anatomy and physiology of liver
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
43 Terms
What are the key roles of the liver relevant to pharmacy?
The liver is central to drug metabolism and detoxification. Its main pharmacy-related roles include:
Metabolism of drugs and toxins
First-pass metabolism of orally administered drugs
Detoxification of harmful substances
CYP450 enzyme activity (major drug-metabolizing enzymes)
Bioavailability regulation through metabolic processes
Handling of prodrugs (activation into active forms)
Jaundice (bilirubin accumulation due to liver dysfunction)
Drug interactions through enzyme induction/inhibition
Hepatotoxicity (drug-induced liver damage)
Bile production for fat digestion and excretion of metabolites
Albumin synthesis for drug binding and transport
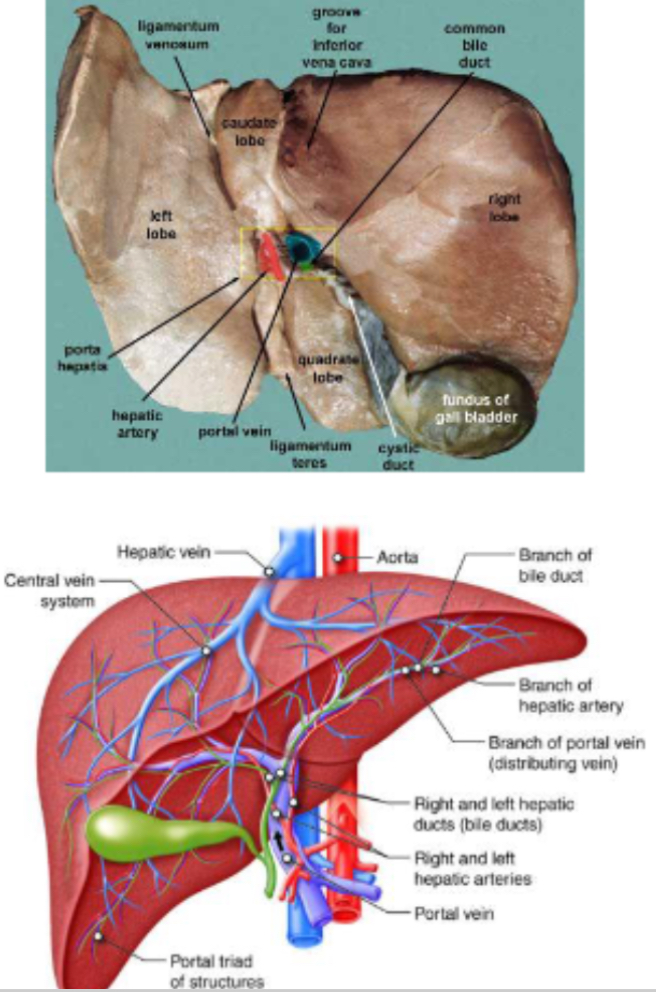
PHOTO: What does the liver overview diagram show?
It visually depicts the liver’s major functions and anatomical location under the diaphragm, showing how it contributes to:
Metabolism, detoxification, and drug processing
Bile secretion and bilirubin management
Blood flow from the portal vein and hepatic artery
Pharmaceutical relevance: emphasizes that most drugs are metabolized or detoxified in the liver before entering systemic circulation.
What are the main characteristics and roles of the liver? And pharmacy relevance
It’s the largest internal organ (~1.5 kg in adults).
Lies under the right ribs, protected by the diaphragm.
Has a dual blood supply:
Hepatic artery → oxygenated blood.
Portal vein → nutrient- and drug-rich blood from the GI tract. - comes from gut
Receives ~25% of cardiac output.
It is the first organ to process orally absorbed drugs via first-pass metabolism.
Pharmacy relevance: Orally administered drugs must first pass through the liver, where they undergo metabolism before reaching systemic circulation — a critical factor in determining bioavailability.
What are the main anatomical features of the liver? And pharmacy relevance
Divided into right and left lobes.
Composed of lobules, which are the hexagonal functional units of the liver.
Each lobule contains a portal triad (hepatic artery(oxygenated blood from heart), portal vein(bringing nutrient and drug from gut), bile duct(drains bile to gall bladder which drains into intestine with chyme, bicarbonate to neutralise the acidic chyme) and a central vein.
The central vein drains “cleaned” blood into the hepatic vein → then to the vena cava.
Pharmacy relevance:
Drug molecules and toxins are metabolized by hepatocytes as blood flows through lobules before entering systemic circulation — crucial for understanding drug clearance and first-pass metabolism.
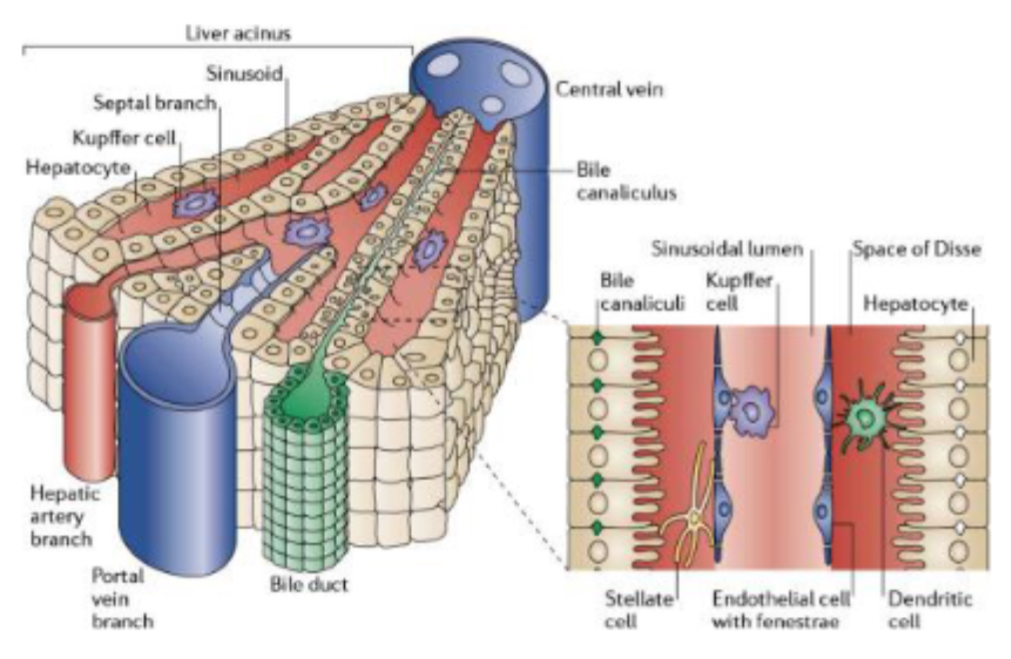
PHOTO: What does the liver gross anatomy photo show?
The image displays the right and left lobes, portal triads, and central veins arranged in hexagonal lobules.
It likely labels the hepatic artery, portal vein, and bile duct (the “portal triad”).
Demonstrates direction of blood flow toward the central vein and bile flow toward the periphery.
Key takeaway: The spatial organization explains how drugs and toxins are processed through hepatocytes before being excreted or entering circulation.
What are hepatocytes and what are their functions?
Hepatocytes are the main functional cells of the liver.
Functions include:
Metabolizing nutrients, drugs, and toxins.
Producing bile necessary for digestion and fat absorption.
What are sinusoids and what is their role in liver function?
Sinusoids are specialized, leaky capillaries in the liver.
They carry blood from both the portal vein (nutrient-rich) and hepatic artery (oxygen-rich) to hepatocytes.
They enable exchange of nutrients, oxygen, drugs, and toxins between blood and liver cells.
What are Kupffer cells and what is their role?
Kupffer cells are macrophages located within liver sinusoids.
They remove bacteria, debris, and damaged blood cells from the blood.
Function as an immune defense barrier against pathogens absorbed from the gut.
What are canaliculi and why are they important?
Canaliculi are tiny channels between hepatocytes.
They collect bile produced by hepatocytes and direct it toward the bile ducts.
What are bile ducts and what is their function?
Bile ducts transport bile from canaliculi to the gallbladder and intestine for digestion.
This ensures fat digestion and excretion of drug metabolites via bile.
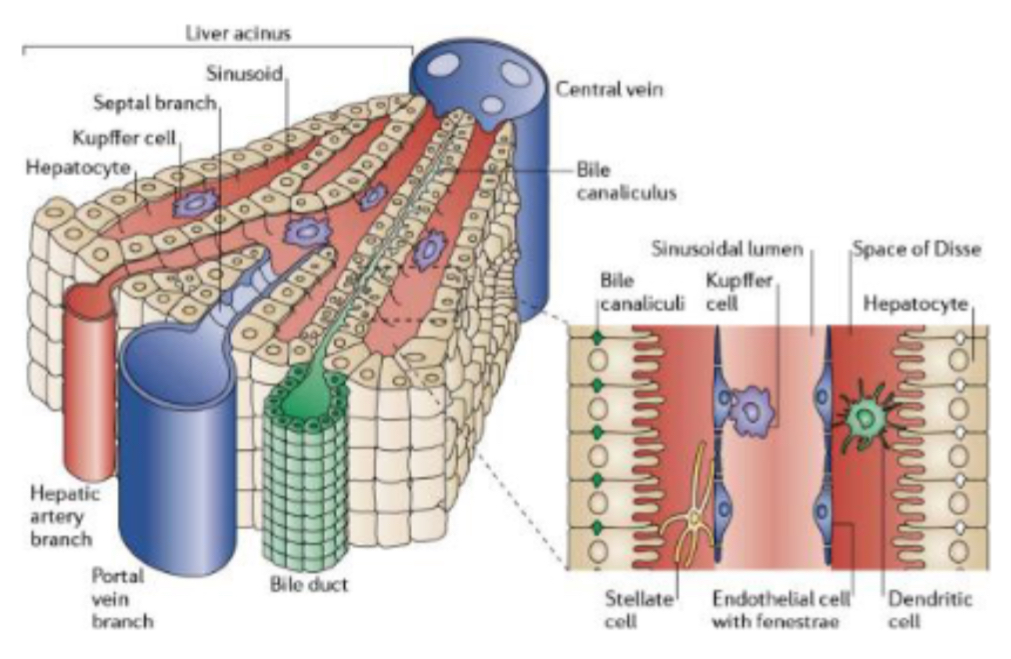
PHOTO: What does the liver microanatomy diagram show?
The image illustrates liver lobules under the microscope.
You can see hepatocytes, sinusoids, Kupffer cells, bile canaliculi, and portal triads.
Arrows usually show blood flow (from portal triad → central vein) and bile flow (from hepatocytes → bile duct).
Key takeaway: Demonstrates the interaction of blood and bile flow essential for drug metabolism and detoxification.
What are the three major types of metabolism carried out by the liver?
Carbohydrate metabolism
Lipid metabolism
Protein metabolism
Each pathway is essential for maintaining energy balance, hormone production, and detoxification.
What are the main functions of the liver in carbohydrate metabolism? And pharmacy relevance
Glycogen storage and release (when low) to maintain blood glucose homeostasis.
Gluconeogenesis (glucose production) during fasting.
Conversion of excess glucose to fatty acids in liver for long-term energy storage. (Excess sugar stored as fat —> fatty liver)
Pharmacy relevance:
Drugs affecting insulin, glucagon, or hepatic enzymes (e.g., metformin) can alter carbohydrate metabolism in the liver.
What are the main functions of the liver in lipid metabolism? And pharmacy relevance
Synthesis of cholesterol, triglycerides, and phospholipids.
Steroid hormones (lipids) made in liver
Production of lipoproteins (HDL, LDL, VLDL) for lipid transport.
Essential role in steroid hormone synthesis (e.g., cortisol, oestrogen, testosterone).
Pharmacy relevance:
Drugs like statins inhibit cholesterol synthesis in hepatocytes. Hepatic dysfunction can alter lipid levels and drug handling.
What are the main functions of the liver in protein metabolism? And pharmacy relevance
Synthesis of plasma proteins such as:
Albumin (drug binding and osmotic pressure maintenance)
Clotting factors (hemostasis)
Transport proteins (e.g., transferrin)
Urea cycle: detoxifies ammonia formed from amino acid breakdown into urea for renal excretion.
Pharmacy relevance:
Albumin (made in liver) binds acidic drugs (e.g., phenytoin, warfarin), affecting drug distribution and free concentration. . If issue with albumin, has issues with bioavailability of drug that’s why need to monitor albumin levels in elderly eg. If on warfarin to prevent toxicity
Enzyme activity in hepatocytes drives Phase I & II metabolism, influencing drug clearance.
First-pass metabolism impacts oral drug bioavailability.

PHOTO - What does the liver metabolism diagram show?
It visualizes how the liver integrates carbohydrate, lipid, and protein metabolism.
Arrows typically indicate:
Glucose ↔ glycogen (storage/release)
Amino acids → urea (detoxification)
Fatty acids → triglycerides/cholesterol
Often includes pathways to bile formation and drug metabolism.
Key takeaway: the liver is the central metabolic hub, balancing nutrient use, detoxification, and drug processing simultaneously.
What is first-pass metabolism?
First-pass metabolism is the process by which orally administered drugs are metabolized by the liver before reaching systemic circulation.
This reduces the active concentration of the drug available in the bloodstream.
What is the sequence of events during first-pass metabolism?
The drug is absorbed from the gut into the portal vein.
Blood carrying the drug enters liver sinusoids.
Hepatocytes metabolize part of the drug, reducing its active concentration.
The “cleaned” blood then exits through the central vein → hepatic vein → systemic circulation.
What is the pharmacy relevance of first-pass metabolism?
It can significantly reduce oral drug bioavailability, meaning less active drug reaches circulation.
Drugs subject to high first-pass metabolism require higher oral doses or alternative routes.
Some routes bypass the liver (e.g., sublingual, rectal, intravenous) to avoid this effect.
What is an example of a drug affected by first-pass metabolism?
Propranolol, morphine, and nitroglycerin undergo extensive first-pass metabolism, reducing their bioavailability when taken orally.
Nitroglycerin is therefore given sublingually to bypass the liver.
What factors can influence first-pass metabolism?
Liver enzyme activity (CYP450 system efficiency).
Liver disease (cirrhosis or hepatitis decreases metabolism).
Drug interactions (enzyme inhibitors or inducers).
Age, genetics, and nutrition.
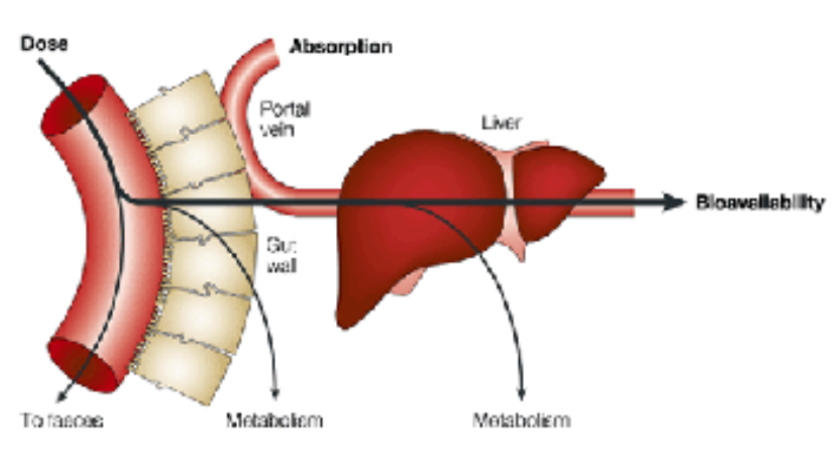
PHOTO What does the first-pass metabolism diagram illustrate?
It shows how oral drugs travel from the GI tract → portal vein → liver before entering systemic circulation.
The diagram usually highlights drug concentration decreasing between the gut and systemic blood due to hepatic metabolism.
Arrows may mark the metabolic conversion of drugs within hepatocytes and the reduced active fraction leaving the liver.
Key takeaway: explains why oral bioavailability is often lower and why alternative administration routes are sometimes required.
What is the purpose of drug biotransformation in the liver?
Biotransformation converts lipid-soluble drugs and toxins into more water-soluble metabolites for easier excretion via urine or bile.
It typically occurs in two stages: Phase I (functionalization) and Phase II (conjugation).
What occurs during Phase I reactions?
Functionalisation
Involves cytochrome P450 (CYP450) enzymes. - located in SER in hepatocytes - carry out metabolism reaction like the 3 below.
Reactions: oxidation, reduction, and hydrolysis.
Purpose: introduce or expose functional groups (e.g. –OH, –NH₂, –COOH).
Can produce active, inactive, or sometimes reactive metabolites like NAPQI formed by metabolism from paracetamol.
Example: CYP2D6 converts codeine to morphine (activation of a prodrug).
What occurs during Phase II reactions?
Involves conjugation with polar groups such as: (attached to functional group in molecule)
Glucuronidation
Sulphation
Acetylation
Glutathione conjugation
Makes metabolites more water soluble → facilitates renal or biliary excretion.
Usually detoxifies Phase I products, though some conjugates may remain toxic.
What is the overall outcome of biotransformation?
Lipid-soluble drugs/toxins → water-soluble metabolites → excretion via urine or bile.
This prevents accumulation of harmful substances and regulates drug clearance.
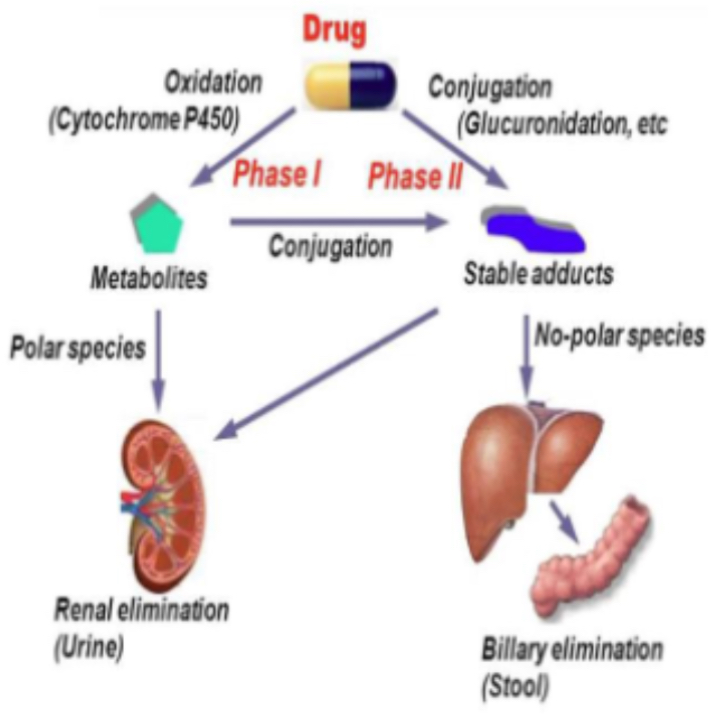
PHOTO What does the biotransformation diagram show?
It illustrates Phase I and Phase II pathways for drug metabolism.
Usually labels CYP450 enzyme sites, oxidation/reduction reactions, and conjugation reactions.
Shows how parent drug molecules become hydrophilic and ready for excretion.
Key takeaway: explains the two-step detoxification system that determines drug half-life and toxicity risk.
What is bile and why is it important?
Bile is a digestive and excretory fluid produced by hepatocytes, composed of:
Bile salts, phospholipids, cholesterol, bilirubin, and water.
Essential for fat digestion, absorption of fat-soluble vitamins (A, D, E, K), and elimination of waste.
How much bile does the liver produce daily?
Approximately 600–1000 mL per day.
It is continuously synthesized by hepatocytes and stored in the gallbladder.
How is bile stored and released?
Stored in the gallbladder where it becomes up to 10× more concentrated.
Released into the duodenum via the common bile duct after fatty meals.
Cholecystokinin (CCK) triggers bile release.
What is bile’s role in digestion?
Emulsifies fats → breaks large lipid droplets into smaller micelles.
Enables pancreatic lipase to access triglycerides.
Aids absorption of fat-soluble vitamins.
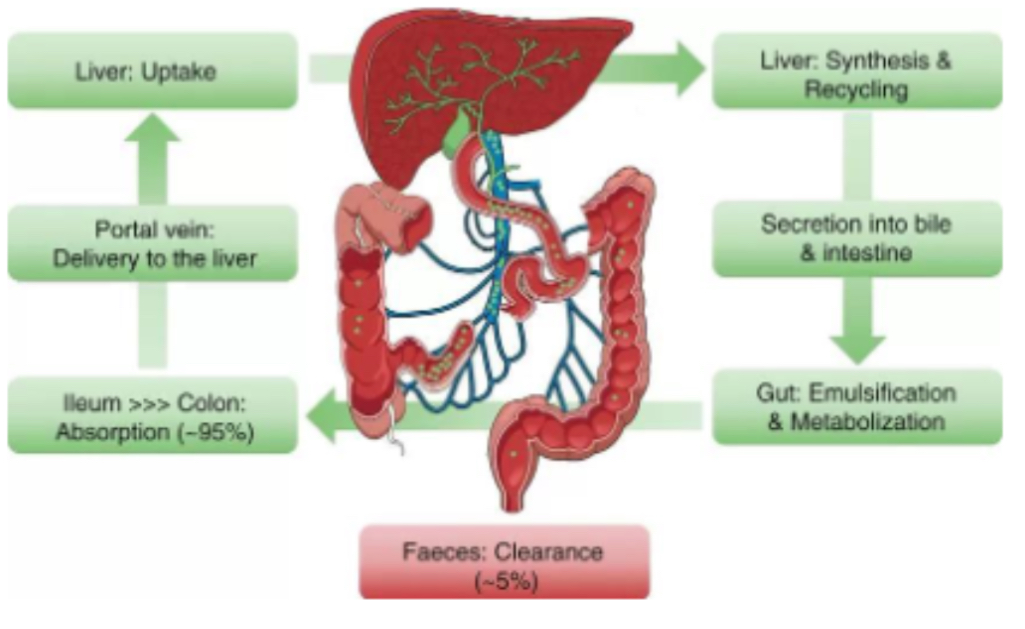
PHOTO What does the bile production and flow diagram show?
Displays bile synthesis in hepatocytes, its movement through canaliculi → bile ducts → gallbladder → duodenum.
Illustrates opposite flow to blood within the hepatic lobule.
Often labels CCK, bile salts, and micelle formation.
Key takeaway: emphasizes bile’s dual role in digestion and drug metabolite excretion.
What is the hepatic lobule?
It’s the structural and functional unit of the liver, arranged in a hexagonal shape around a central vein.
What makes up the portal triad?
Hepatic artery – delivers oxygen-rich blood.
Portal vein – delivers nutrient- and drug-rich blood.
Bile duct – drains bile in the opposite direction of blood flow.
How does blood flow through the hepatic lobule?
Blood flows from the periphery (portal triad) → through sinusoids → toward the central vein.
As it passes, hepatocytes metabolize nutrients, drugs, and toxins.
How does bile flow in the lobule?
Bile flows opposite to blood: from hepatocytes (centre) → bile canaliculi → bile ducts (periphery).
What is the role of Kupffer and Stellate (Ito) cells in the hepatic lobule? And pharmacy relevance
Kupffer cells: remove microbes and debris within sinusoids (immune defense).
Stellate cells: store vitamin A and can produce collagen during fibrosis.
Pharmacy relevance:
Drugs such as methotrexate and amiodarone can activate stellate cells → fibrosis and hepatotoxicity.
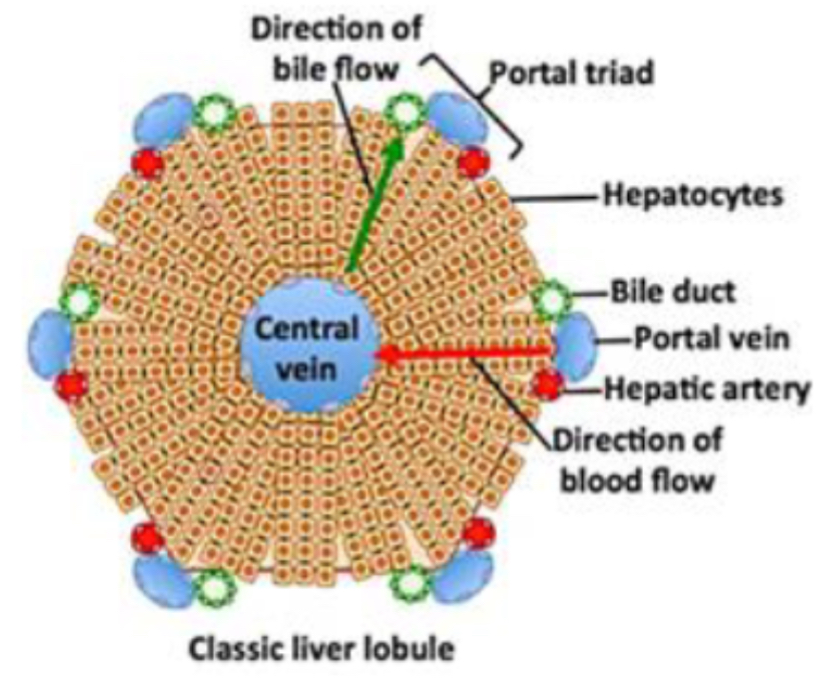
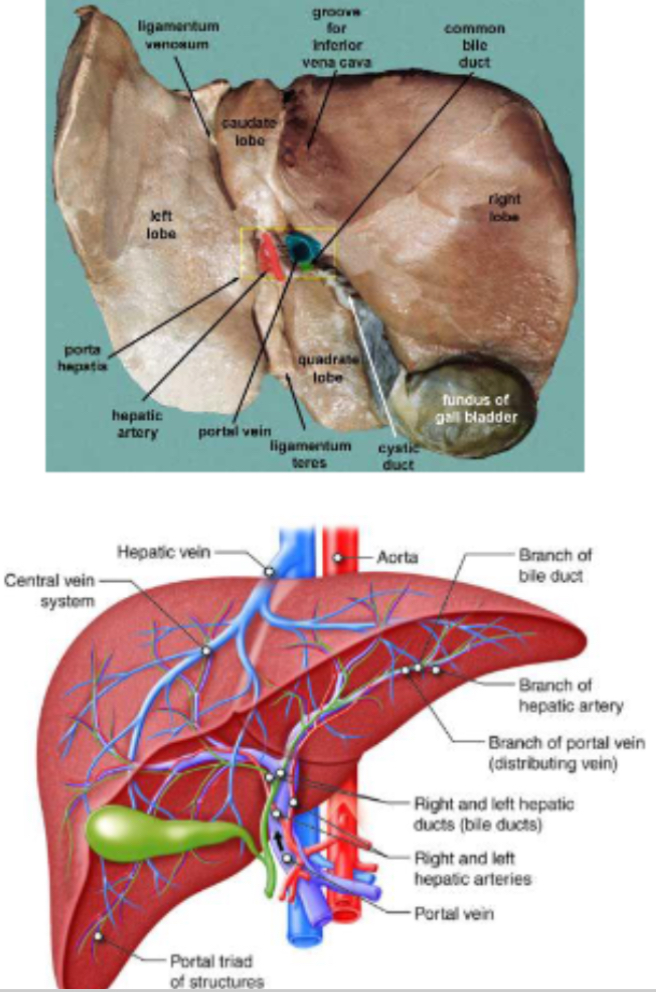
PHOTO What does the hepatic lobule diagram show?
A hexagonal structure representing a lobule.
At each corner: portal triad (hepatic artery, portal vein, bile duct).
Blood flow: periphery → central vein.
Bile flow: opposite direction, toward bile ducts.
Highlights Kupffer and Stellate cells and their positions.
Key takeaway: visually explains the opposing flow of blood and bile and how detoxification occurs before blood returns to circulation.
Can the liver regenerate itself?
Yes — the liver can regenerate from as little as 25% of its original mass.
This is driven by hepatocyte proliferation and growth factors such as HGF (hepatocyte growth factor) and TGF-α.
Regeneration is vital for recovery after injury or surgery.
What are the main causes of liver damage or disease?
Hepatitis – inflammation causing enzyme leakage (↑ ALT, AST).
Fatty liver disease – accumulation of lipids impairs metabolism.
Cirrhosis – fibrosis replaces hepatocytes → loss of functional tissue.
Drug-induced liver injury (DILI) – caused by hepatotoxic medications.
What are the pharmacy implications of liver disease?
Reduced enzyme activity → prolonged drug half-life (e.g., diazepam, warfarin).
Low albumin → increased free drug fraction → higher toxicity risk.
Dosage adjustments needed using Child-Pugh score.
Early recognition of hepatotoxicity is a key pharmacist responsibility.
What laboratory markers indicate liver damage?
ALT (alanine aminotransferase) and AST (aspartate aminotransferase) rise in hepatocellular injury.
ALP and bilirubin may increase in cholestatic damage.
Albumin and prothrombin time reflect liver synthetic function.
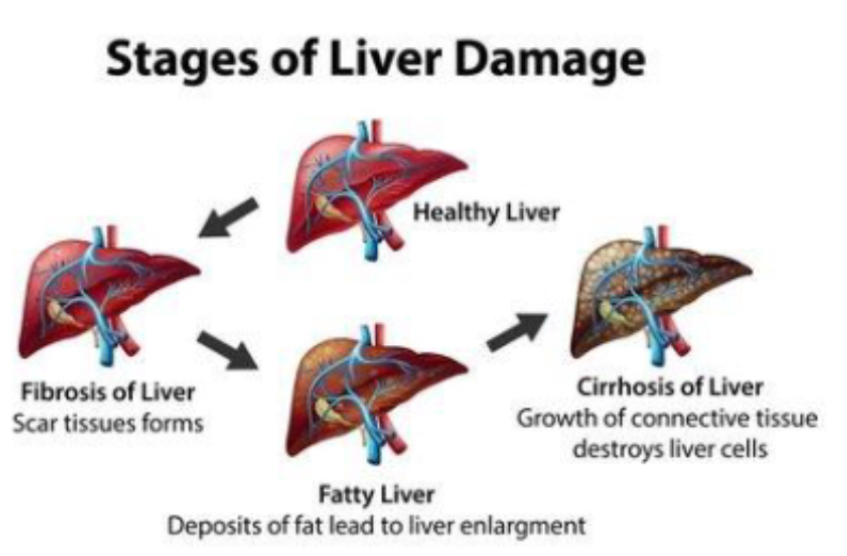
PHOTO What does the liver regeneration and damage diagram show?
It contrasts healthy liver tissue with damaged or fibrotic liver.
Shows hepatocyte proliferation during regeneration and collagen deposition in cirrhosis.
May label growth factors (HGF, TGF-α) and activated stellate cells producing scar tissue.
Key takeaway: highlights the balance between regeneration and fibrosis, showing how chronic injury can lead to irreversible liver disease.