Behavioural medicine
1/26
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
27 Terms
What does biopsychosocial mean?
-biological, psychological and social (environmental) factors (are involved in health and illness)
Give examples of biological factors involved in health and illness
-genetics, microbiology, pharmacology
Give examples of social factors involved in health and illness
-socioeconomic status (can affect life expectancy for example)
-occupational health
-public and environmental health
-education
What are the 2 types of health behaviours?
-health-protective e.g. exercise, sleep (7-8)
-health-impairing e.g. poor diet, smoking
Give examples of psychological factors involved in health and illness. Give examples of direct and indirect effects of psychological factors
-behaviour
-beliefs and attitudes
-habits and lifestyle
-motivation e.g. with taking meds
Direct effects for example: smoking, exercise, diet.
-Indirect effects: not taking meds, delay in seeking treatment
2/3rds of all deaths are due to…
the 2 big C’s: cancer and cardiovascular disease
What is health psychology?
-the study of psychological and behavioural processes in health, illness and healthcare. Focuses on how psychological, cultural and behavioural factors contribute to physical health and illness
What is behavioural medicine?
-the study of the relevancy of environmental, biomedical and behavioural knowledge relevant to health and disease.
What is behavioural pharmacy?
-applying behavioural medicine and health psychology in pharmacy settings
Give examples of where health psychology is applied
-the promotion and maintenance of health e.g healthy eating and physical activity
-the prevention and management of illness and addictions e.g. smoking, alcohol, sexual health, pain, adherence
-improving healthcare system e.g. screening, pt communication
-understanding and optimising adherence to treatment
-stress management (many studies have shown that less stress=improvement of health and physical healing of the body)
Give examples of self care
-smoking cessation, diet, exercise
What are examples of how pharmacists help in terms of behavioural medicine?
-offering screening for pts at high risk of vascular disease
-using new technologies to expand choice and improvement
-weight management
-flu vaccines
What is non-adherence?
-when a person doesn’t follow a prescribed or agreed-upon course of action, especially regarding medication, treatment plans, or lifestyle recommendations.
What are the 3 categories of the consequences of non-adherence?
-patient
-healthcare providers/payers
-pharmaceutical industry
Give 3 consequences of non-adherence on the pt
• Worsening condition and more intensive treatments
• Increased treatment costs
• Illness impact on work and livelihood, so more financial burden
What are the consequences of non-adherence on healthcare providers/payers?
• Costs of wasted medicines BUT ‘knock on’ costs are greater:
-Doctor thinks treatment not working and escalates to more intensive (expensive treatment) , which leads to additional medical tests and investigations. Even hospitalisation
What are the consequences of non-adherence on the pharmaceutical industry?
-bad reputation. Healthcare professionals may think that the medication isn’t working or isn’t good enough
Difference between compliance and adherence
-adherence involves pt in decision. ‘‘are you comfortable with this treatment decision?’’
-acknowledges patient’s right to decline treatment and noncompliance is no reason to blame the patient
What are the 3 behaviours in adherence and what do they mean?
1. Initiation – Do they start on time?
2. Execution- Do they use it as advised (eg twice daily after food)?
3. Persistence – Do they continue with treatment for the recommended duration? (problem especially in people who have long-term conditions)
What does primary non-adherence mean?
-pt doesn’t even start the treatment course
What is non-persistence?
-pt stops their treatment course earlier than they should
-usually more common than primary non-adherence
Give 4 myths about non-adherence and explain them
-everyone who has a long-term health or a life-threatening condition is good at adhering to treatment plan
-non-adherent pts all share a common trait. Not true. No consistent links to show age, gender, socioeconomic status etc as being a certainty in non-adherence. e.g. some studies have shown older pts adhere more than younger but other studies show the opposite.
-Simplifying the regimen and reducing ‘pill-burden’ solves the problem of nonadherence. Although it can be helpful for some people, this alone usually doesn’t solve the problem. Some people can adhere to complex regimen but not a simple. The key issue is how well the treatment fits in with the individual patient’s routine, expectations and preferences. There are multiple factors usually involved in non-adherence
-Providing more information about a therapy guarantees adherence. Although it’s important, giving more information doesn’t guarantee engagement. To result in action, information must either: Agree with our existing beliefs OR Change them
Relationship between route of administration and adherence
-easier the route of administration, the more likely they will adhere
If the patient trusts the messenger…
-the trust the message
Explain the perceptions and practicalities approach
-perceptions=’don’t want to’. Intentional non-adherence
-practicalities=’i can’t’. Unintentional non-adherence
-The many causes of non-adherence fall into two overlapping categories: intentional and unintentional. We need to consider two issues: motivation and ability (resources).
-Unintentional non-adherence occurs when the patient wants to take the medicine but is prevented from doing so by barriers beyond their control e.g. poor recall or comprehension of instructions, difficulties in administering the treatment, simply forgetting or because they can’t afford it. These are practical barriers
- Deliberate or intentional non-adherence arises when the patient decides not to follow the treatment recommendations. Usually involves the beliefs and preferences influencing the person’s motivation to start and continue with treatment. These are perceptual barriers
- Each individual has a unique mix of perceptual and practical barriers to adherence, and interventions should be tailored to meet the needs of individuals by first assessing the specific barriers and then selecting appropriate techniques to address each
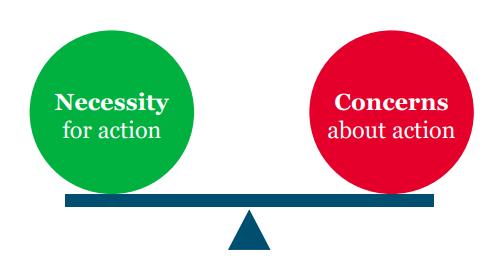
- Research has shown that the beliefs influencing adherence may be operationalised by the Necessity Concerns Framework
What should be the first barriers that need to be overcome in pts who aren’t adhering?
-beliefs, even if actually taking the medication is easier
-We need to understand how people really think about illness and treatment and how this determines their response to treatment advice
Explain the necessity concerns framework
-framework based on beliefs leading to non-adherence
-necessity=
• ‘How much do I need to do this to achieve something that is important to me?’
• ‘Can I get away without doing it?’
-if pt feels it’s necessary and the best option, they are more likely to adhere
-concerns=
• What are the ‘downsides’?
• What are the potential adverse consequences of following the advice?
• How much do they concern me?
-some pt’s have beliefs that the medication will do more harm than good
-the pt’s beliefs could be about all medicines or specific medicines