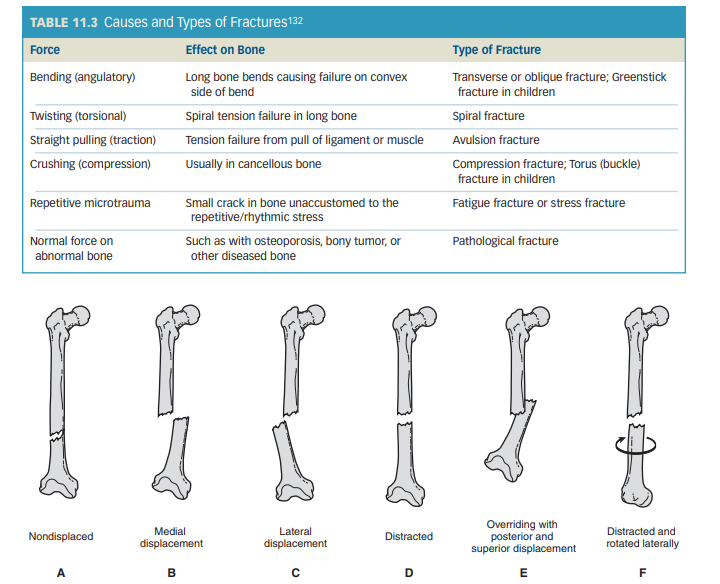
A Twisting (torsional) causes what type of fracture
Spiral
Pathological fracture are caused by whatt forces
Normal force on abnormal bone
A Crushing (compression) force causes what fracture
Compression fracture; Torus (buckle) fracture in children
A Transverse or oblique fracture; Greenstick fracture in children is caused by what type of force
Bending (angulatory)
An avulsion fracture is caused by what type of force
Straight pulling (traction)
A fatigue fracture or stress fracture is caused by?
Repetitive microtrauma
How to name a fracture:
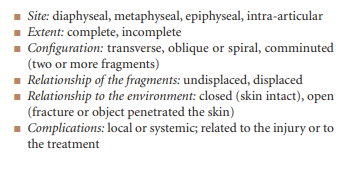
3 stages of bone healing:
Phase where there is hematoma formation and cellular proliferation
phase in which there is callous formation uniting the breach and ossification
phase in which there is consolidation and __________ of the bone
Inflammatory Phase
Reparative phase
Remodeling Phase
When the fracture site is firm enough that it no longer moves, it is _______ united
Clinically
True or False:
During the stage of clinical union on radiographic examination, the fracture line is no longer apparent
False:
the fracture line is still apparent, but there is evidence of bone in the callus
The bone is considered _________ healed, or consolidated, when the temporary callus has been replaced by mature lamellar bone
radiographically healed
children heal within?
adolescents within?
and adults within?
children heal within 4 to 6 weeks
adolescents within 6 to 8 weeks,
and adults within 10 to 18 weeks.
Which type of bone is more susceptible to compression forces, resulting in crush or compression fractures?
Cancellous bone
Complications of Fractures:
Swelling contained within a compartment
Fat embolism
Skin ulceration, nerve injury, or vascular compromise
Problems with fixation devices
Infection
Refracture
Delayed union
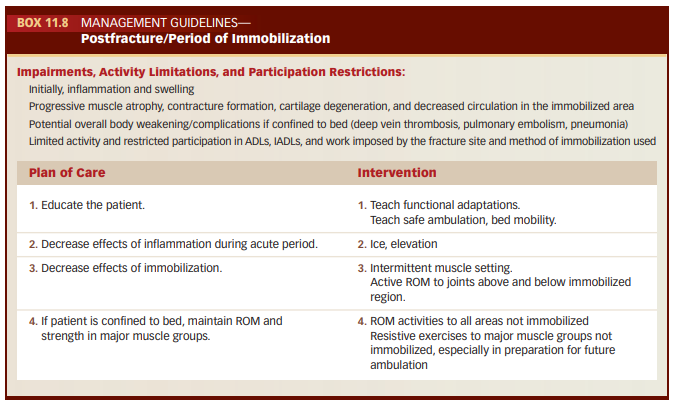
Management Guidelines for Postfracture / Period of immobilization
When applying joint mob exercises post immobilization, which grades are used initially?
grades 1 and 2
What type of stretching is used for postfracture postimmobilization patients
PNF stretching
For how many weeks following immobilization are light isometrics used for treating the weak muscles?
2 to 3 weeks
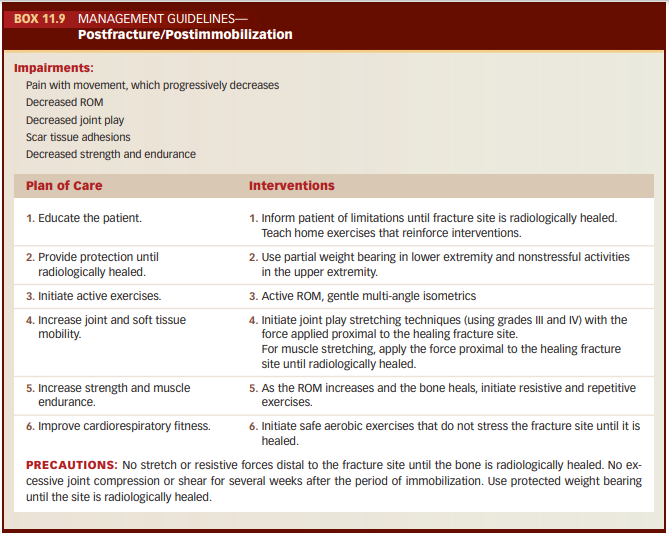
Management Guidelines for Postfracture / Postimmobilization