CAR week 3 - ECG and blood pressure
1/125
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
126 Terms
What is an ECG?
It’s an electrocardiogram
it represents the electrical activity of the heart in a graph
it monitors rate and rhythm
electrical activity is recorded using electrodes attached to the skin surface
What does an ECG assess?
heart rate
heart rhythm
What is the baseline of an ECG called and what is it used for?
it is called the isoelectric line
used to show no voltage change
what is the shape of an ECG dependent on?
direction of contraction and lead position
when does a positive deflection in an ECG occur
when the wave of depolarisation travels towards the lead
when does a negative deflection occur in an ECG?
when the wave of depolarisation travels away from the lead
What do we measure an ECG on?
graph paper
what is paper output speed
the rate at which the ECG machine produces a trace
what 2 paper output speeds are used for ECGs?
25mm.sec and 50mm/sec
what setup do we need for a 50mm/sec ECG?
lead II
right lateral recumbency
what does the vertical axis of an ECG show?
amplitude of the heart’s electrical current in milivolts (mV)
10mm in height = 1mV
each 1 mm square = 0.1 mV and large square is 0.5mV
what does the horizontal axis on the ECG show?
time
at 25mm/sec, 1mm square = 0.04sec, each large square = 0.2sec
at 50mm/sec, 1mm square = 0.02 sec and each large square = 0.1sec
when and why would we use a 50mm/sec paper output rate
when we have a tachycardic patient
it’s easier to spot abnormalities that may by lost due to a fast heart rate
How do we calibrate ECG paper?
use ECG chamber
it’s important to make sure the ECG paper is standardised to 1mV vertically and 5mm horizontally
What causes the electrical activity in the heart?
the myocardial muscle cells contain many ions and many ion channels which initiate depolarisation in their movement
the abundance of ions means they can act as electrical conductors.
What leads to depolarisation of the myocardial cells?
normally it’s interior is negative and exterior is positive, causing a potential difference across the cell membrane, forcing ions to move
+ve ions cross the cell membrane into myocardial cell. When threshold is reached, AP is triggered and the cell depolarises
depolarisation = contraction
this spreads across the myocardium like a domino effect
what ions are involved in electrical conduction
Na+
K+
Ca2+
What is the general idea of how antiarrhythmic drugs work? What are they used to treat?
they work by altering Na+, Ca2+ and potassium channels, adjusting how excitable a cell is
they may also block the sympathetic activity to the heart e.g. beta blockers
used to treat cardiac arrhythmias
Outline the conduction pathway through the heart
Initial impulse generated by SAN
impulse travels through AVN and bundle of His
then down L/R branch block into the purkinje fibres
In a healthy heart, where does normal conduction start?
SAN
In an abnormal heart/heart with a problem, what can assume the role of pacemaker if the SAN is damaged and what is this known as?
AVN
escape rhythm
Outline pacemaker cells:
where we find them
what they can do
what enables them to do this
SAN
self generate electricity and spontaneously depolarise
unique ion channels provide this action potential
Outline non-pacemaker cells:
where do we find them
what do they do
what protects them from random excitation
atrial and ventricular cardiomyocytes, purkinje conduction system
conduct electrical impulses generated by the pacemaker cells
have a plateau phase where they can’t be triggered
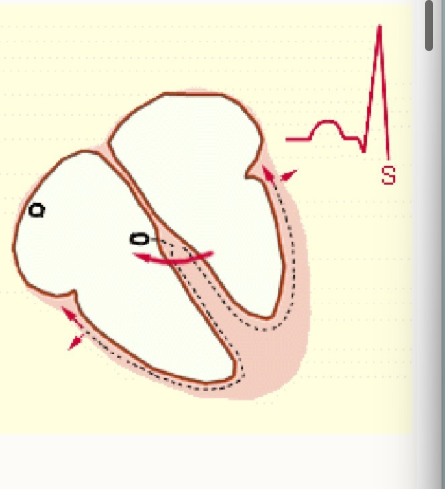
what do that parts of an ECG represent?
movement of these electrical signals through specific areas
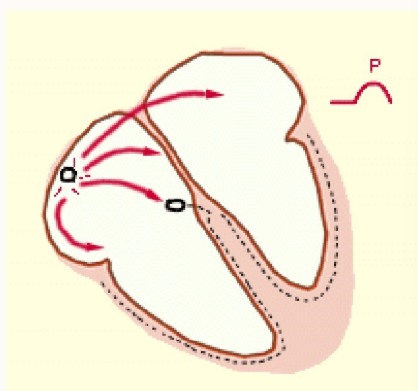
What is the P-wave of the ECG
electrical impulse generated in the SA node
impulse is rapidly spread across the atrial muscle, causing depolarisation and contraction = atrial systole
impulse arrives at AV node
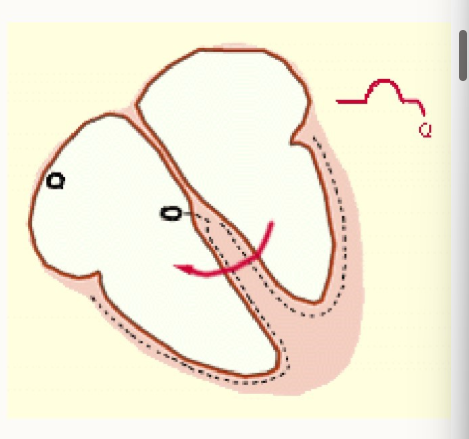
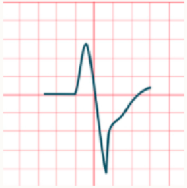
what is the Q wave
when the impulse travels through AV node into bundle of His → L/R bundle branch into purkinje fibres
interventricular septum depolarises ready to spread impulse across the ventricles
ventricles fill with blood (ventricular diastole)
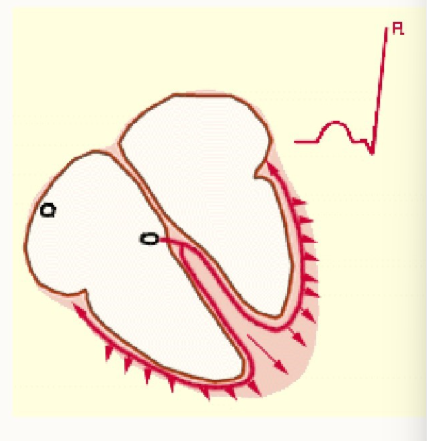
what is the R wave?
electrical impulse spreads across ventricular muscle
ventricles depolarise and contract (ventricular systole)
blood is ejected from the ventricles
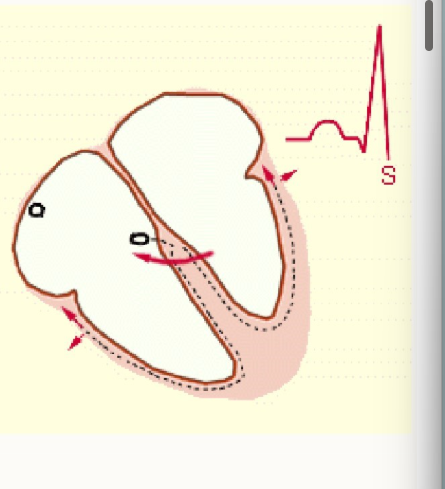
what is the S wave
electrical impulse reaches the last remaining areas of the ventricles = late ventricular depolarisation
ventricles then relax
what is the T wave
ventricular muscle repolarises, resetting electrical charge after contraction in preparation for the next heartbeat
what is normal sinus rhythm
the normal rhythm of the heart
How do we identify normal sinus rhythm
ECG shows that the SA node is initiating electrical impulses
electrical activity is following the normal path of conduction through the heart - this is the rhythm or pattern of the heartbeat
ECG shows regular rate
How do we determine if the rhythm is regular or irregular
measure distance b/w QRS complex = RR interval
is it constant = regular rhythm
does it differ b/w beats = irregular rhythm
what does a narrow QRS complex indicate?
supraventricular in origin

What does a wide QRS complex indicate?
likely to have originated in the ventricles
if electrical activity is initiated w/in ventricles and travels by an abnormal path across the ventricular muscle, depolarisation occurs at a slower rate
What are the 3 kinds of ectopic complexes
PACs: pre-atrial complex
AV junctional (atrioventricular)
VPCs - ventricular premature complex
what is the waveform and interval change of PACs?
premature P wave
P wave shape changes (signal isn’t from SAN)
PR interval normal or prolonged
QRS measurement = narrow (signal still originates from atrium)
Pause following complex - SAN resets
what is the waveform and interval changes of an AV junctional?
no preceding P wave or inappropriately placed P wave
QRS complex sooner than expected
pause following complex
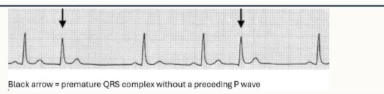
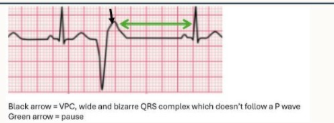
What is the waveform and interval changes of VPCs
No P wave before VPC - signalment doesn’t come from SAN
broad QRS complex
QRS is abnormally shaped - wide and bizarre b/c electrical activity is originating from ventricles
pause following complex
What are the steps of checking an ECG? What are 2 additional checks we should make?
what is the heart rate
is there a P wave for every QRS?
is there a QRS complex for every P wave
what is the relationship b/w P waves and QRS complexes?
are QRS complexes narrow or wide?
Are there T waves and are their shape normal?
Is the rhythm regular or irregular
Do all complexes look the same?
Additionally:
amplitude of each wave
segment interval times
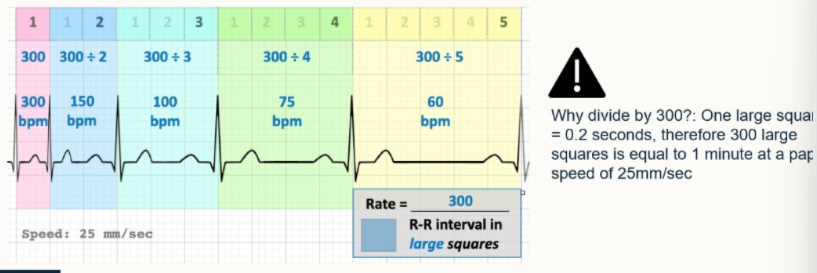
When do we use:
Large square method
Small square method
R wave method
For calculating heart rate?
for ECGs that show a regular rhythm and rate
useful for very fast regular rhythms, as likely to provide more accurate rate than large square method
useful for slow/irregular rhythms, use if RR intervals are irregular
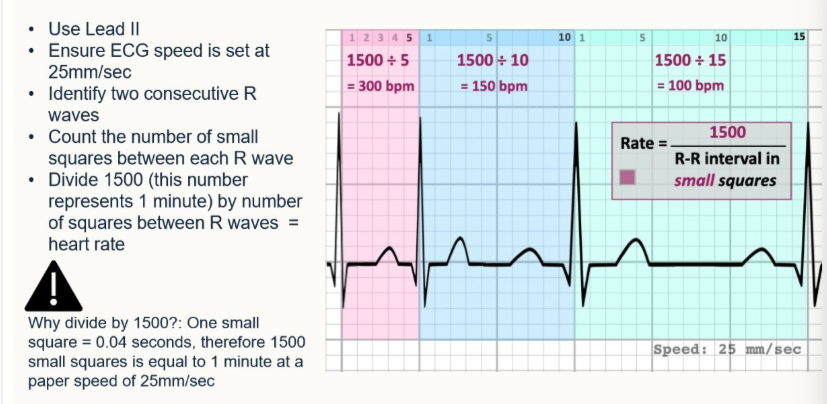
How do we calculate HR with small square method for
a) 25mm/sec
b) 50mm/sec paper output
Firstly, count the number of small squares b/w R waves
a) 1500 / number of small squares
b) 3000 / number of small squares
How do we calculate HR using RR interval for:
a) 25mm/sec paper output
b) 50mm/sec paper output
Firstly: count the number of R waves in 30 large boxes
a) multiply that number by 10 (30 boxes = 6 seconds, 60/6=10)
b) multiply the number by 20 (30 boxes = 3 seconds, 60/3=20)
How do we do a large square method for 25mm/sec:
what setup is needed
what speed
how do we calculate?
Lead II
ensure ECG is set at 25mm/sec
identify 2 consecutive R waves, count the number of large squares b/w each, divide this by 300.
How do we do a small square method for 25mm/sec:
what’s setup is needed
what speed
how do we calculate it
Lead II
25mm/sec
identify 2 consecutive R waves, count no. small squares between them, divide by 1500
what lead setup is needed for the R wave
lead II
what lead setup do we need for a 50mm/sec
Lead II (same as for 25mm/sec)
What is RR? what does it represent and what is it used for?
distance b/w two R waves on an ECG
represents the interval b/w heartbeats and regularity of rhythm
used to calculate heart rate
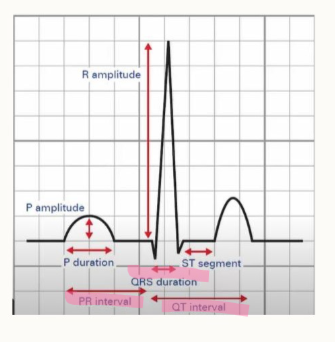
what is PR and what does it reflect?
measure from beginning of the P wave to the beginning of QRS wave
reflects conduction through the AV node
What is an ST wave, what does it represent?
measurement b/w end of the S wave and the beginning of the T wave
represents the interval b/w ventricular depolarisation and repolarisation
what is important to understand about canine and feline interval times?
they differ
depending on species
breed
age
any heart conditions
give the normal values for a dog for:
P wave
QRS complexes
T wave
in seconds and mV?
0.02-0.04 = 0-0.4mV
0.03-0.05 = <_ 3 mV.
0.04-0.08 = 0.5 mV
give the normal values for a cat for:
P wave
QRS complexes
T wave
in seconds and mV?
<0.04s = 0-0.2mV
0.03-0.04s = -0.1→0.8mV
0-0.04s = 0-0.3mV
what are the normal interval times for:
RR
PR
ST
in a dog?
0.35-0.8s
0.08-0.12s
0.04-0.1s
what are the normal interval times for:
RR
PR
ST
in cats?
0.06-0.13s
0.05-0.07s
0.06-0.08s
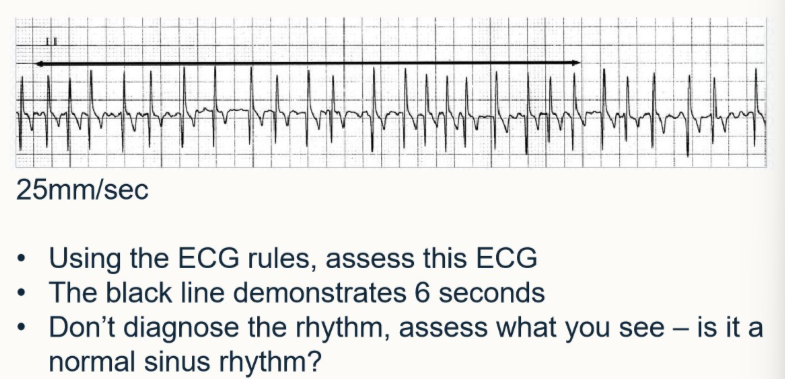
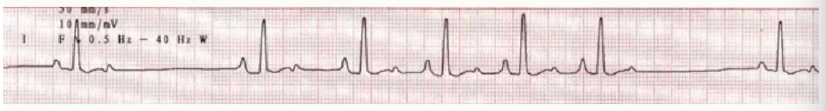
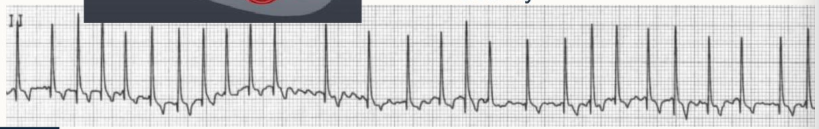
Using ECG rules, assess this ECG
the black line = 6s
assess what you can see
is it normal sinus rhythm
HR = 200bpm = tachyarrhythmia
no P wave
QRS complexes are narrow and upright
RR interval irregular
not normal sinus rhythm
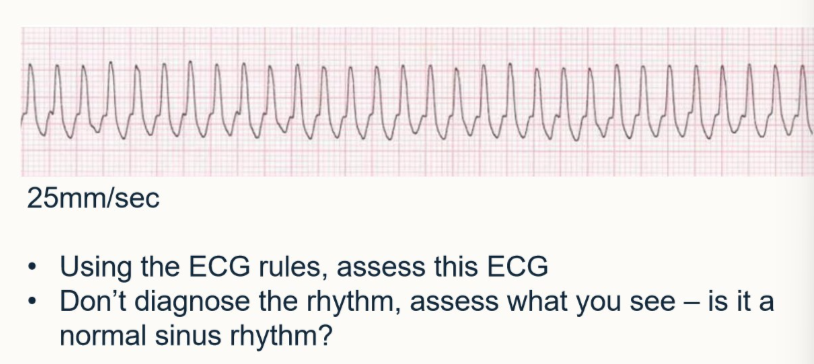
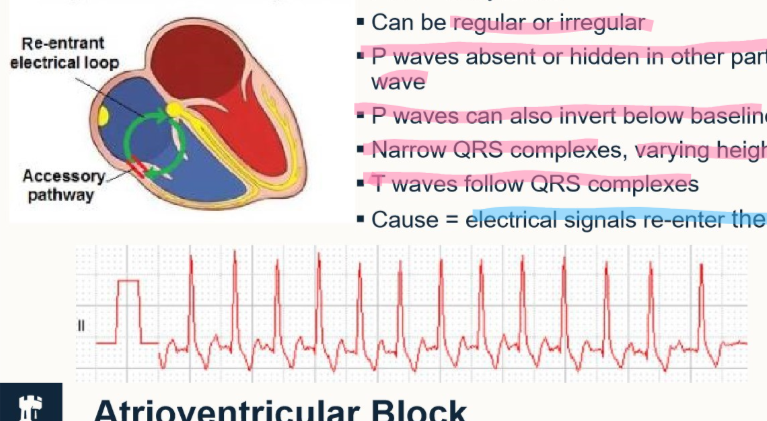
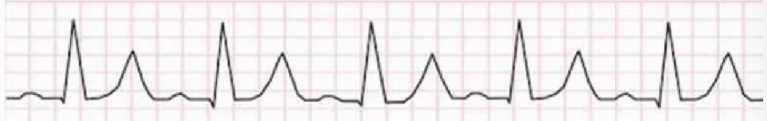
Using ECG rules, assess this ECG
assess what you can see
is it normal sinus rhythm
HR = 300bpm = tachyarrhythmia
no P waves
QRS complexes wide
RR interval regular
not normal sinus rhythm
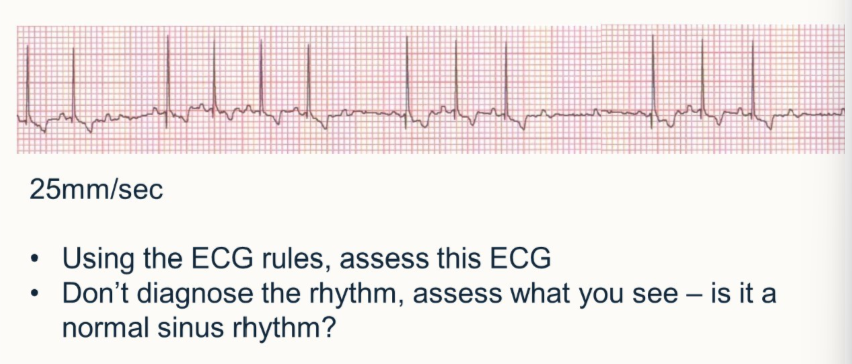
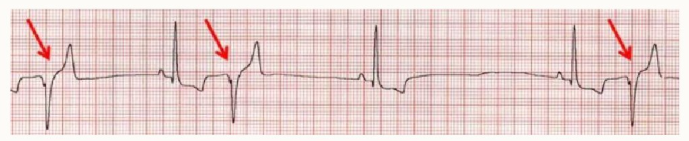
Using ECG rules, assess this ECG
assess what you can see
is it normal sinus rhythm
HR = 120bpm = normal
several P waves occur without a following QRS complex
QRS complexes are narrow and upright
RR interval irregular
not a normal sinus rhythm
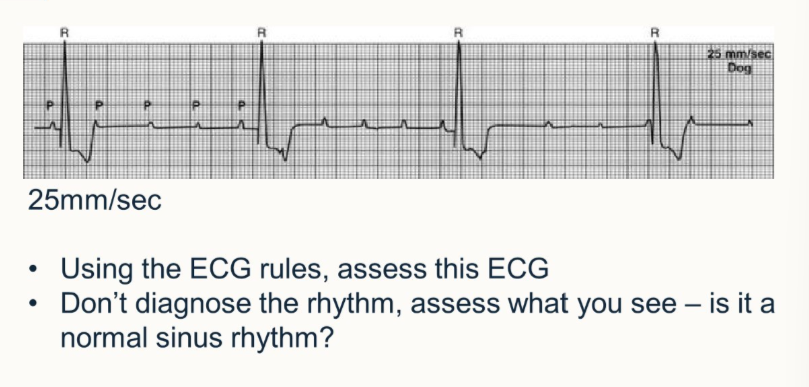
Using ECG rules, assess this ECG
assess what you can see
is it normal sinus rhythm
HR = 30bpm = bradyarrhythmia
P waves are present, no association with QRS complexes - no P wave for every QRS and no QRS for every P wave
QRS complexes are normal width/height
RR interval is regular
not a normal sinus rhythm
What questions do we need to ask ourselves when assessing arrhythmias? (3)
do we have brady or tachyarrhythmia?
is the rhythm, sinus, supraventricular or ventricular
where did the heartbeat originate from ^ (SAN, AVN/atria, ventricles?)
what is meant by an ectopic complex?
premature or extra beats caused by unusual impulses
Outline sinus arrhythmia:
what is its rhythm
what causes it to increase/decresae
how would we describe the rate
what is common in dogs with this?
normal sinus rhythm
rate increases on respiration and decreases during pause b/w breaths
change in rate = variation in RR intervals = regularly irregular
common dogs - high resting vagal tone
Outline sinus tachycardia:
where does it originate from
what waves are present and what does this make the rhythm
how would we describe it on an ECG
what can cause it
sinus = normal beat originating from the SAN
P wave, QRS complex and T wave present = normal sinus rhythm
fast but regular rhythm
causes = increased sympathetic tone, medication, systemic
Outline sinus bradycardia:
where does it originate from
what waves are present and what does this mean
how would we describe it on an ECG
what can cause it?
SAN = sinus
P wave, QRS complex, T wave = normal sinus rhythm
slow but regular rhythm
medications, electrolyte disturbances, vagal stimulation, hypothermia, hypoadrenocorticism, hypothyroidism, raised ICP
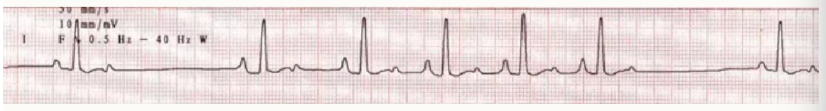
Outline supraventricular tachycardia:
what does this mean
what can the rhythm be?
what waves are present/absent
what causes it?
tachycardia - fast
can be regular or irregular
P waves absent/hidden in another part of the wave
P waves can be inverted below the baseline
narrow QRS complexes, varying heights
T waves follow QRS complexes
Cause = electrical signals re-enter atria (go along an abnormal pathway which constantly stimulates atrial systole)
the green circle represents this
Outline atrioventricular block:
what is it
what kinds are there and how do we diagnose
what does an ECG change imply?
what waves are present and not present?
delay or disturbance in the transmission of electrical impulses from the atria to the ventricles
numerous types - assess the relationship b/w P waves and QRS complexes to diagnose
AVN issues - P waves present but not associated with QRS complexes, prolonged PR interval

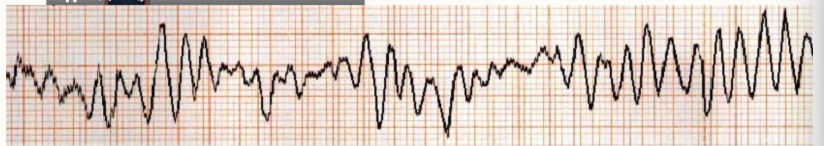
Outline ventricular fibrillation:
what does it look like on an ECG:
what waves are present/absent
what is causing it
irregular deformed wave
no distinct P wave, QRS complex or T wave anywhere
ventricular myocardium depolarising erratically (not one smooth motion)
re-entry, triggered activity, automaticity
Outline ventricular tachycardia (VT):
what does it look like on an ECG
what is the heart rate (normally)
what does a rapid rate result in?
what can cause it?
wide and bizarre QRS complexes, no associated P waves
tachycardia = >120/180bpm (dog/cat)
low cardiac output = reduced preload and stroke volume
re-entry, triggered activity, automaticity

Outline atrial fibrillation:
what does it look like on an ECG
what other symptoms may be present
what causes it?
narrow, upright QRS complexes
irregular ventricular rate
absence of P wave
irregular RR interval
undulating baseline
tachycardic, pulse deficits
re-entry, triggered activity
Outline hyperkalaemia:
what does it look like on an ECG
what causes it?
peaked/spiked T waves
flat/absent P waves
prolonged QT interval
widened QRS complex
cause = high potassium disrupts electrical signals
Outline ventricular premature complexes (VPCs):
where do the signals originate from?
what does it look like on an ECG
what does the signal interrupt?
what is it an example of?
ventricles - no P wave
QRS are wide and bizarre
signal interrupts sinus (normal rhythm)
ectopic beat - premature impulse that starts in ventricles
these may look different in each ECG, the wave may e inverted in some and not in others - this is dependent on where the signal originates in the ventricles
what are the 3 pieces of equipment we can use to measure blood pressure and are they direct or indirect?
arterial catheter and pressure transducer = direct
doppler ultrasonography = indirect
oscillometric = indirect
what do each of these methods read pressure wide:
arterial catheter and pressure transducer
doppler ultrasonography
oscillometric
systolic, diastolic, mean
systolic
mean, then systolic and diastolic is calculated through algorithms
what are 2 advantages to arterial catheter and pressure transducer
‘real time’ monitoring to detect trends and allow for immediate intervention if necessary
restraint only needed for initial placement, so falsely elevated readings due to stress from handling are less likely
what are 4 disadvantages to arterial catheter and pressure transducer
equipment is expensive
invasive procedure which is difficult
risk of complications such as bleeding from site
need close and continuous monitoring
what are 5 advantages of doppler ultrasonography
easy to use
affordable
readily available in most clinical settings so can be utilised in conscious patients and when monitoring anaesthesia
usually well tolerated
appropriate for patients with hypertensions and cardiac arrhythmias
what are 4 disadvantages to doppler ultrasonography
absolute values may not be identical, therefore as accurate, as direct monitoring
correct cuff size is imperative
patient may need restraining which could cause an increase in BP (if incorrect). Position of patient can affect reading
difficult to obtain readings in patients with severe peripheral vasoconstriction and if patient is stressed
what are 3 advantages to oscillometric BP reading
automated process, therefore less technical skill is required
monitors can be programmed to measure at timed intervals
little/no restrain of patient
what are 3 disadvantages to oscillometric BP reading?
not accurate in patients <5kg
patient must be still, so good for anaesthesia monitoring but not always in conscious patients
less accurate if patient has cardiovascular arrhythmias, significant tachycardia or bradycardia, vasoconstriction or hypothermia
When do we measure BP?
during anaesthesia
in patients with heart disease
in diabetic patients
in patients with renal disease
in patients with thyroid disease (hyper (cats) hypo (dogs))
in obese patients
in geriatric patients
in patients undergoing medical treatment where blood pressure allows us to monitor stability → blood transfusion
What equipment do we need for doppler BP reading?
headphones
ultrasound gel
probe
doppler
surgical spirit ± clippers
cuff
sphygmomanometer
pump to inflate the cuff
How does a doppler work?
ultrasound gel is placed over crystal surface and placed distal to the cuff
doppler uses the crystal to detect pulsatile flow and converts it to an audible sound
cuff is inflated to a P greater than that of BP to occlude the artery, so audible sound of pulsatile flow is lost
as P is released, audible sound of flow returns and the number on the sphygmomanometer in which it does, is the systolic pressure
repeat 2-3 times to obtain several readings (fully deflating the cuff b/w each reading) and take the average value
How do we choose the correct cuff size? What happens if cuff is too large/too small?
width of cuff needs to be 30-40% of total circumference of the limb (or tail) where we place the cuff
too large = reading will be falsely low
too small = reading will be falsely elevated
What is Einthoven’s triangle?
place 3 electrodes on the body to make an equilateral triangle
shows how leads I, II and III surround the heart like a circuit.
Useful for identifying correct/incorrect lead placement which may lead to incorrect diagnosis.
why do we get 6 electrical views of the heart from 4 electrodes?
each electrode records electrical activity of the heart in relation to itself and in combination with other leads
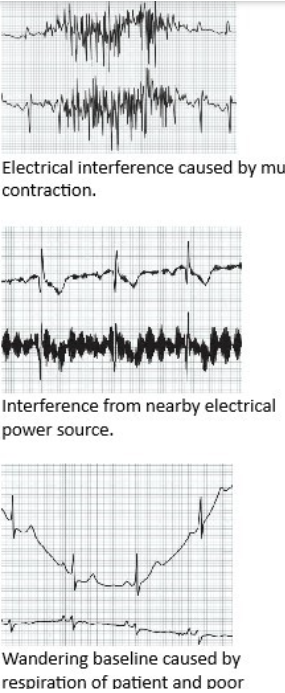
What are 9 steps we can take to reduce artifacts on an ECG
switch off non-essential electrical devices and equipment nearby
is the patient close to the machine power source? Try using battery power if possible
ensure cables aren’t tangled or in contact with metal objects/tables
all leads should NOT run across the machine
inspect wires and cables for cracks/damage
is filter on/off? - filter can help reduce interference from muscle, turn off for lead II (can lead to distortion of the waves)
ensure all connectors are attached to the machine
ensure all electrodes are attached properly
Bottom image - caused by poor respiration of patient and poor electrode connection
what are 6 things to consider about the patient when preparing for an ECG?
reduce movement as much as possible
don’t cross the limbs
patient should be calm, not panting/purring/trembling
fur/skinn should be free from excessive oil/water - clean with surgical spirit and dry
fur can be clipped to improve contact
right lateral recumbency
what are 3 points to consider about electrode application?
use adequate surgical spirit or ultrasound gel to improve contact/signal
maximise surface area of attachment
consider if the electrodes are placed over a joint or significant muscle mass - interference from movement/contraction more likely, aim for fleshy areas around olecranon and stifle

Give the standard time for dogs for:
P wave
PQ interval
QRS
QT interval
<0.04s
0.06-0.13s
<0.05 or <0.06 (giant)s
0.15-0.25s
Give the standard time for cats for:
P wave
PQ interval
QRS
QT interval
<0.04s
0.05-0.09s
<0.04s
0.12-0.18s
Give the standard amplitude (upper limit) for these waves in a dog:
P
R
T
<0.4mV
<3.0mV
<1/4 R wave mV
Give the standard amplitude (upper limit) for these waves in a cat:
P
R
T
<0.2mV
<0.9mV
<1/4 R wavemV
what is the general function of the cardiovascular system?
deliver oxygenated blood to the tissues and to remove CO2
What should we always do when interpreting clinical findings/readings
consider all of them - never just one
what would we like to measure in the cardiovascular system vs what can we measure?
tissue oxygen delivery
tissue perfusion and blood oxygen content
what drives tissue perfusion
mean arterial pressure (MAP)
how do we measure MAP?
arterial blood pressure - invasively: canulated peripheral arterty
arterial blood pressure - non-invasive: sphygmomanometry, oscillometric and doppler
‘feeling with fingers’ - not ideal
what is the gold standard method of measure MAP?
cannulated artery
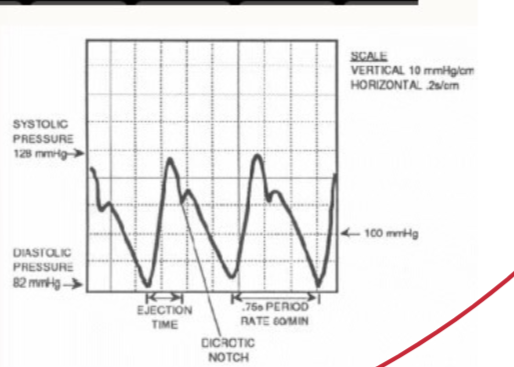
Outline the direct/invasive method of taking a blood pressure
real time - beat by beat
gives more information from trace
more accurate
insert a cannula into a peripheral artery
connect a cannula to transducer
reported as systolic/diastolic and (mean)
what pressure readings can a doppler obtain and what is it dependant on?
diastolic, systolic and mean
method of reading it
what does CVP measure and why is this relevant clinically?
it measures the volume of blood returning to the RHS of the heart
reflects the volume of blood returning to the heart - if P increases, indicates heart may be failing. if it falls - may have haemorrhage in the body