pain modulation and the thalamus 3/6
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
49 Terms
pain (nociception)
sharp pain (cutting)
dull pain (diffuse, burning)
sharp pain (cutting)
noxious stimuli that may be tissue damaging sources of energy (internal or external)
dull pain (diffuse, burning)
noxious stimuli following tissue damage (inflammation)
nociceptors are found in
skin, muscle, joint, connective tissue , viscera
types of nociceptors
myelinated A-delta fibers (fast pain)
unmyelinated C fibers (slow, burning pain)
pain is a
complex sensory and emotional experience
two phase of pain perception
discriminative: fast pain, well localized, sharp and pricking sensation
affective: slow pain, diffuse, dull burning pain
spinal fast pain pathway
neospinothalamic system
discrimination and localization
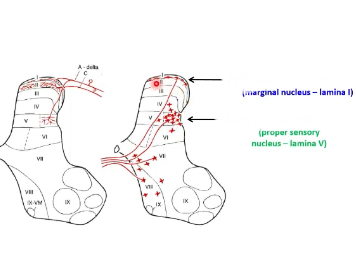
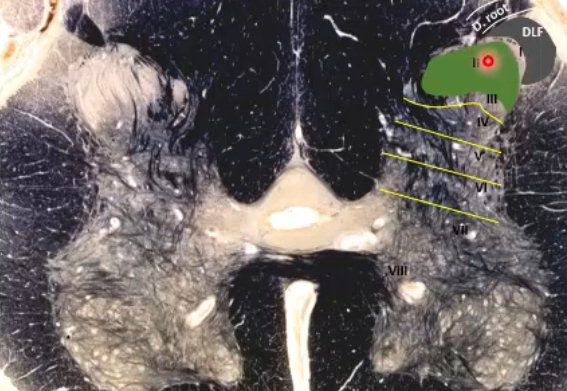
first order neuron synapses on lamina I marginal nucleus
axon decussates through ventral white commissure, ascends in spinothalamic tract
axons synapse on VPL in lateral thalamus
axons travel to primary somatosensory cortex for localization, discrimination, intensity perception
spinal slow pain pathways
paleospinothalamic and spinoreticulothalamic systems
phylogenetically older
affective/motivational/emotional/arousal aspects of pain
collaterals to medullary reticular formation—from massive reticulothalamic system which projects nociceptive impulses to medial thalamus then to many areas of cerebral cortex
where do the neospinothalamic, spinoreticulothalamic and paleospinothalamic tracts ascend?
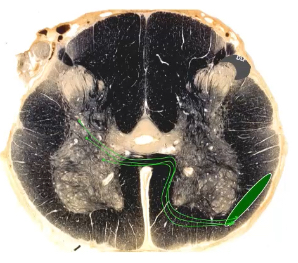
anterolateral quadrant/system/region
paleospinothalamic and spinoreticulothalamic tracts
cell bodies in spinal cord
axons travel toward thalamus, but first synapse and give off collaterals in spinal cord and brainstem (causes diffuse effect of slow pain)
go to different thalamic nuclei and then different cortical regions (causes responses in various systems to pain, ex. emotional)
slow pain pathway steps
c fibers synapse in lamina II/V
crosses ventral white commissure
ascends in anterolateral system/quadrant
collaterals enter reticular formation as info ascends brainstem to medial thalamus
medial thalamus projects to part of cortex associated w emotion (cingulate gyrus) and others
fast pain second order neuron
marginal nucleus lamina 1
slow pain second order neuron
spinal projection neurons→proper sensory nucleus (lamina 5)→axons cross at ventral white commissure→ascend in the anterolateral system (intermingled with spinothalamic tract)
slow pain vs fast pain
response to tissue damage vs acute pain
slow pain pathway first order neurons
unipolar neurons (C fiber) in dorsal root ganglion→project centrally through lateral portion/division of dorsal root/rootlets→funneled into Lissauer’s tract (dorsolateral fasciculus, DLF)→synapse in lamina 2 (substantia gelatinosa)
slow pain pathway third order neuron
medial thalamus:
intralaminar thalamic nuclei (centromedian)
medial dorsal nuclei
anterior nuclei
project to anterior cingulate cortex (ACC) and orbitofrontal cortex and insula

insula
integrates sensory, affective, and cognitive components for autonomic responses to pain, pain related learning and memory
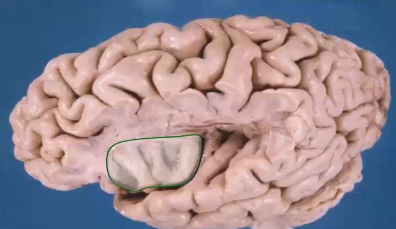
anterior cingulate cortex (ACC) and orbitofrontal cortex
transmits and processes pain related information and emotional responses, connects with and contributes to activity of centers responsible for modulating (descending) nociception (such as periaqueductal gray or PAG)

asymbolia for pain
patients with lesions of the insular cortex can recognize fast pain, but have no emotional responses
how does the PAG modulate descending pain pathways
ACC and orbitofrontal cortex have connections to PAG→descend and inhibit activity of pain pathways
medial dorsal nucleus
thalamocortical axons project to the limbic system for affective responses to pain (anguish, depression, fear, anger)
intralaminar thalamic nuclei
centromedian
thalamocortical axons project to widespread areas of cerebral cortex for arousal and attention
slow pain pathways share similarities with
spinothalamic pathway in the spinal cord—1st neuron cell bodies in DRG, 2nd neuron axons cross in ventral white commissure & ascend in anterolateral quadrant
slow pain pathways form
a multisynaptic reticulothalamic pathway
slow pain pathways give off terminals to
medulla (nucleus raphe magnus)
pons (locus coeruleus)
midbrain (periaqueductal gray)
hypothalamus (periventricular gray)
amygdala
reticular formation
influences voluntary movements
regulates visceral activity via the ANS
participates in the conduction and modulation of slow pain
associated with diffuse modulating systems
regulates activity of the cerebral cortex and consciousness

exogenous pain modulation
via large cutaneous primary afferent nerve fiber (A-alpha and A-beta) connections in the substantia gelatinosa (lamina II)
endogenous pain modulation
via activity of periaqueducteal gray, periventricular gray, nucleus raphe magnus, and dorsal horn neurons in substantia gelatinosa (also involved in other pain modulation, same mechanism from different area)
endogenous pain modulation pathway
analgesia centers (periventricular and periaqueductal gray) send descending fibers, impact nucleus raphe magnus, send descending pathway to dorsal horn→excites inhibitory interneurons in substantia gelatinosa (lamina II)→inhibit 2nd order pain neurons
exogenous pain modulation pathway
A-alpha and A-beta fibers give off collaterals (remainder ascends in spinal touch pathway), which excite substantia gelatinosa (lamina II) inhibitory interneurons, which inhibit 2nd order pain neurons that project to spinothalamic tract (spinal pain sensory pathway)
gate theory of melzack and wall
selective activation of large (A-beta) fibers to manage chronic pain
transcutaneous electrical nerve stimulation (TENS)
intractable pain treatments
aka pain that doesn’t go away
pharmacological approaches—NSAIDs, opioids
electrical stimulation
ablative surgeries—cut the nerve
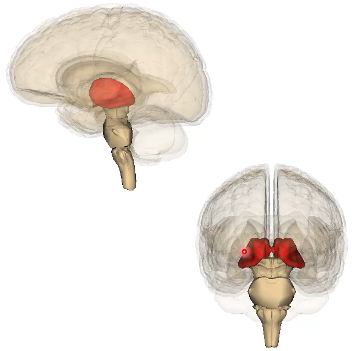
thalamus
gateway to the cerebral cortex
relay for motor information—basal ganglia (VA) and cerebellum(VL)
relay for sensory information—almost all sensory, cerebellar, BG, limbic pathways have neuronal relays in these nuclei; spinal pathways (VPL) and cranial pathways (VPM)
processes and refines information sent to cerebral cortex
receive, process, sort, send info back and forth between lobes of brain (arousal)
diencephalon parts
epithalamus (pineal gland)
subthalamus
hypothalamus
thalamus
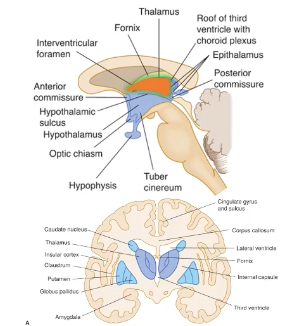
thalamic borders
medially: 3rd ventricle
laterally: internal capsule
superiorly: lateral ventricle
3 regions of each thalamus
medial, anterior, lateral
divided by internal medullary lamina
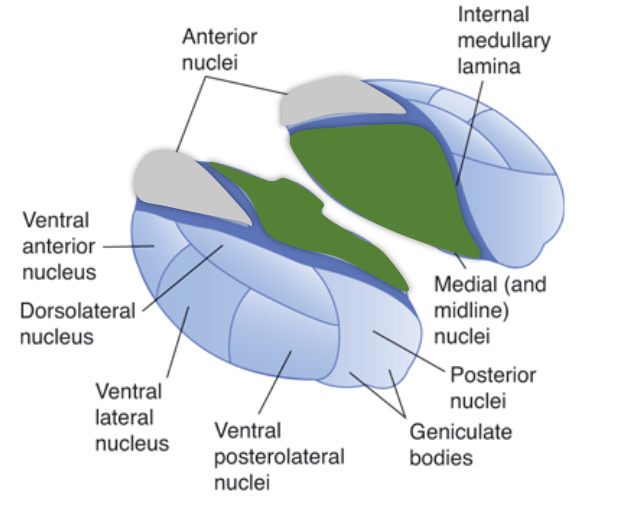
fast pain thalamic nucleus
ventral posterior nucleus in lateral thalamus (spinal→VPL, cranial→VPM)
slow pain thalamic nucleus
medial thalamus—intralaminar, medial dorsal, anterior nuclei
cerebellum thalamic nucleus
ventral lateral (VL)
basal ganglia thalamic nucleus
ventral anterior (VA)
auditory pathway thalamic nucleus
medial genicualte nucleus (MGN)
visual pathway thalamic nucleus
lateral genicualte nucleus (LGN)
PI: which statement correctly summarizes exogenous inhibition of pain?
flow of ascending pain info is modified by stimulation of low-threshold mechanoreceptors
flow of ascending pain info is modified by stimuli from cortical centers
flow of ascending pain info is modified by stimuli from brainstem centered
descending inputs from pain centers indirectly modify the activity of dorsal horn projection neurons by acting on local circuit neurons
descending inputs from pain centers directly modify the activity of dorsal horn projection neurons
1
PI: which thalamic nucleus contributes to the affective aspect of pain?
ventral posterolateral
ventral posteromedial
ventral anterior
ventral lateral
medial dorsal
5
note to self
make separate flash cards for thalamic nuclei and where they project to—medial dorsal projects to ACC & orbitofrontal cortex

PI: in an experiment, subjects are given a selective A-delta fiber blocker and then exposed to a strong heat stimulus. which curve best represents the expected perception of pain by the subjects?
A
B
C
D
E
1
PI: in a neuroscience experiment examining the effect of hypnosis on pain perception subjects were first poked in the hand with a sharp probe and asked to rate the pain on a 1 (no pain) to 5 (intense pain) scale. researchers noted how much pressure it took to elicit pain at both a level 2 and a level 4. subjects were then hypnotized and scanned using fMRI. during fMRI evaluation, subjects were poked with the sharp probe with enough pressure to elicit level 2 pain. without changing the intensity of the pressure, researchers then persuaded subjects that the pressure was increasing during the fMRI measurements. in what brain region would you expect to see increases in activity in the hypotized subjects?
cerebellum
somatosensory cortex
ventral posterolateral nucleus of the thalamus
anterior cingulate gyrus
no region would change in activity
4
PI: logan has been managing chronic pain in his leg and back from bike accident injuries for over a year. his doctor has suggested that they stimulate his brain in an attempt to relieve some of the pain. stimulation of which region would be most likely to produce relief?
periaqueductal gray
somatosensory cortex
medial geniculate nucleus
ventral posterior medial nucleus of the thalamus
superior colliculus
1