Antibody-based cancer therapies
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
26 Terms
What are the different Antibody-Based Approaches?
Basis of concept:
antibodies directed towards antigens (i.e., biomarkers) relevant to tumour cells - this gave rise to several strategies below
1) Single Agents (Monospecific Antibodies) – Target a single antigen.
2) Bispecific Antibodies – Recognise two different antigens.
3) Antibody-Drug Conjugates (ADCs) – Antibodies linked to cytotoxic agents.
4) Antibody-Radionuclide Conjugates – Antibodies linked to radioactive elements.
5) Antibody-Nanoparticle Conjugates – Antibodies linked to nanoparticles/liposomes.
6) ADEPT (Antibody-Directed Enzyme Prodrug Therapy) – Uses enzyme-antibody complexes to activate prodrugs at tumour sites.
What is the role of monoclonal antibodies in cancer therapy?
diagnosis and treatment of cancer
Describe the structure of antibodies
Recognition (antigen-binding sites): Variable regions that bind to specific antigens.
Heavy and light chains: Heavy chains are held together by hydrogen bonds, van der Waals forces, and disulphide bridges.
Hinge region: Provides flexibility to interact with antigens.
-They have sugar chains added to some of their amino acid residues (i.e., they are glycoproteins).
-The basic functional unit of each antibody is an immunoglobulin (Ig) monomer (containing only one Ig unit).
Note: some antibodies can also be
▪ Dimeric with two Ig units
▪ Tetrameric with four Ig units
▪ Pentameric with five Ig units
The variable parts of an antibody are its V (Fab) regions (determines what antibody binds to), and the constant part is its C (Fc) region.
What is hybridoma technology, and how does it produce monoclonal antibodies (MABs)?
- Involves the formation of hybrid cell lines called hybridomas by
fusing a specific antibody-producing B cell with a myeloma cell
selective for its ability to grow in tissue culture and for an absence
of antibody chain synthesis
- The antibodies produced by the hybridoma are all of a single
specificity and are therefore MABs
- Select a particular clone and grow it, they produce a pure antibody
of a particular type
-Done by injecting antigens into a mouse which will produce antibody producing plasma cells (B cells)
-Fused with myeloma cells to make hybridomas
-Grown in culture
-Clones tested for desire antibody
-Desired clones are cultured and frozen
What are the issues with mouse antibodies?
-Immunogenicity o Short half-life
o Limited penetration into tumour sites
o Poor ability to recruit host effector functions
What are the different types of monoclonal antibodies used in cancer therapy - state the relevance of immunogenecity of each
1) Murine (Mouse-derived) – High immunogenicity (risk of anaphylaxis).
2) Chimeric (Part mouse, part human) – Murine variable regions fused onto human constant regions = Reduced immunogenicity and increased serum half life
3) Humanised (Mostly human 95%, part mouse variable regions) – Produced by grafting murine hypervariable amino acid domains into human antibodies = Even lower immunogenicity but decreased affinity to antigen - engineering has been done to increase this
4) Fully Human Antibodies – Least immunogenic, made using recombinant DNA, transgenic mice, or phage display. - Human immunoglobulin genes are transferred into the murine genome. Transgenic mice are then vaccinated with desired antigen leading to production of fully human antibodies
Suggest reasons for why it took so long for antibody-based anticancer agents to become common practice
-to technical challenges (manufacture, purification, stability and immunogenicity problems)
- For solid tumours, de-bulking may be needed initially
- Early antibody therapies most efficacious when used in combination with traditional
cytotoxic agents
How do single agent 'naked antibodies work' (MOA's)
A. Interfering with Cell Signalling
-Many tumour cells have receptors that interact with growth factors (e.g., TGF-alpha).
Antibodies block receptor dimerisation, preventing the activation of signalling pathways (signals tumour to grow)
Example: Trastuzumab (Herceptin) binds HER2, blocking its interaction with HER3 (its partner receptor - or two HER2 molecules) to inhibit signalling e.g. in breast cancer cells.
Note: targets (antigens) of these antibodies sit on the cell surface
B. Interfering with Vasculature
-VEGF (Vascular Endothelial Growth Factor) stimulates blood vessel growth by binding VEGF-R receptors (on endothelial cells).
Bevacizumab (Avastin) is an antibody that binds VEGF = can't bind to its receptor , preventing it from stimulating angiogenesis.
Note:
-In order for a tumour to grow it must bring blood vessels to the tumour as it
grows rapidly for nutrients and get rid of waste products
-Centre of tumour often necrotic due to poor blood supply = hard for chemo to erradicate this centre
C. Checkpoint Inhibitors
-Immune checkpoints are receptors on immune cells that prevent the super activation of the immune system
-Cancer cells try to overexpress these receptors to accentuate this hiding the cancer cells - over engaging of the immune checkpoints
-Tumour cells express PD-L1 ligands, which binds to PD-1 receptors on T cells, turning them off.
-Tumour cells also exploit CTLA-4 receptors to suppress T-cell activity.
Main inhibitors for this:
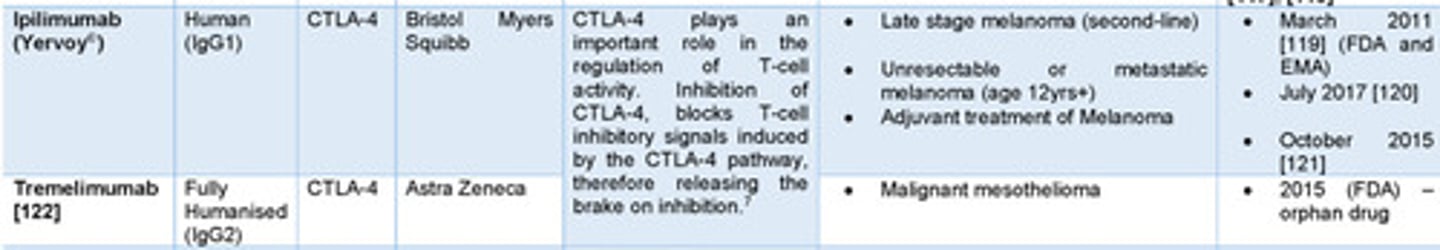
-CTLA-4 inhibitors: Block T-cell suppression (e.g., Ipilimumab for melanoma).
-PD-1 inhibitors: Block PD-1 on T-cells, reactivating immune response (e.g., Pembrolizumab, Nivolumab).
-PD-L1 inhibitors: Block PD-L1 expression on tumour cells (e.g., Atezolizumab)
What are the 2 stimuli T cells need to be activated?
Signal 1: Recognition of a specific antigen presented by MHC molecules on antigen-presenting cells (APCs) by the T cell receptor (TCR)14.
Signal 2: Co-stimulation provided by the interaction between co-stimulatory molecules on APCs (such as CD80/CD86) and receptors on T cells (such as CD28)
What is the normal moa of tumour cells at CTLA-4?
Function: CTLA-4 is an immune checkpoint that suppresses T-cell activation.
Expression: Found on activated T-cells and regulatory T-cells (Tregs).
Binding: Competes with CD28 for B7 ligands (CD80/CD86) on antigen-presenting cells
T-cell Suppression:
-Outcompetes CD28, preventing co-stimulation
-Inhibits T-cell signaling cascades
-Reduces production of factors needed for T-cell activation
-Boosts activity of regulatory T-cells, further suppressing immune response.
-Allows cancer cells to avoid detection by dampening T-cell responses
examples: Ipilimumab or Tremelimumab
Examples of Well-Known Single-Agent Antibodies
-🔹 Trastuzumab (Herceptin®)
Type: Humanised monoclonal antibody
Target: HER2/neu receptors (Human Epidermal Growth Factor Receptor 2)
Mechanism: Blocks HER2 signalling, preventing tumour growth.
Use: Breast cancer (HER2-positive
-Cetuximab (Erbitux®)
Type: Chimeric monoclonal antibody (part mouse, part human).
Target: Epidermal Growth Factor Receptor (EGFR)
Mechanism: Inhibits EGFR signalling, which drives tumour growth.
Use: KRAS-wild-type colorectal cancer (ineffective in KRAS-mutant cases)
-Bevacizumab (Avastin®)
Type: Monoclonal antibody
Target: Vascular Endothelial Growth Factor (VEGF)
Mechanism: Blocks angiogenesis (prevents new blood vessel formation).
Use: Metastatic colorectal cancer (first-line therapy with 5-FU)

What are the moa's of PD-1 Inhibitors
-Ligand blockade: Inhibits PD-1 binding to PD-L1/PD-L2 on tumor/stromal cells
-Immune reactivation:
-Epitope specificity:
Pembrolizumab/nivolumab bind distinct PD-1 regions
What are the moa's of PD-L1 Inhibitors?
Dual blockade: Prevents PD-L1 interaction with both PD-1 and B7-1 (CD80)
Fc engineering: Modified IgG1 Fc region minimizes ADCC/ADCP to preserve PD-L1+ T-effector cells
Tumor selectivity: Targets PD-L1-overexpressing cancers (e.g., triple-negative breast cancer)
What are the moa's of CTLA-4 inhibitors? - Restores 2nd signal (1st signal is between antigen and t cell receptor)
-Blocks CTLA-4's interaction with B7 ligands on antigen-presenting cells
-Prevents CTLA-4-mediated suppression , allowing CD28/B7 costimulatory signaling to proceed
-Depletes regulatory T cells (Tregs) via FcγR-mediated antibody-dependent cellular cytotoxicity (ADCC)
-Enhances T-cell infiltration into tumors#
e.g.
- PD-1 Inhibitors: Genentech attaches to PDL-L1 to switch T cell back on
- Can lead to toxicity
When these single agent antibodies sit on the surface receptors (antigens) of tumour cells, how do they kill them ? - 2 ways
1) Antibody-Dependent Cell-Mediated Cytotoxicity (ADCC)
The Fc region of the antibody binds to T-cell Fc receptors, bringing immune cells close to the tumour cell.
This triggers tumour cell destruction via natural killer (NK) cells (which cause a release of chemical mediators e.g. granzyme B) or macrophages both = apoptosis
2) Complement-Dependent Cytotoxicity (CDC)
Antibodies activate the complement system (comprises a number of proteins in the blood that can cause cell death after an antibody binds to the cell surface), forming protein complexes that lead to tumour cell lysis. . Once triggered, cell death occurs by a number of mechanisms including activation of the membrane attack complex (i.e., complement-dependent cytotoxicity), enhancement of antibody-dependent cellmediated cytotoxicity, or CR3-dependent cellular cytotoxicity
Both release proteases to punch holes in the tumor cells
What is mutational burden? effect on T cells likelihood of killing them
-However many mutations a tumour has
-= A lot of mutant antigens = easier for T cell to find them
How can we make cheaper MAbs?
-Using biosimilars (when MAbs go off license)
e.g. Rituximab
-Not as easy as making a small molecule (the licensed drug)
How do bispecific monoclonal antibodies (BsMABs) work? provide an example
-Through multistep targeting
-Each arm of the antibodies variable region binds a different target antigen
Example: Blinatumomab
One arm binds CD19 on B-cell lymphoma cells.
The other arm binds CD3 on T-cells, bringing them together to kill tumour cells.
What is DNA payload ?
a specific DNA sequence or molecule that is designed to be delivered and act within cells, often for therapeutic purposes like gene editing or causing cell death
How do Antibody drug conjugates work (ADCs) ?
- Take an antibody and through a chemical linker you attach a highly cytotoxic
drug (DNA payload is attach to antibody for specific antigen)
-Antibody binds to tumour antigen
-The antibody-payload complex is internalised trafficked to the lysosome into the tumour cell by binding to antigen cell surface
-Lysosome has proteases to break down chemical linker between payload and
antibody
-Payload goes into DNA damages it and kills cell (May also leave cell and kills other cells)
Note:
Depends on type of payload and whether it can cross cell membrane
Examples:
1) Microtubule-targeting agents
-Auristatins (MMAE) – Used in Brentuximab Vedotin (Hodgkin’s lymphoma).
-Taxanes (Paclitaxel, Vincristine) – Disrupt microtubules, stopping cell division.
2) DNA-targeting agents
Trastuzumab Deruxtecan (HER2 ADC) – Releases a DNA-damaging payload to kill tumour cells.
Structure of ADC
But they are very hydrophobic, if too much then they are difficult to conjugate
to an antibody-
What are key characteristics of ADC payloads?
Highly cytotoxic (cannot be used as free drugs).
Hydrophilic enough to prevent aggregation.
Stable in circulation but released effectively inside the tumour.
What are the challenges with ADCs?
-Linker Stability: The linker must be stable in the bloodstream but cleave at the tumour site.
-Bystander Effect: If the drug leaks out, healthy cells may be damaged (they have profound side
effects because payload comes off linker prematurely causing toxicity, but can be a good thing as it can kill cancers around)
-Drug-Antibody Ratio (DAR): The right number of drug molecules (payload) must be attached to the antibody for efficacy - must be efficacious but not toxic and must be consistent
How can we achieve uniformity in terms of Drug-Antibody Ratio (DAR)?
2 options :
Lysine Residues:
-Payloads and linkers can be conjugated to lysine residues located across the surface of antibodies.
-Lysine residues have nucleophilic amine groups that react with linker-payload molecules.
Issue: This method can produce a heterogeneous mixture of ADC species with varying DAR values, leading to regulatory challenges.
Disulfide Bridges:
-ADCs can utilize the 8 disulfide bridges that hold antibody heavy and light chains together.
-Reduction of these bridges exposes nucleophilic thiol groups, which can react with linker-payload molecules.
Issue: This approach also generates multiple ADC species, contributing to heterogeneity, hydrophobicity, rapid clearance, and low tolerability in vivo.
Main challenges with heterogenous Drug-Antibody Ratio (DAR)?
-complicate manufacturing, analysis, and quality control processes
-High DAR species often exhibit poor PK profiles due to increased hydrophobicity and faster clearance.
-can lead to unpredictable toxicity profiles, reducing clinical efficacy.
What are the different types of linkers?
-Protease linkers
-PH sensitive linkers - e.g. more acidic tumour environment due to higher metabolism and secretion of lactate