NURS 333 Module 2 Labor and Delivery
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
63 Terms
hospitals
- Over 98% of deliveries occur in hospitals (2012)
- Provides access to key personnel, equipment, pain control options, and emergency services
home births
- 88% of home births are intentional; 12% precipitous
- Many choose home births because of negative hospital experiences
- Women may feel more comfortable, empowered, and in control at home
birthing centers
- Generally freestanding centers are not located in a hospital.
- Midwives attend most births in birthing centers.
- Cater to women with low-risk pregnancies.
- Transfer agreements with local hospitals.
Involuntary uterine contractions
Occur in upper 2/3 of uterus
Apply pressure to fetus → pressure to amniotic fluid, lower portion of uterus & cervix → cervix dilated and effaced → allows for passage of fetus, amniotic fluid, membranes, placenta
Ferguson reflex
reflex contractions (urge to push) of the uterus after stimulation of the cervix when the presenting part of the fetus reaches the perineal floor
voluntary contraction
Muscle contraction under conscious control.
dilation
how open they are
0-10 cm
effaced
0-100%
10 cm
When should secondary powers (i.e., voluntary pushing) start?
The muscles of the pelvic floor
help turn and orient the fetus
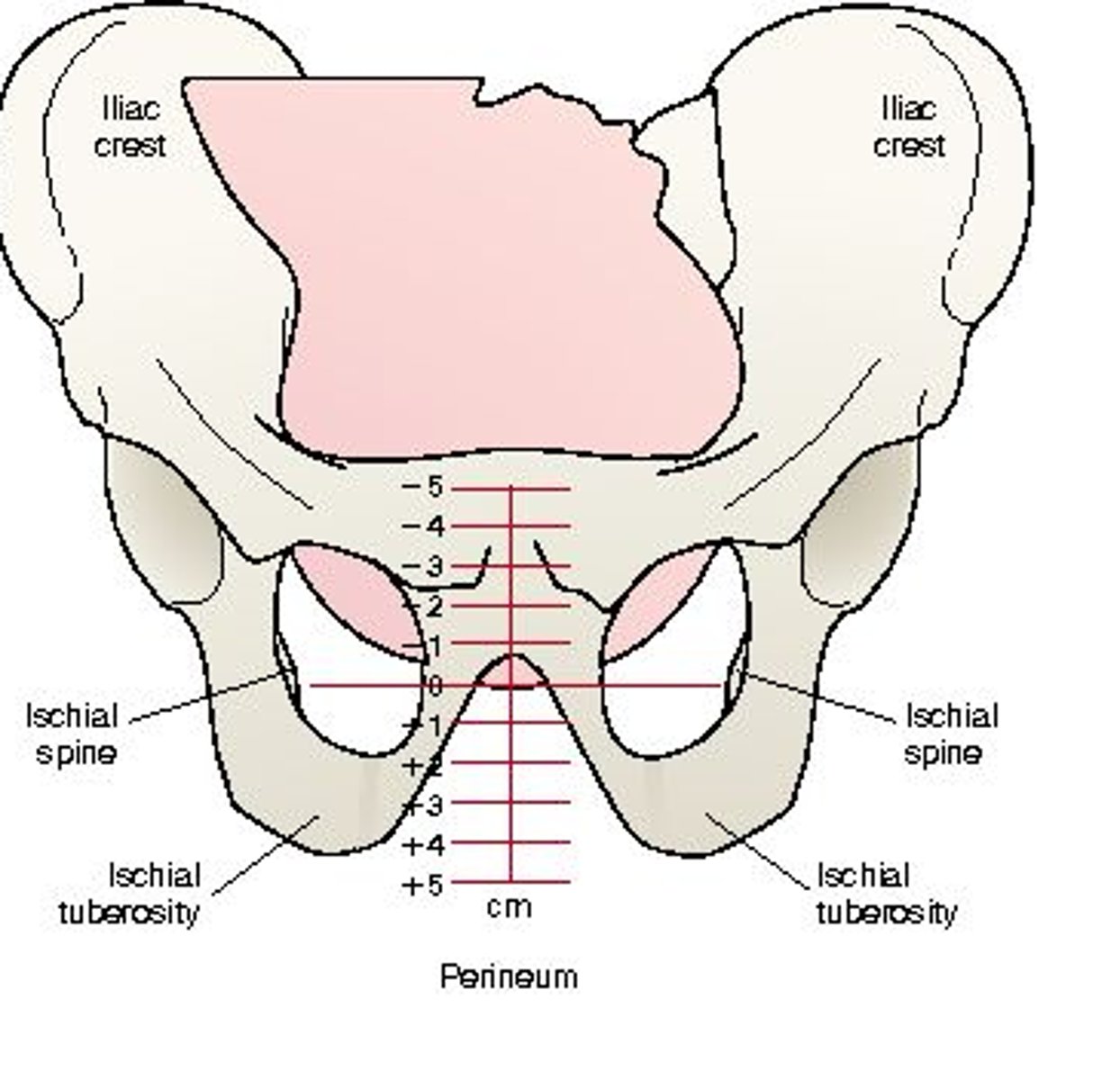
fetal station
The relationship between the fetal presenting part and the pelvis is assessed by
zero station
The level of the ischial spines is referred to as
the presenting part has reached zero station
Fetus is engaged when?
station
-5 to +5
fetal head size
Typically the largest part of fetus
Unfused skull bones allow for head to change in reference to birth canal
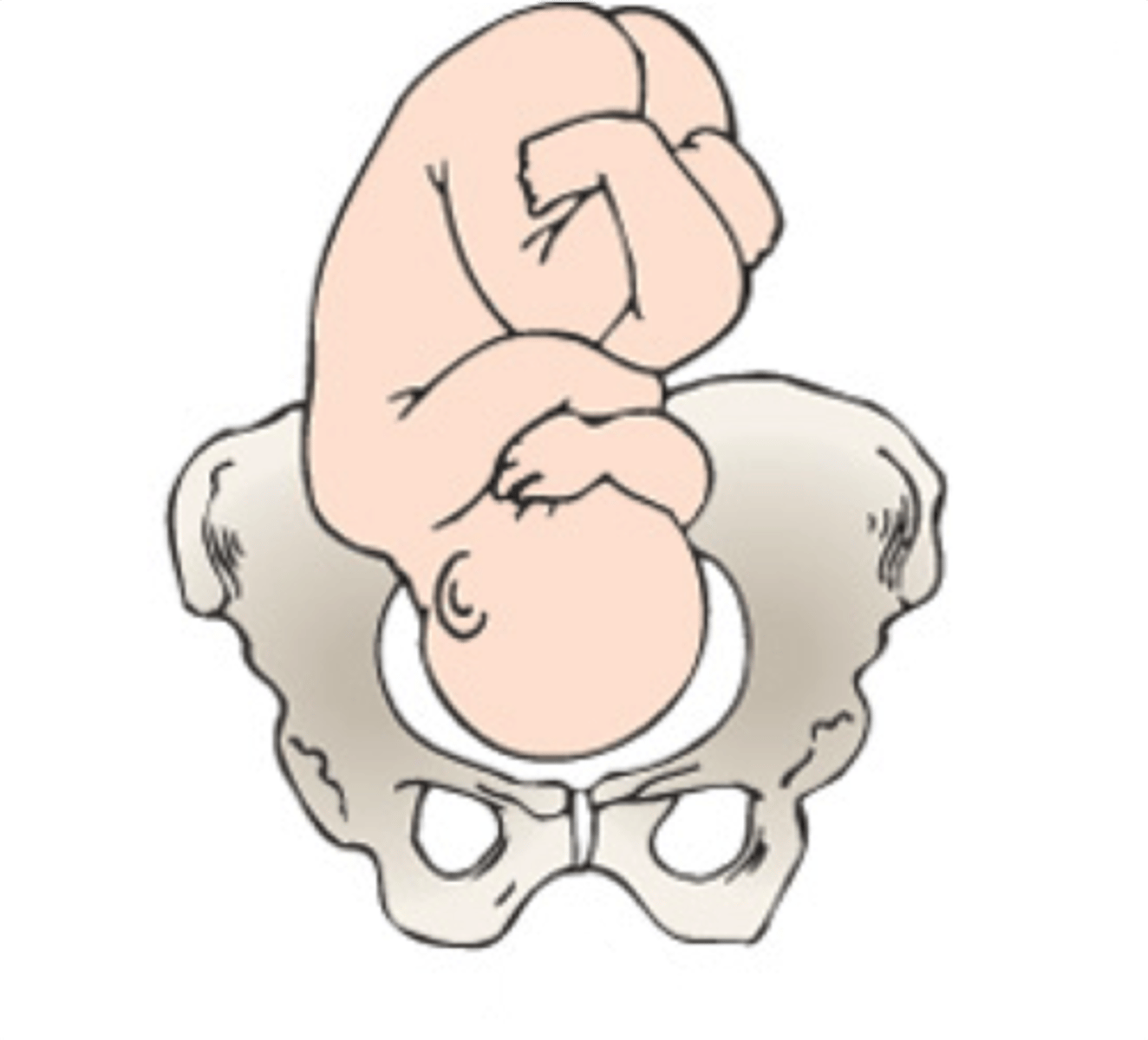
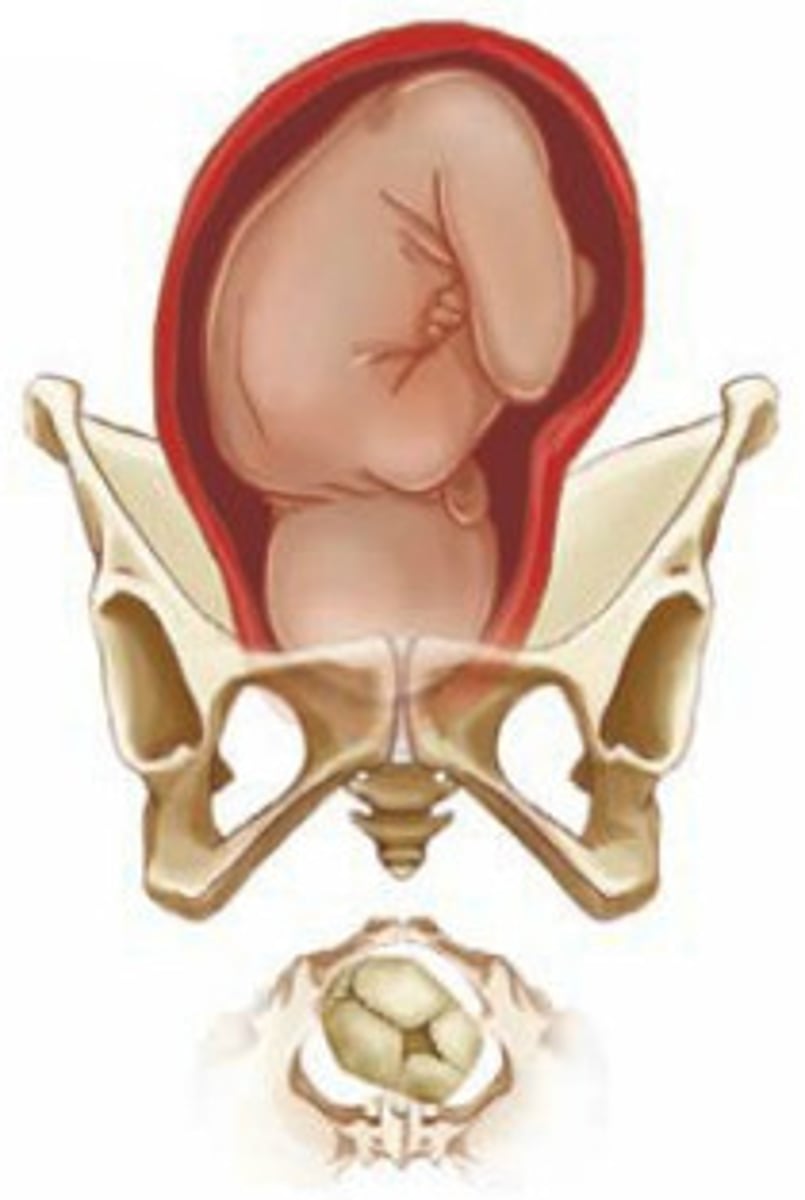
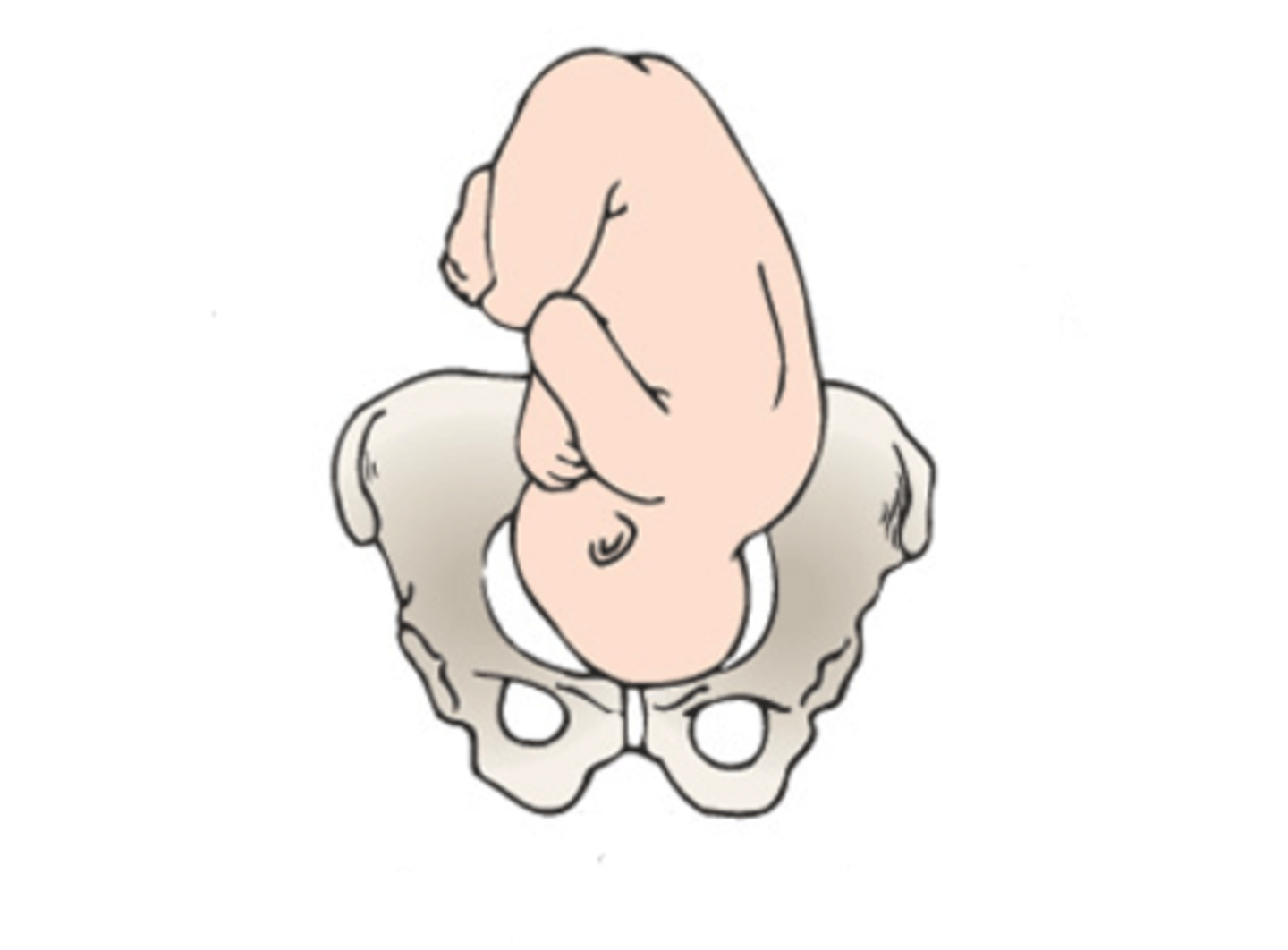
fetal presentation
The part of the fetus that enters the pelvis 1st (presenting part)
Majority of fetuses enter pelvis head first - AKA cephalic presentation
Other presentations: breech (buttocks or feet) & shoulder
fetal attitude
Position of fetal body parts in relationship to one another (flexion/extension)
Typical attitude = flexed neck, arms, legs & rounded back - optimal!
fetal lie
Relationship of the long axis of the fetus to the long axis of the mother
Longitudinal or transverse (rare: oblique)
Passenger: Fetal Position
Described w/ a series of 3 letters
1st letter = Right (R) or Left (L) - Refers to MATERNAL R or L
2nd letter = Presenting part (fetal)
Occipital bone (O): vertex presentation
Chin (mentum [M]): brow/face presentation
Buttocks (sacrum [S]): breech presentation
Scapula (acromion process [A]): shoulder presentation
3rd letter = position of the presenting part as
Posterior (P)
Anterior (A)
Transverse (T)
Examples:
Left Occiput Anterior (LOA)
Occiput Posterior (OP)
![<p>Described w/ a series of 3 letters</p><p>1st letter = Right (R) or Left (L) - Refers to MATERNAL R or L</p><p>2nd letter = Presenting part (fetal)</p><p>Occipital bone (O): vertex presentation</p><p>Chin (mentum [M]): brow/face presentation</p><p>Buttocks (sacrum [S]): breech presentation</p><p>Scapula (acromion process [A]): shoulder presentation</p><p>3rd letter = position of the presenting part as</p><p>Posterior (P)</p><p>Anterior (A)</p><p>Transverse (T)</p><p>Examples:</p><p>Left Occiput Anterior (LOA)</p><p>Occiput Posterior (OP)</p>](https://knowt-user-attachments.s3.amazonaws.com/50ae9365-68b8-440a-b088-bbb3df531b4c.jpg)
ROP
LOP

ROA
LOA
psyche
A woman's psyche can impact labor
Examples of factors that can delay labor progress:
Anxiety
Stress
Fear
Pain tolerance
Relaxation can augment labor
Childbirth education
Trust in support people & care providers
Doula support
Signs of Labor
Contractions become regular (q 4 min x 1 min for 1 hr //411)
Presence of bloody show
Descent of the fetus into the birth canal (lightening), may occur about two weeks before labor for a primigravida
Nesting impulse
GI distress (heartburn, nausea, diarrhea)
Weight loss of 1 to 3 pounds just before onset of labor
bloody show

first stage of labor
regular contractions that cause progressive dilation and effacement of the cervix (longest stage - divided into 3 phases)
Latent phase: 0-5 cm dilation
Active phase: 6 cm - 10 cm dilation
second stage of labor
starts with complete dilation of cervix, pushing, and ends with the birth of the baby
third stage of labor
begins just after the birth of the baby and ends with delivery of the placenta
fourth stage of labor
begins just after the delivery of the placenta and ends after 4 hours or when the mother becomes clinically stable
Latent phase characteristics (0-5 cm)
Longest lasting phase of labor
Period of excitement for some, anxiety for others
Contractions feel like menstrual cramps (or lower back ache) and are mild to palpation (nose)
Active phase characteristics (6-10 cm)
Women may become more focused, anxious, or restless
Contractions become more regular and painful
Contractions are moderately strong to palpation (chin)
Contractions strong and close together (forehead)
Women may feel out of control, irritable, exhausted, or dependent
May experience N&V, bloody vaginal discharge typical
D. Vaginal examination
A woman states that she thinks she is in labor as she enters the perinatal triage unit. Which of the following assessments will provide the nurse with the most valuable information regarding the client's labor status?
A. Leopold maneuvers
B. Frequency of uterine contractions
C. Fetal heart rate assessment
D. Vaginal examination
A. Check the patient's cervix to determine if the patient is in the transition phase of labor
A patient's cervix was 5 cm dilated and 80% effaced 2 hours ago. She is now agitated, irritable, and her contractions have increased in intensity. What should the nurse do next?
A. Check the patient's cervix to determine if the patient is in the transition phase of labor.
B. Discuss pain medication options.
C. Notify the provider of the patient's change in condition.
D. Prepare for the second stage of labor.
labor pain
Pain is what the patient says it is!
Many factors play a role in pain tolerance, including:
Fear
Previous experiences with labor pain
Support system
Fatigue
Manifestations of pain include:
Pain in abdomen, low back, or thighs with contraction
Continuous pain in low back may occur if fetus is in an occiput-posterior position
Continuous abdominal pain may indicate a placental abruption
Opioids for labor pain
Fentanyl—short acting (1-2 hours), may cause maternal or neonatal respiratory depression
Mixed opioid agonist/antagonists for labor pain
Nubain (nalbuphine)—single dose lasts 3 to 6 hours
Stadol (butorphanol)—single dose lasts 3 to 4 hours
Should not be used in women who are dependent on opioids because may cause withdrawal
Less risk of respiratory depression than opioids
Nitrous oxide for labor pain
Self-administered analgesic gas that the patient inhales for 15-30 seconds before the start of each contraction.
Side effects include nausea, vomiting, vertigo and lightheadedness
Epidural Analgesia/Anesthesia
involves injection of local anesthetic and an opioid analgesic into the lumbar epidural space
61% of women receive an epidural in the U.S.
Given continuously throughout labor
Can be used for vaginal deliveries or C-sections
Can potentially increase the duration of 2nd stage of labor
Epidural Analgesia/Anesthesia side effects
Nausea and vomiting
Hypotension *
Fever
Pruritus
Intravascular injection
Maternal fever
Allergic reaction
Respiratory depression
Infuse 1,000 mL of lactated Ringer's IV fluid
Have the woman empty her bladder
Which of the following actions would the nurse expect to perform immediately before a woman receives epidural anesthesia? Select all that apply.
Assess fetal heart rate
Infuse 1,000 mL of lactated Ringer's IV fluid
Place the woman in the Trendelenburg position
Monitor blood pressure every 5 minutes for 15 minutes
Have the woman empty her bladder
true
Is the following statement true or false?
Nonpharmacologic pain management techniques should only be used during the latent phase of labor.
Drop in blood pressure
Immediately following epidural anesthesia administration, the nurse must closely monitor the mother for which of the following side effects?
Numbness and tingling in her legs and feet
Drop in blood pressure
Increase in central venous pressure
Fetal heart accelerations
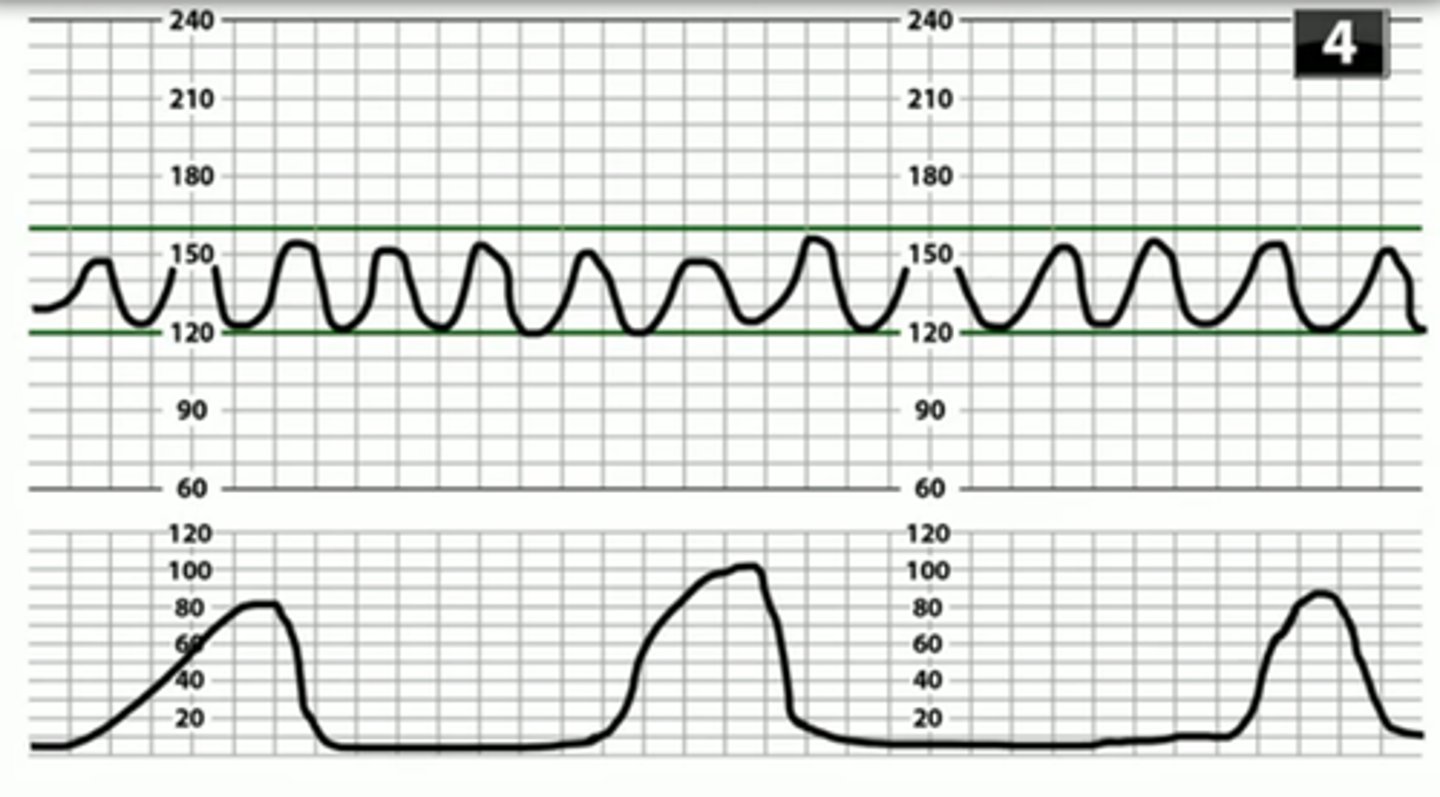
fetal monitoring
Assessment of the fetal heart rate (FHR) for patterns that may indicate fetal compromise
A normal (or reassuring) pattern is associated with positive outcomes for the neonate.
Abnormal (or nonreassuring) patterns are associated with hypoxemia and may lead to fetal hypoxia → metabolic acidosis
When describing FHR pattern, 5 components are assessed:
Baseline FHR
Variability
Accelerations
Decelerations
Uterine contractions
Uterine Contractions
Assessment of uterine contractions looks at the number of contractions during a 10-minute window, averaged over 30 minutes.
NORMAL: ≤ 5 contractions in 10 minutes
TACHYSYSTOLE: > 5 contractions in 10 minutes
(Note: term hyperstimulation is outdated and should not be used)
Intermittent monitoring
includes auscultation of the FHR:
Every 15 to 30 minutes during the active phase of labor
Every 5 to 15 minutes in the second stage of labor
Devices: fetoscope, Doppler ultrasound, pinard stethoscope
Auscultate FHR in conjunction w/ ctx for an entire ctx cycle
Continuous fetal monitoring
s a common practice in the United States.
In low-risk pregnancies, does not reduce risk of cerebral palsy or perinatal mortality as is often thought
With continuous fetal monitoring, a nurse evaluates:
Low-risk pregnancy: Every 30 minutes during the 1st stage of a low-risk woman and every 15 during the 2nd stage.
High-risk pregnancy: More frequent; ~every 15 min during 1st stage, every 5 min during 2nd stage (follow institution's policy)
External Fetal Monitoring (EFM)
Ultrasound transducer for FHR + tocotransducer to detect ctx
Internal Fetal Monitoring
Scalp (or spiral) electrode for FHR
Intrauterine pressure catheter (IUPC) for ctx - measures internal uterine pressure of ctx in Montevideo Units (MVUs)
FHR Baseline
average FHR rounded to 5 bpm
Normal: 110-160 (>160 = tachycardia; <110 = bradycardia)
Monitor between contractions, not including accels/decels, over 10 min
Variability
pattern of fluctuations in the baseline FHR assessed over a 10-min period; based on amplitude
Absent: no amplitude
Minimal: amplitude ≤5 bpm
Moderate: amplitude is 6-25 bpm
Marked: ≥26 bpm
Acceleration
increase in FHR from baseline
Before 32 wks GA: ≥10 bpm for at least 10 seconds (<2 min)
After 32 wks GA: ≥15 bpm for at least 15 seconds (<2 min)
Prolonged: >2 min, <10 min
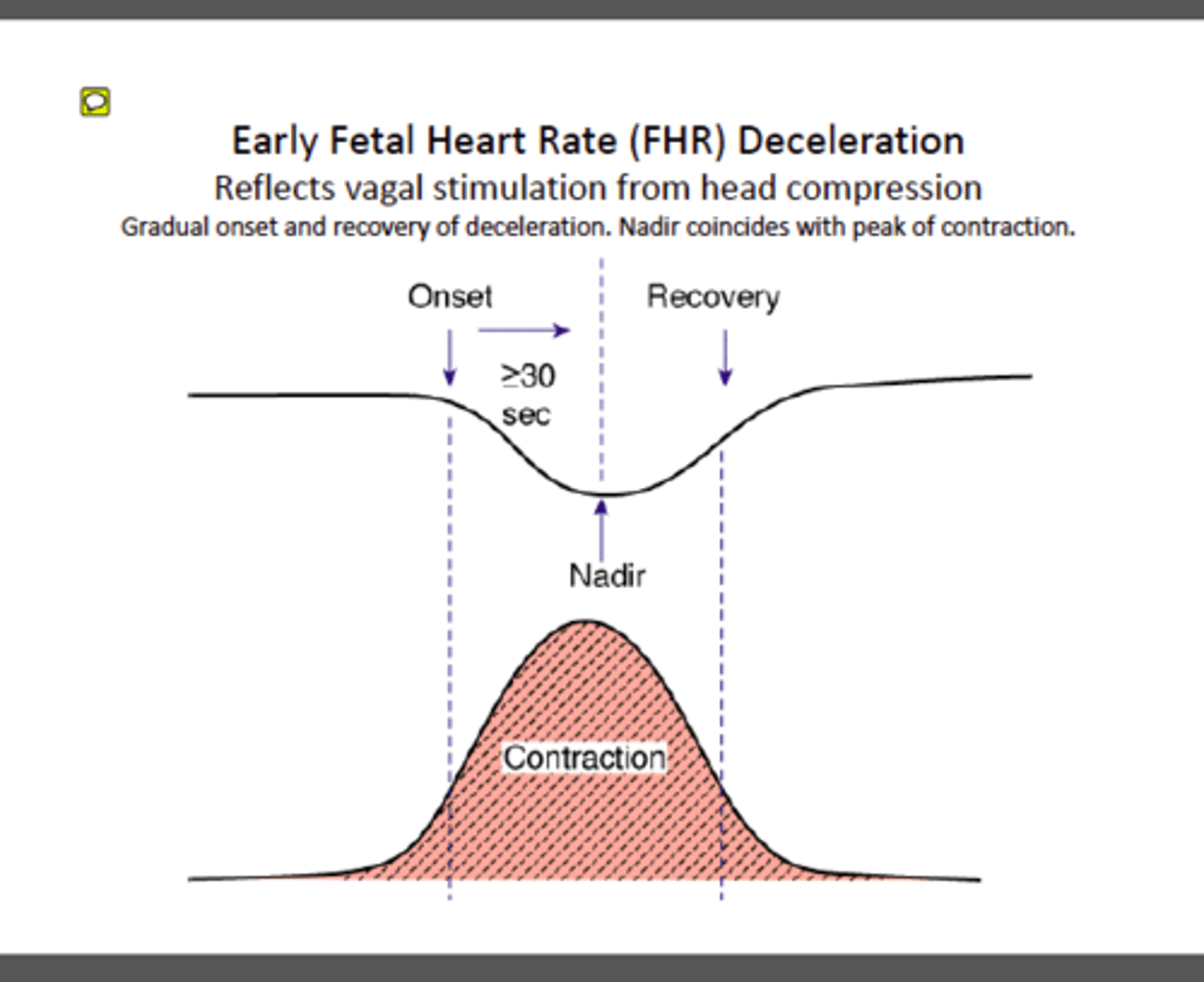
Early Decelerations
decel: benign, associated w/ head compression; start, nadir & end mirrors ctx
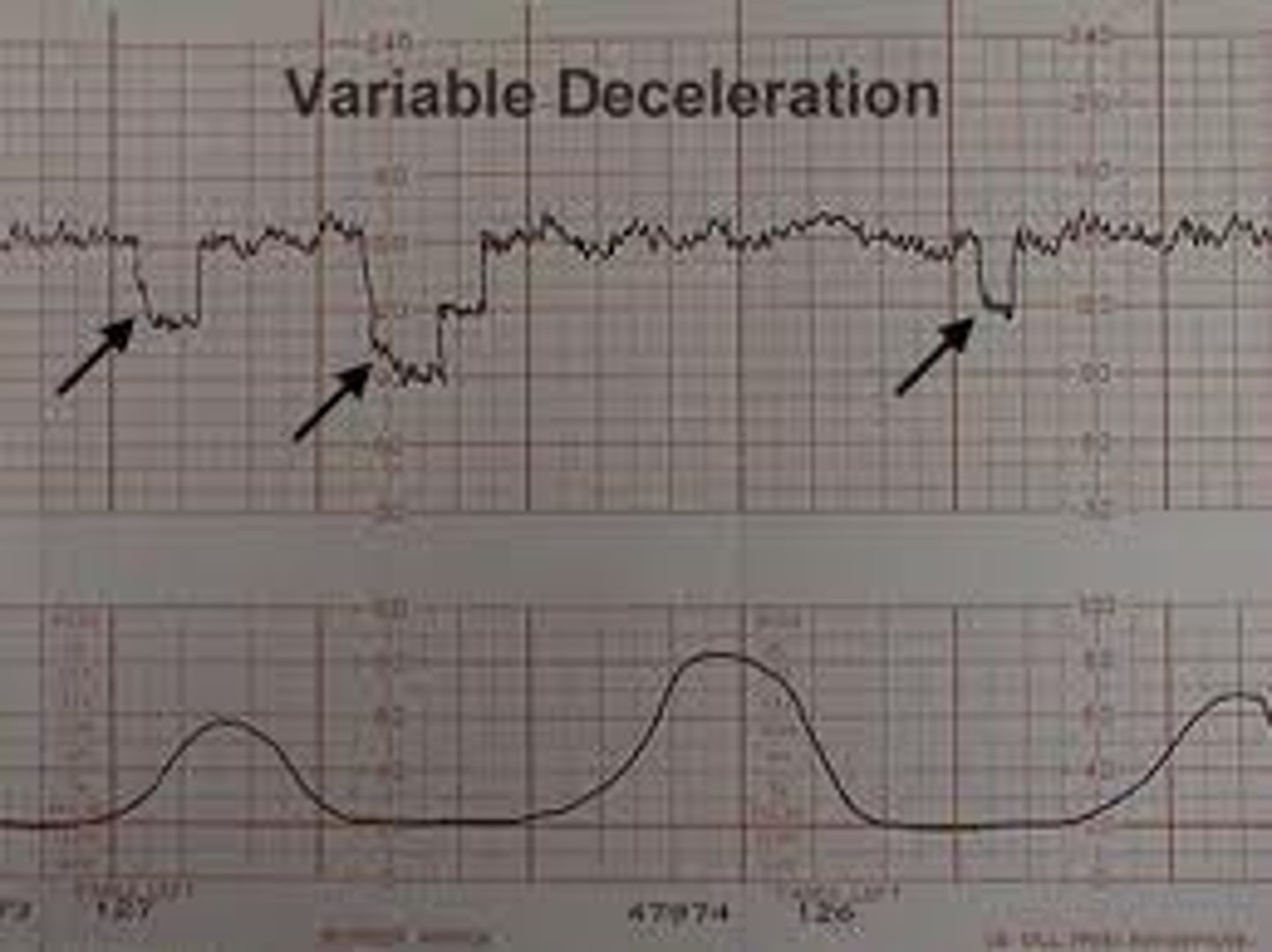
Variable decelerations
decel: abrupt drop to nadir in <30 sec; decrease of >15 bpm for 15 sec to 2 min; may/may not be linked to ctx; associated w/ cord compression
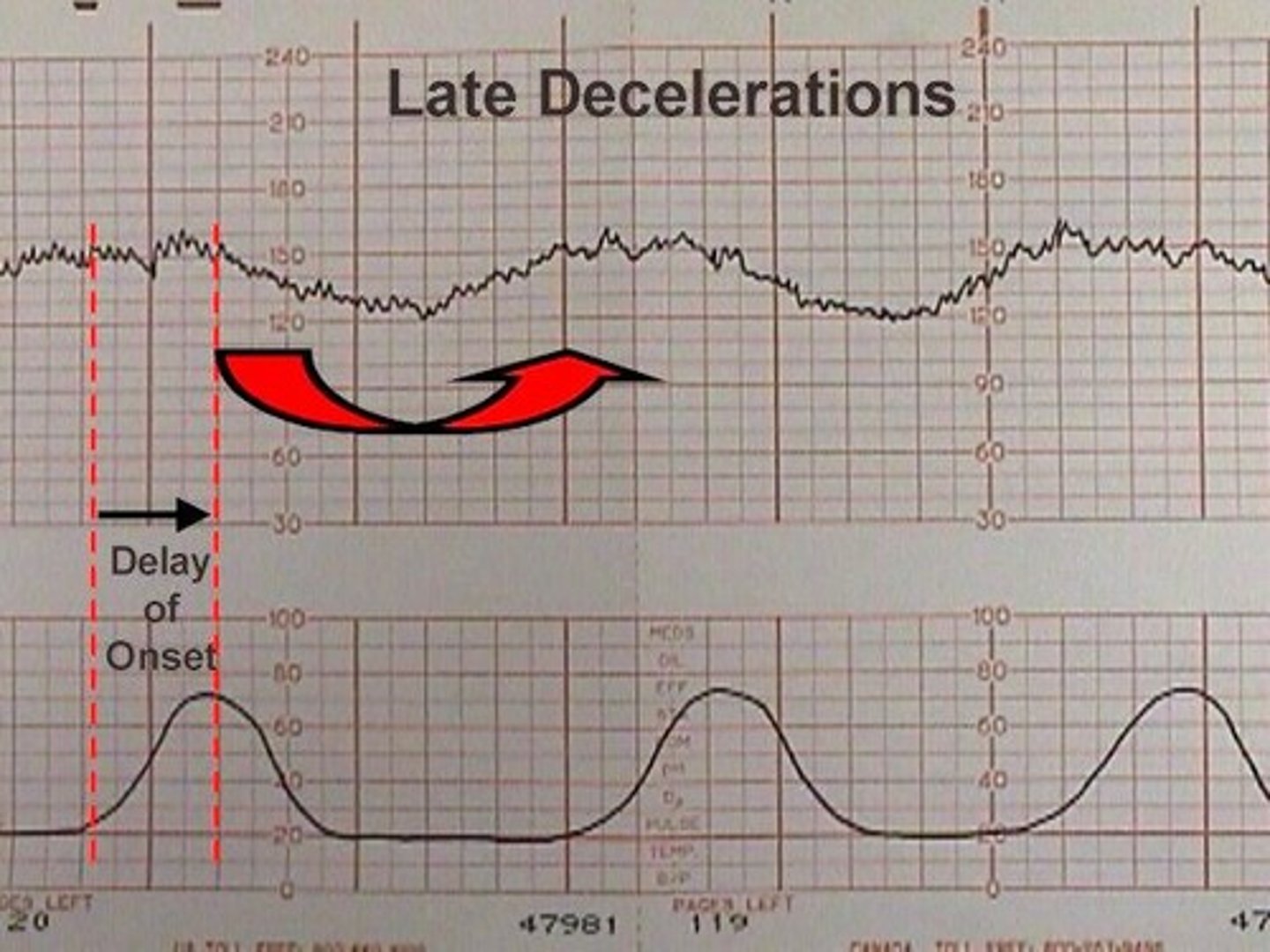
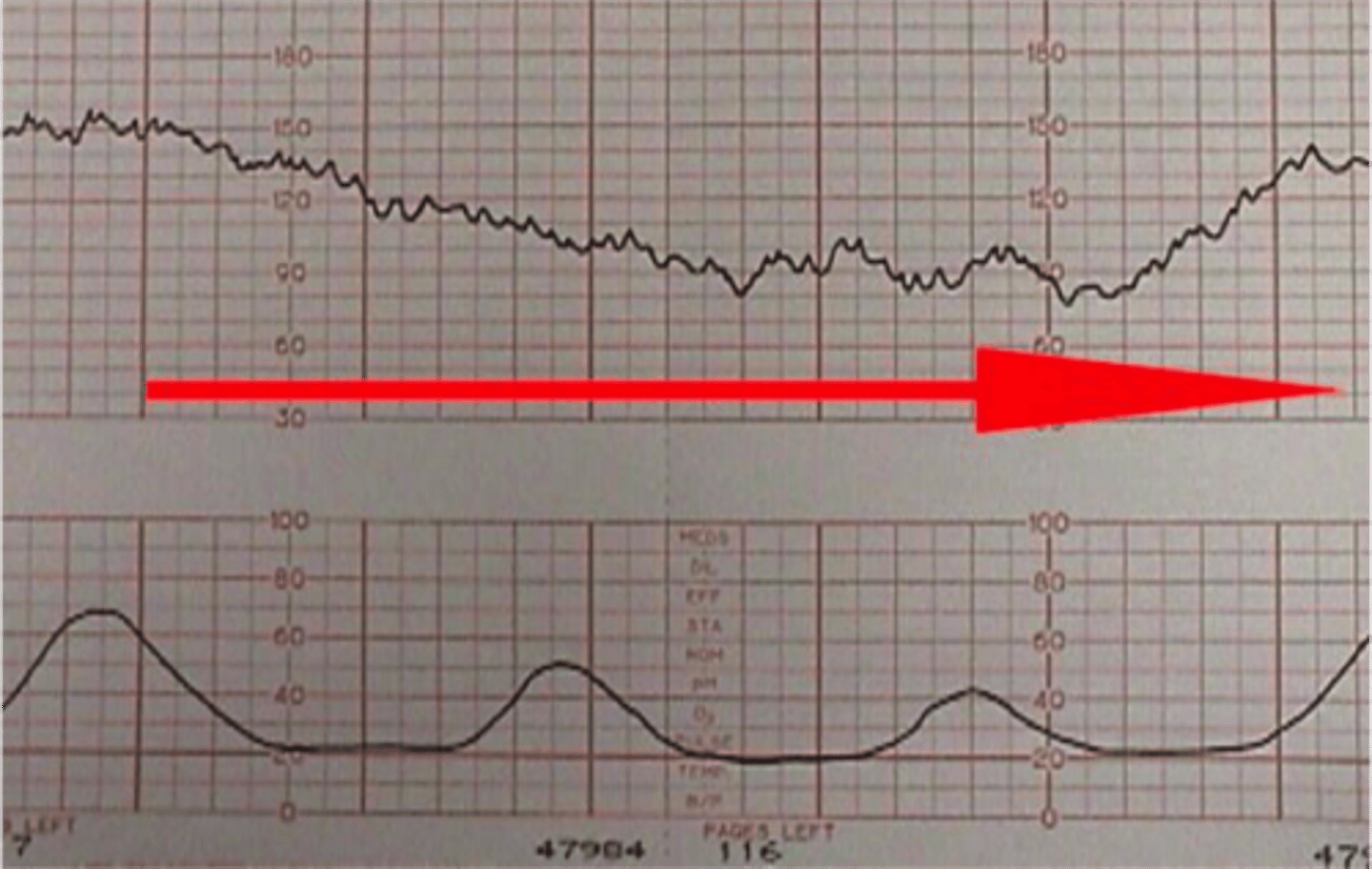
Late decelerations
decel: gradual onset >30 sec w/ nadir occurring after peak of ctx; associated w/ placental insufficiency
Prolonged deceleration
decel: decrease of >15 bpm lasting 2-10 min
Sinusoidal Pattern
Smooth wave-like pattern of regular frequency and amplitude
Rare & ominous FHR pattern - Category III
FHR Category I
Baseline FHR 110-160
Moderate variability
No late or variable decelerations
Early decelerations optional
Accelerations optional
FHR Category II
Everything that does not fit the criteria for Category I or III
*considered "indeterminate" - requires continued monitoring and re-evaluation
FHR Category III
Absent variability AND:
Recurrent late decelerations -or-
Recurrent variable decelerations -or-
Bradycardia
FHR Interpretation Mnemonic
VEAL CHOP
Variable
Early
Acceleration
Late
Cord compression
Head compression
Oxygenated well
Placental insufficency
Category II Interventions
POISON
Position change
Oxygen administration
Increased fluids
Sterile vaginal examination
Oxytocin off
Notify Provider
A. Findings are consistent with category I FHR tracing and requires
no interventions.
A continuous fetal monitoring strip is evaluated and found to have a baseline heart rate of 130, moderate variability, no accelerations or decelerations, and contractions every 3 minutes lasting 60 seconds each. How does the nurse interpret these findings?
A. Findings are consistent with category I FHR tracing and requires no interventions.
B. Findings are consistent with category II FHR tracing and requires no interventions.
C. Findings are consistent with category III FHR tracing and requires no interventions.
D. Findings are consistent with category III FHR tracing and requires intrauterine resuscitation measures.