Movement Lecture
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
65 Terms
Lower Motor Neurons
Neurons in spinal cord and brainstem that initiate skeletal muscle contraction
Final common pathway for transmitting info from many sources
Components of Lower Motor Neurons
Cell bodies located in the ventral horn of the spinal cord and in the motor nuclei of the cranial nerve of the brainstem
Sends axons directly to skeletal muscles
Spatial and temporal patterns of activation determined by local circuits
In Lower Motor Neurons which sensory neurons do local circuit neurons receive input from?
Sensory- Motor reflexes
Rhythmical and stereotyped behavior
Upper motor neurons
modulate the activity of lower motor neurons
Components of Upper motor neurons
Cell bodies located in brainstem centers
Vestibular nuclei, superior coliculus, reticular formation, also
the cerebral cortex; initiate and guide a wide variety of involuntary and voluntary movements
Neural Circuits function
responsible for the control of movement divided into 4 subsystems
4 subsytems of neural circuits
Local circuitry within the gray matter of the spinal cord and the tegmentum of the brainstem
Upper motor neurons with cell bodies in the brainstem or cortex
Cerebellum
Basal Ganglia
Local circuitry within the gray matter of the spinal cord and the tegmentum of the brainstem
• “final common path” for initiating movement
• Lower motor neurons and local circuit neurons
Upper motor neurons with cell bodies in the brainstem or cortex
Essential for the initiation of voluntary movements and for complex
spatiotemporal sequences of skilled movementsCortical areas in the frontal lobe (primary motor cortex) and
premotor cortex are essential for planning, initiating, and directing
sequences of voluntary movementBrain stem responsible for regulating muscle tone and orienting the
eyes, head, and body in response to sensory stimuli; posture
Cerebellum
regulates the activity of upper
neuronsDetects and attenuates the difference between an
intended movement and the movement actually
performed (motor error)Coordinated control
Basal Ganglia
suppress unwanted movements
and prepare upper motor neuron circuits for the
initiation of movementsParkinson’s and Huntington’s Disease
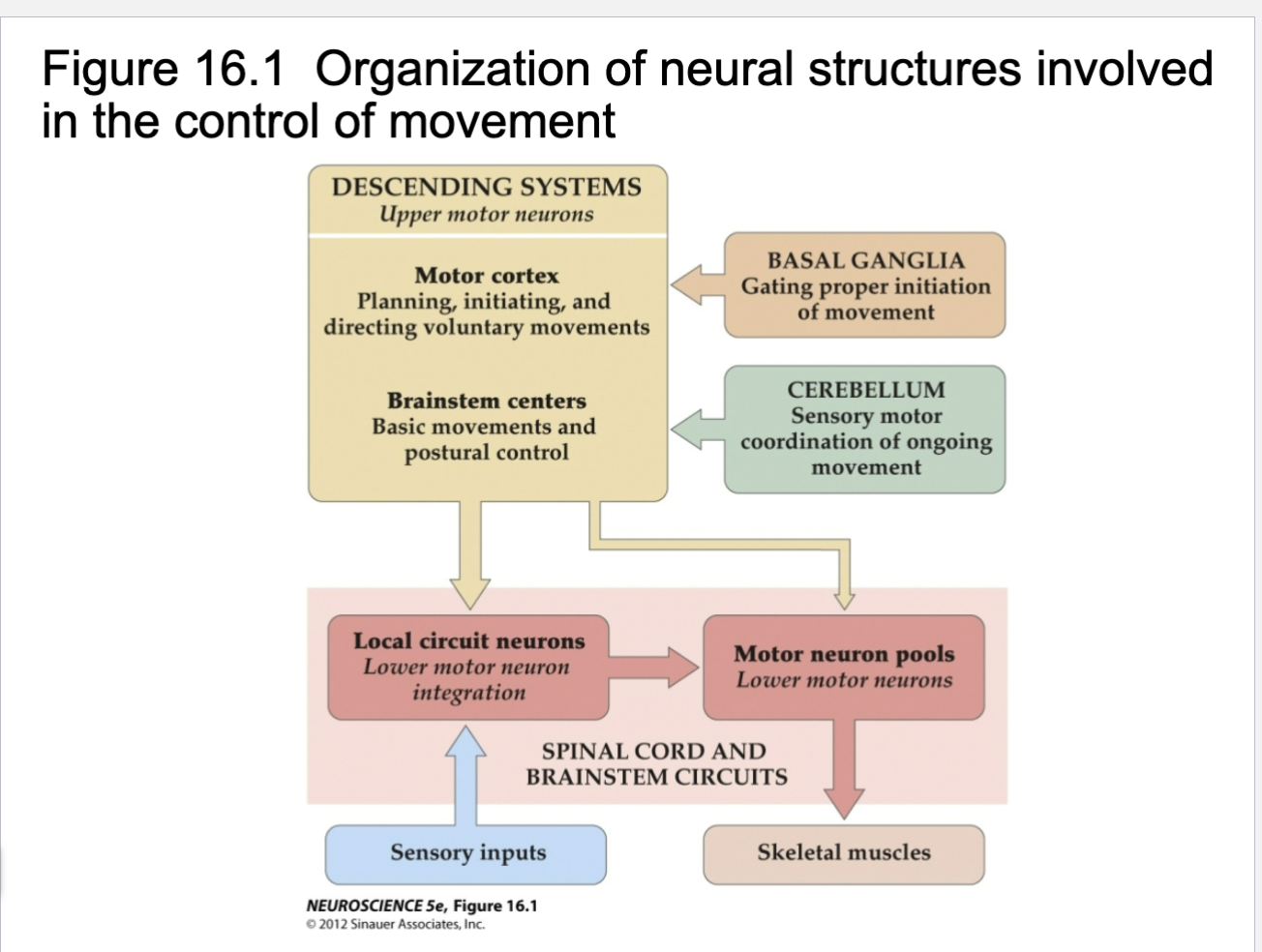
Figure 16.1
Motor cortex vs brainstem
Brainstem- Posture, orientation
Planning, voluntary movements
Lower motor neurons, cell body sits in spinal cord, axon extends out spinal cord through nerve, axon terminals of lower motor neuron goes to muscle fiber
Each muscle served by at least one motor nerve
Motor nerve contains axons of up to hundreds of motor neurons
Axons branch into terminals, each of which → NMJ with
single muscle fiber
Motor Unit
motor neuron and all (four to several hundred) muscle fibers it supplies
Smaller number = fine control
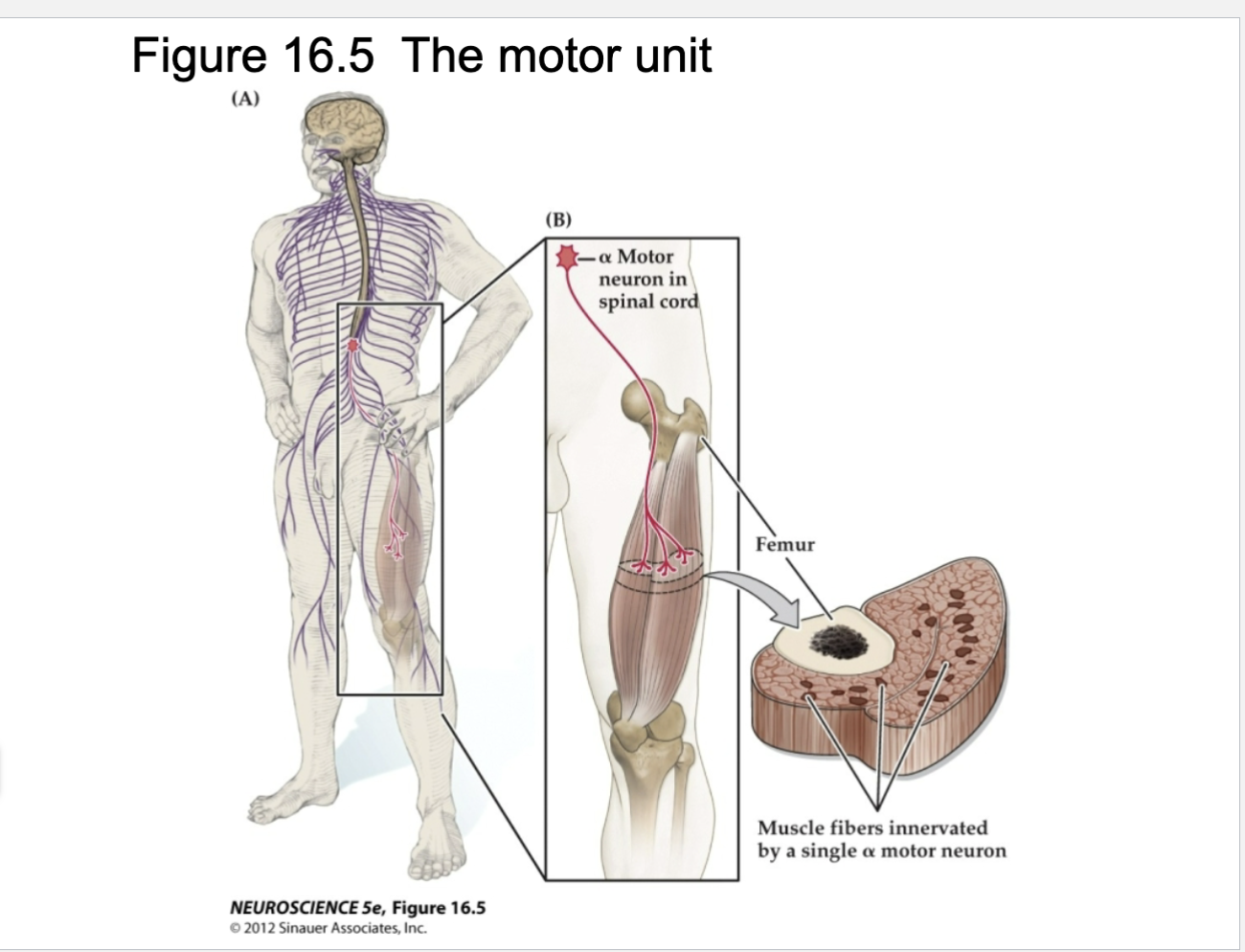
Explain Figure 16.5
Shows motor unit
Large motor neurons (alpha neurons); each neuron synapses with multiple fibers in each muscle.
The motor neuron and the muscle fibers it contacts = motor unit.
Notice the diffuse pattern of muscle fibers contacted by this single motor neuron.
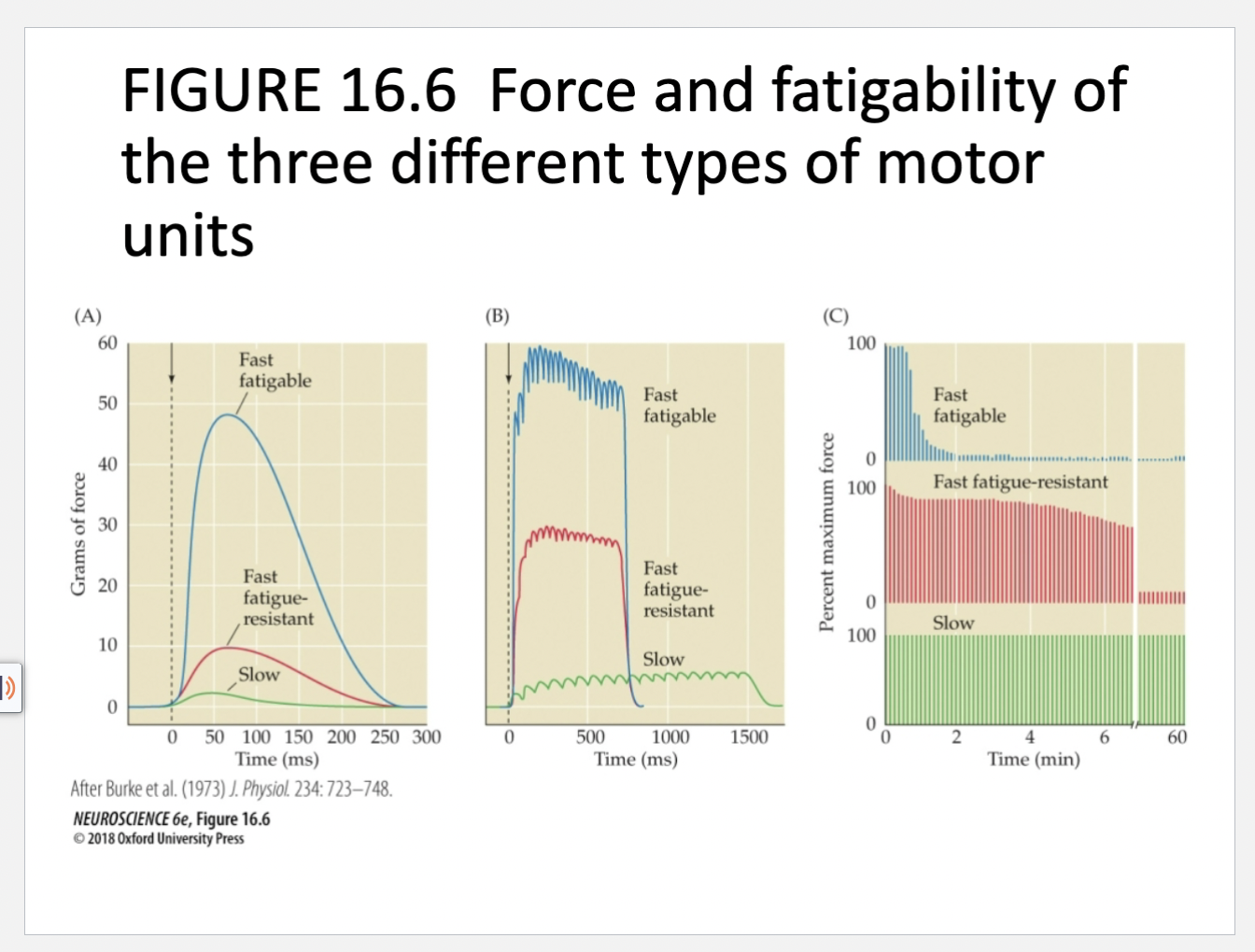
Figure 16.6- Force and fatigability of three different types of motor units diagram explanation
In each case, the response reflects stimulation of a single a motor neuron.
(A) Change in muscle tension in response to a single action potential.
(B) Tension in response to repetitive stimulation of each type of motor unit.
(C) Response to repeated stimulation at a level that initially evokes maximum tension. The ordinate represents the force generated by each stimulus. Note the different time scales in the three panels and the strikingly different tensions generated and fatigue rates among motor units.
Slow= Not alot of force, but persistent
Fast fatiguable= strong movements that quickly get out
Fast= Strong force that can be sustained a little longer
Three different types of motor units
Fast Fatigable
Fast fatigue-resistant
Slow
Fast Fatigable motor neuron
important for brief exertions that require large forces
Ex: Running or Jumping
Fast fatigue-resistant motor neuron
Strong intermediate exertions that can last longer than fast
Slow motor unit
Important for activities that require sustained muscular contraction
Ex: maintaining upright posture
Reflexes
Muscle stretch reflexes – “knee” jerk reflex
Flexion Reflex Pathways
Two types of neuron for reflexes
small gamma motor neurons
Alpha motor neurons
Small gamma motor neurons in Reflexes
innervate specialized muscle fibers called muscle spindles; intrafusal muscle fibers
Regulate the length of the muscle fibers using sensory information provided by sensory receptors in the intrafusal muscle fibers
Alpha motor neurons in Reflexes
Innervate the extrafusal muscle fibers; striated muscle
Actually generate forces for posture and movement
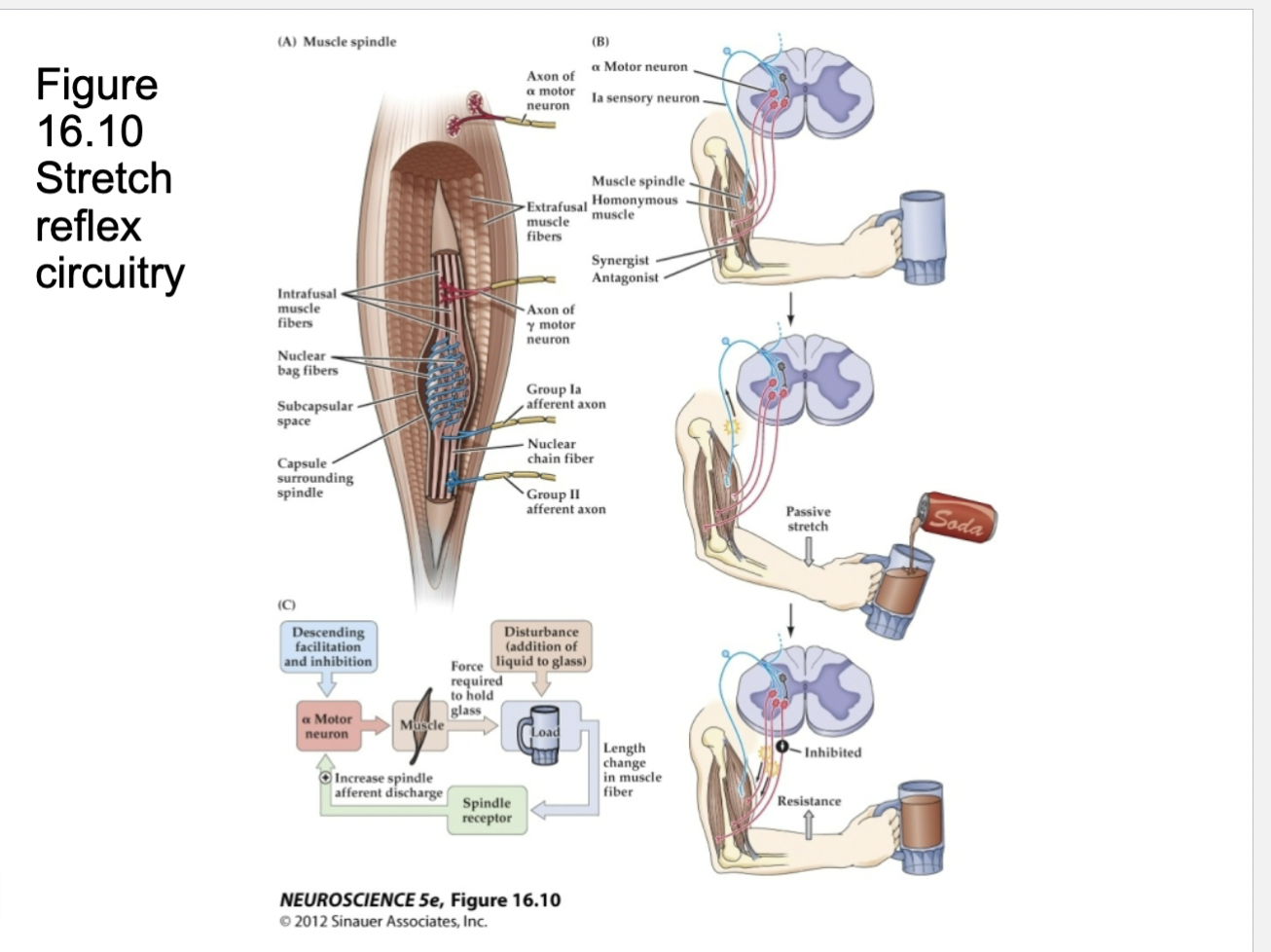
Figure 16.10- Reflexes
(A) Diagram of a muscle spindle, the sensory receptor that initiates the stretch reflex.
(B) Stretching a muscle spindle leads to increased activity in group Ia afferents and an increase in the activity of a motor neurons that innervate the same muscle. Group Ia afferents also excite the motor neurons that innervate synergistic muscles, and they indirectly inhibit the motor neurons that innervate antagonists via intervening reciprocal-Ia-inhibitory interneurons (gray neurons; see also Figures 1.7–1.9).
(C) The stretch reflex operates as a negative feedback loop to regulate muscle length.
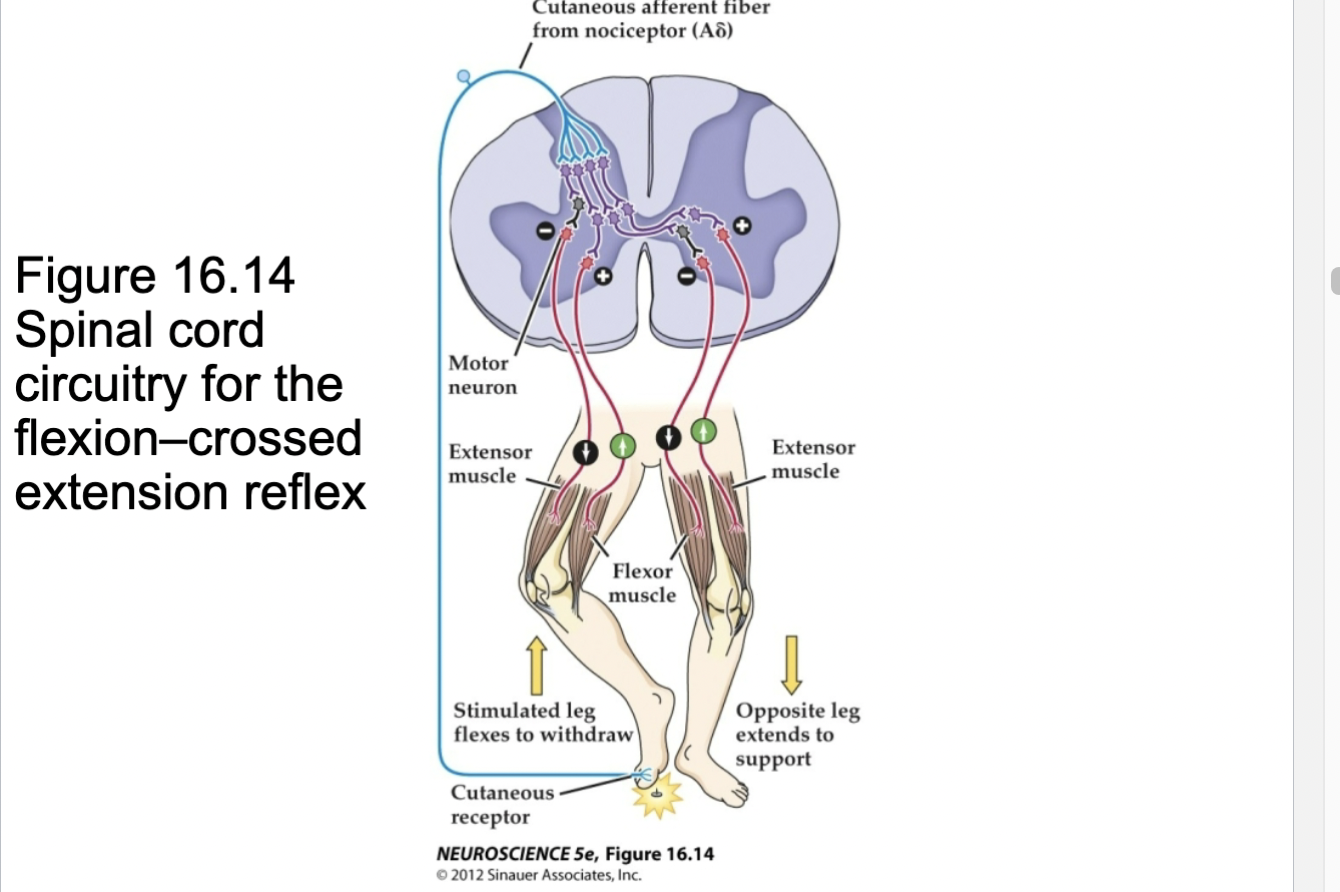
Figure 16.14- Spinal Cord circuitry for the flexion-crossed extension reflex
Stimulation of cutaneous receptors in the foot (by stepping on a tack, in this example) leads to activation of spinal cord local circuits that serve to withdraw (flex) the stimulated extremity and extend the other extremity to provide compensatory support.
Other leg also involved for balance
Pain receptors (nociceptors) activate
Spinal Cord circuitry and locomotion- Central Pattern Generators
capable of controlling the timing and coordination of complex patterns of movement
Rhythmic patterns of limb movement during locomotion are not dependent on sensory input or input from higher centers
Figure 16.5- The mammalian cycle of locomotion is organized by central pattern generators in the spinal cord
The locomotion cycle is shown here for a cat.
Electrode detect when certain muscles are contracted or not
swing vs stance phase
During swing phase flexors muscles activated and extensor muscles relaxed
During stance phase extensor muscles activated and flexor muscles relaxed
After transection of spinal cord cat is still able to activate extensor and flexor in coordinated pattern and able to walk without higher order brain functions, only requires local circuits
Lower motor neurons and muscle cells
Damage to lower neuron cell bodies or peripheral
axons
• paralysis or paresis
• Loss of reflexes (areflexia)
• Loss of muscle tone
• Atrophy due to denervation and disuse
• Fibrillations – due to changes in the excitability of denervated muscle fibers
• Fasciculations – abnormal activity of injured motor neurons
• Fibrillations and fasciculations – clinical tool for diagnosis of lower motor neuron disorders
• ALS – Amyotrophic Lateral Sclerosis
Amyotrophic Lateral Sclerosis (ALS)
Neurodegenerative disease that affects about .05%
of the population in the U.S.
• Slow degeneration of motor neurons in the ventral
horn of the spinal cord and brain stem (lower
motor neurons) and neurons in the motor cortex
(upper motor neurons)
• Progressive weakness and wasting of the skeletal
muscles
• Intellect remains intact
Upper motor neurons Function
Influence the generation of movements by modulating the activity of local circuits in the brainstem and spinal cord
Sources of upper motor neuron pathways
Brain stem center
Cortical Area
2 sources of upper motor neuron pathways
Brain Stem Centers
Coritcal Areas
Brain Stem Centers upper motor neuron pathway function
Postural control, orientation toward sensory stimuli,
locomotion
Cortical areas upper motor neuron pathway function
Planning and precise control of complex sequences of voluntary movements
Somatic expression of emotional states
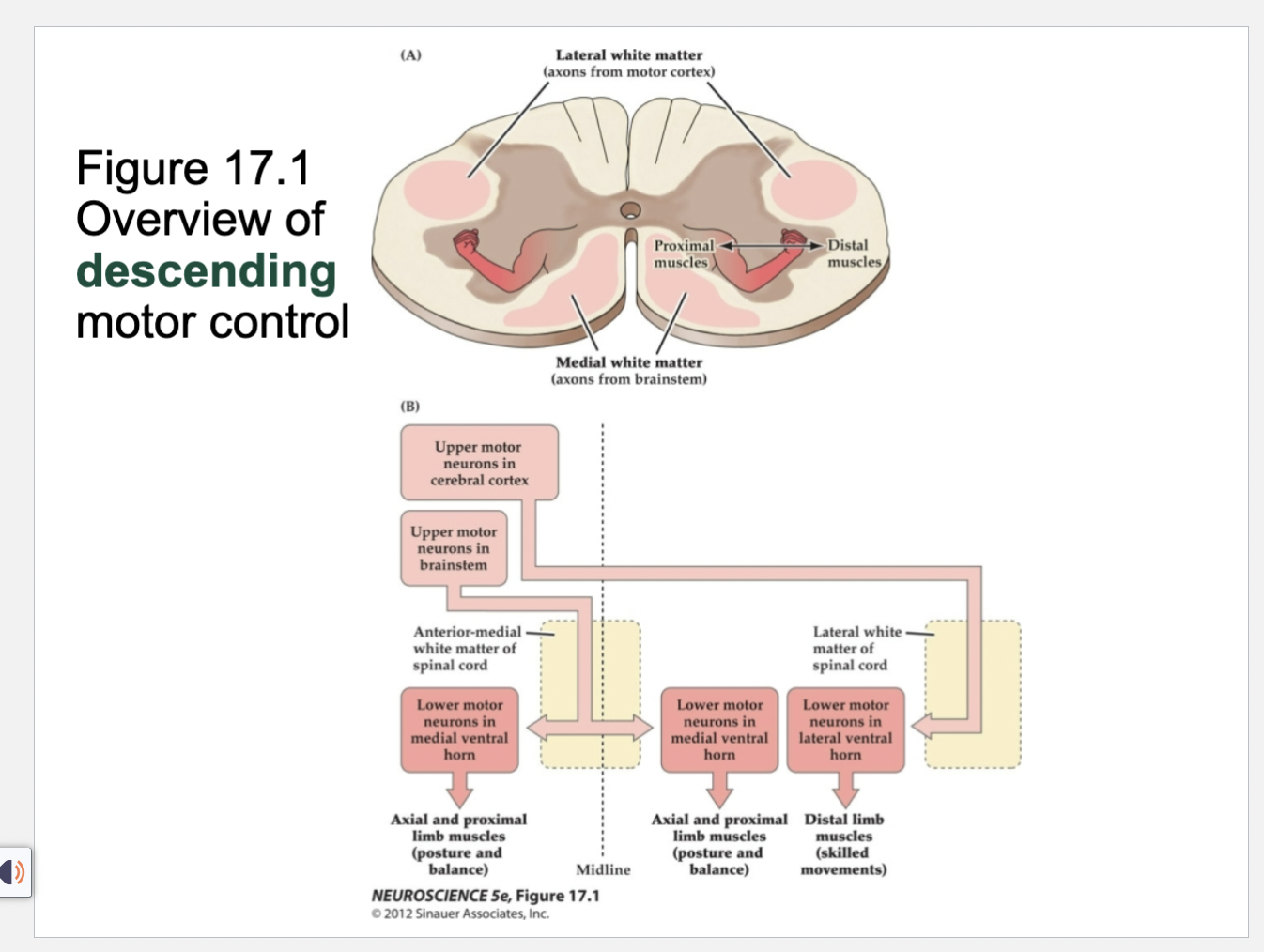
Figure 17.1- Overview of descending motor control
(A) Somatotopic organization of the ventral horn in the cervical enlargement. The locations of descending projections from the motor cortex in the lateral white matter and from the brainstem in the anterior-medial white matter are shown.
(B) Schematic illustration of the major pathways for descending motor control. The medial ventral horn contains lower motor neurons that govern posture, balance, locomotion, and orienting movements of the head and neck during shifts of visual gaze. These medial motor neurons receive descending input from pathways that originate mainly in the brainstem, course through the anterior-medial white matter of the spinal cord, and then terminate bilaterally. The lateral ventral horn contains lower motor neurons that mediate the expression of skilled voluntary movements of the distal extremities. These lateral motor neurons receive a major descending projection from the contralateral motor cortex via the main (lateral) division of the corticospinal tract, which runs in the lateral white matter of the spinal cord. For simplicity, only one side of the brainstem, motor cortex, and lateral ventral horn is shown, and the minor anterior corticospinal tract is not illustrated
2 components of Descending Motor Control
Medial Ventral Horn
Lateral Ventral Horn
Medial Ventral Horn
Posture
Balance
Orienting movements of the head and neck during shifts of visual gaze
Receive descending input from pathways that originate in the brainstem
Lateral Ventral Horn
• Expression of skilled voluntary movements of the distal
extremities
• Receive descending input from motor cortex (corticospinal
tract)
Premotor Cortex
• Receives extensive multi sensory input and more
complex signals related to motivation and intention
from the prefrontal cortex
• Experiments indicate that the premotor cortex uses
information from other cortical regions to select
movements appropriate to the context of the
action
• Selection of movements based on external events
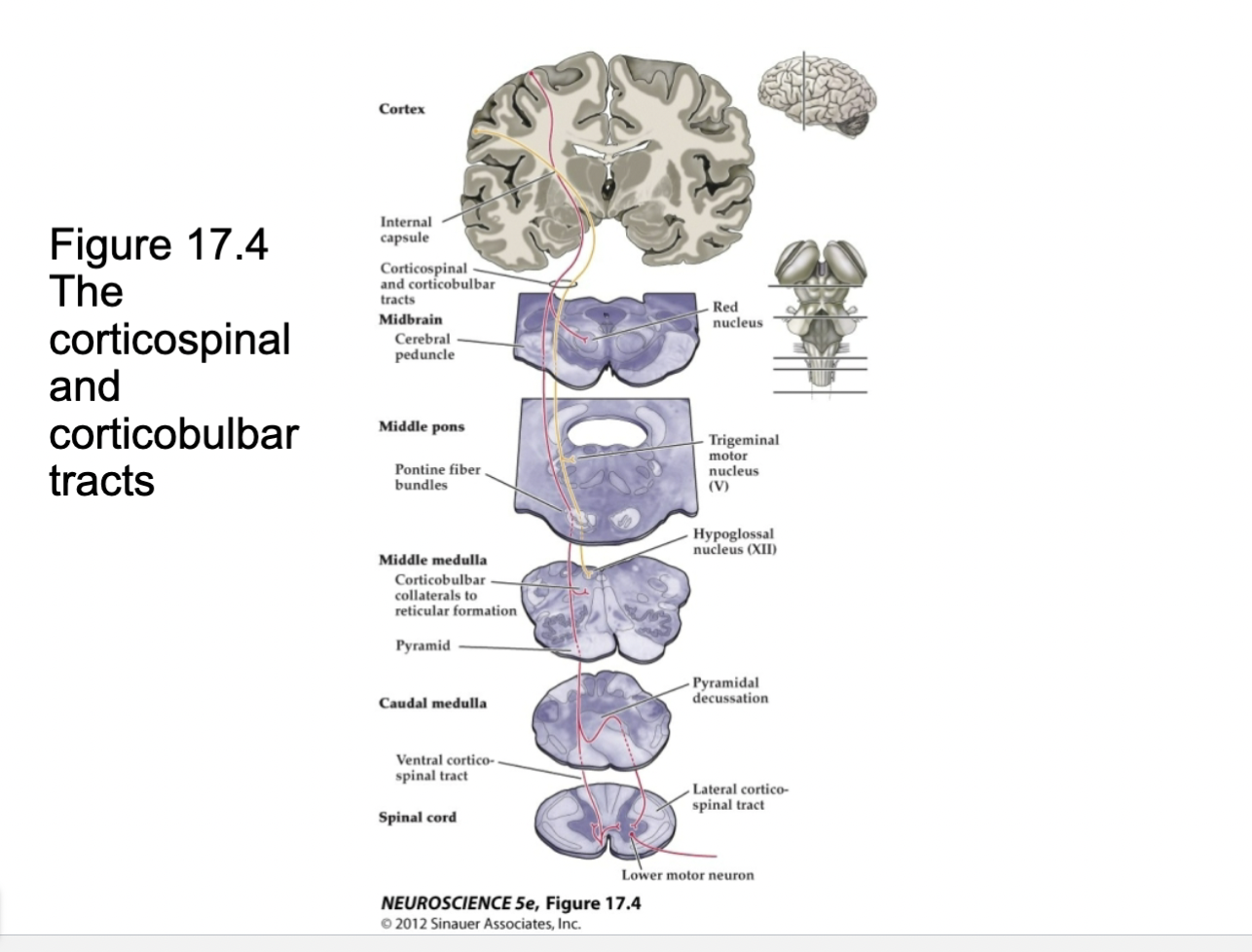
Corticospinal and Corticobulbar tracts
Coritcalbulbar in yellow innerveates brain stem nuclei, psoture, etc
Neurons in the motor cortex give rise to axons that travel through the internal capsule and coalesce on the ventral surface of the midbrain, within the cerebral peduncle. These axons continue through the pons and come to lie on the ventral surface of the medulla, giving rise to the medullary pyramids. As they course through the brainstem, corticobulbar axons (gold) give rise to bilateral collaterals that innervate brainstem nuclei (only collaterals to the trigeminal motor nuclei and the hypoglossal nuclei are shown). Most of the corticospinal fibers (dark red) cross in the caudal part of the medulla to form the lateral corticospinal tract in the spinal cord. Those axons that do not cross (light red) form the ventral corticospinal tract, which terminates bilaterally.
Motor Control Centers of the Brainstem Function
Maintain balance, govern posture, and orient gaze
3 components of Brainstem
Vestibular Complex
Reticular Formation
Superior Colliculus
Vestibular complex
regulates head position; balance
Reticular formation
scattered clusters of neurons; difficult
to subdivide anatomically
• Variety of functions – coordination of eye movements,
cardiovascular and respiratory control, regulation of sleep and
wakefulness
• temporal and spatial coordination of limb and trunk movements
Superior colliculus
output mediated through the reticular formation
Controlling axial musculature in the neck
Generating orienting movements of the head
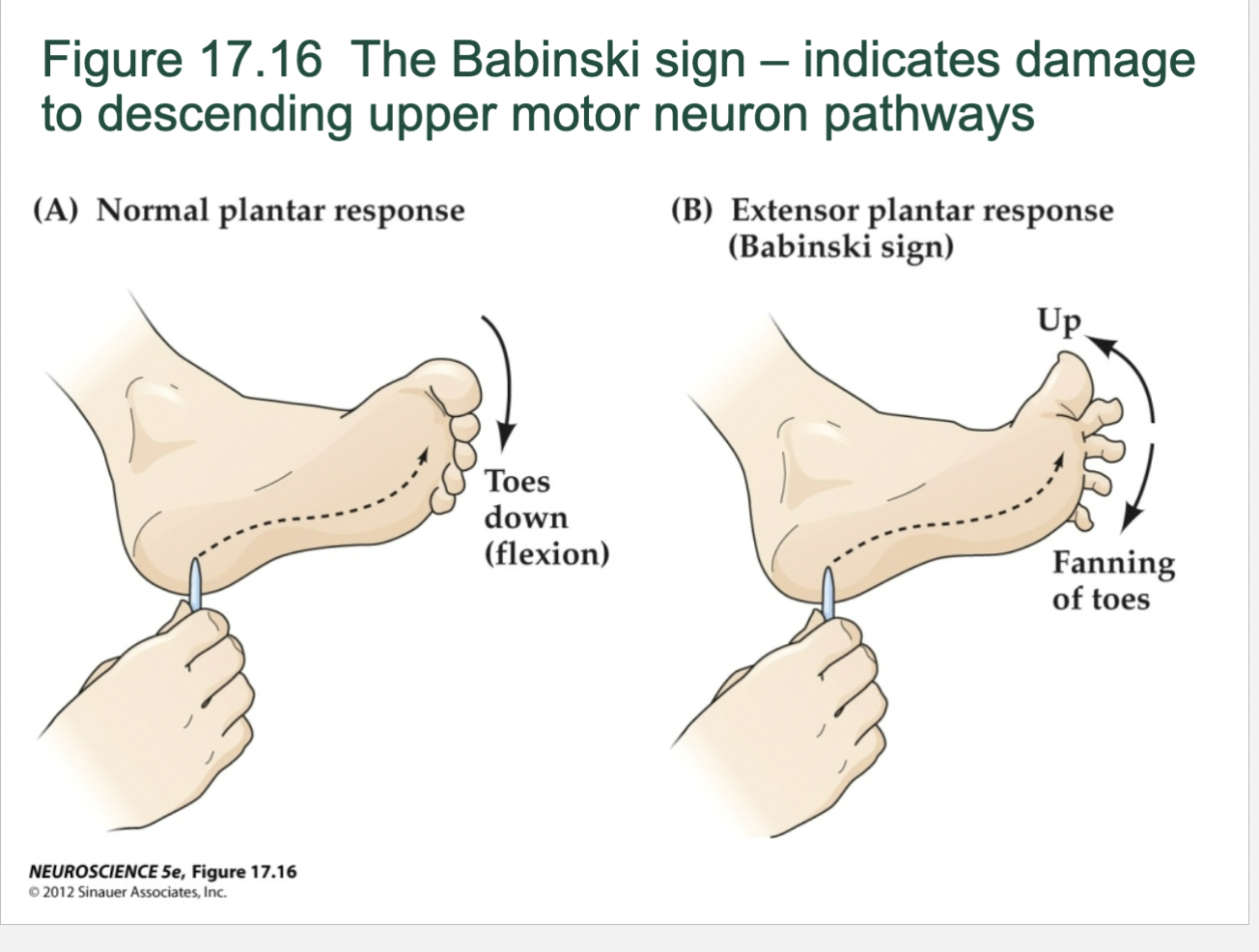
Babinski Sign
A typical fanning of the toes -- caused by damage to descending corticospinal pathways
FIGURE 17.17 The Babinski sign. Following damage to descending corticospinal pathways, stroking the sole of the foot may cause an atypical fanning of the toes and the extension of the big toe.
Indicates issues in upper motor neurons (Corticospinal and Corticobulbar tracts)
Normal response toes curl down
Abnormal response is fanning
Modulation of movement by the basal ganglia
Do not project directly to local circuit or lower motor neurons
• Regulate the activity of upper motor neurons
• Large, functionally diverse set of nuclei
• Motor function
• Caudate
• Putamen (together form the corpus striatum)
• Globus pallidus
• Substantia nigra
• Subthalamic nucleus
All of the structures above form a subcortical loop that links most areas
of the cortex with upper motor neurons in the primary and premotor
cortices and brainstem
• Influences of these structures on upper motor neurons are required for
the normal performance of voluntary movements
• When one of these components is compromised, the motor systems
cannot switch smoothly between commands that initiate and maintain
movement and those that terminate movement
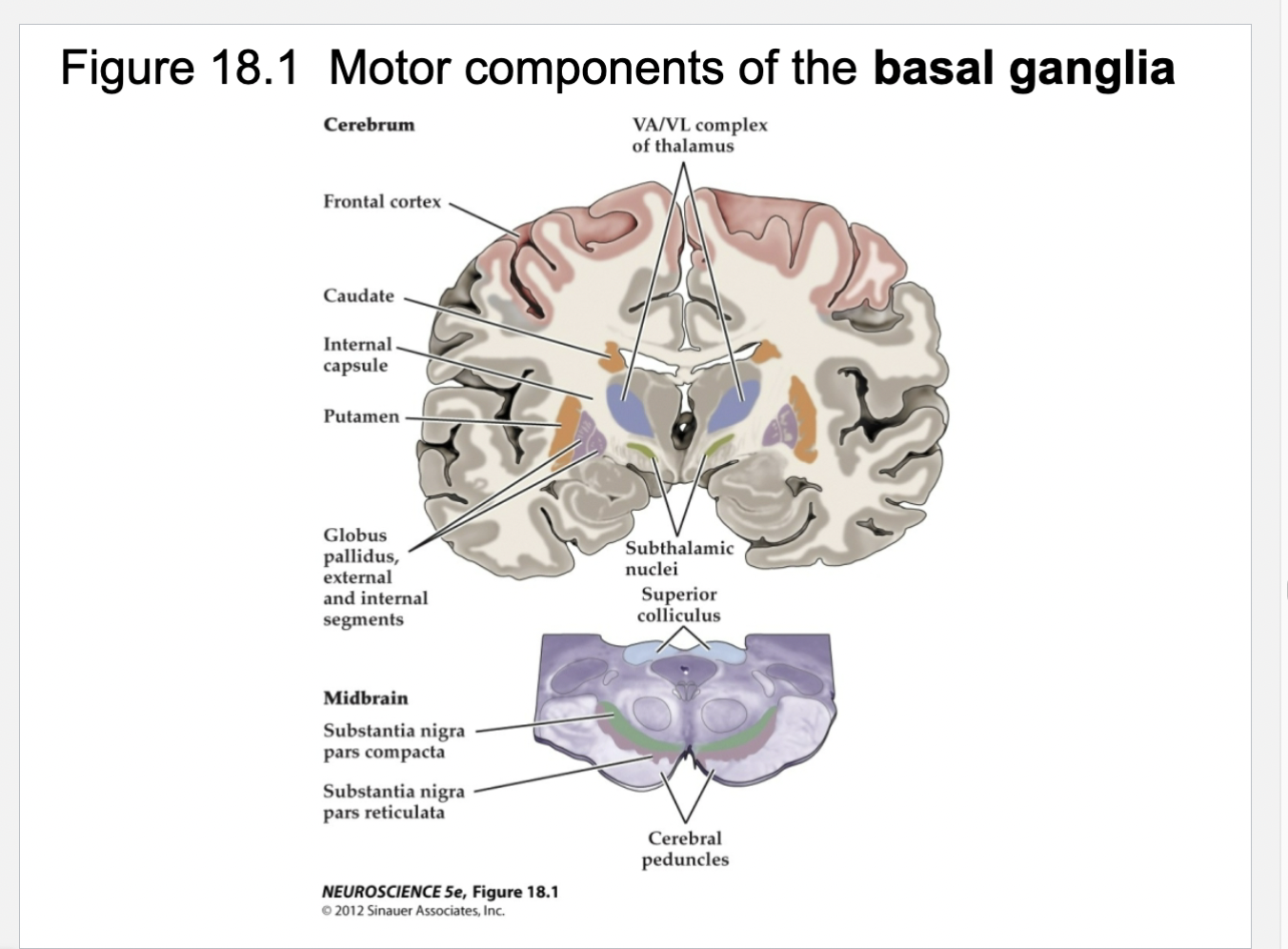
Figure 18.1- Motor components of basal ganglia
Basal ganglia regulate upper motor neuron circuits
The human basal ganglia comprise a set of gray matter structures, most of which are buried deep in the telencephalon, although some are found in the diencephalon and midbrain. The major components that receive and process movement-related signals are the striatum (caudate and putamen) and the pallidum (globus pallidus and substantia nigra pars reticulata). These structures border the internal capsule in the forebrain and midbrain (the cerebral peduncle is a caudal extension of the internal capsule). Smaller but functionally significant components of the basal ganglia system are the substantia nigra pars compacta and the subthalamic nucleus, which provide input to the striatum and pallidum, respectively. For the control of limb movements, output from the basal ganglia arises in the internal segment of the globus pallidus and is sent to the ventral anterior and ventral lateral nuclei (VA/VL complex) of the thalamus, which interact directly with circuits of upper motor neurons in frontal cortex. The substantia nigra pars reticulata projects to upper motor neurons in the superior colliculus and controls orienting movements of the eyes and head.
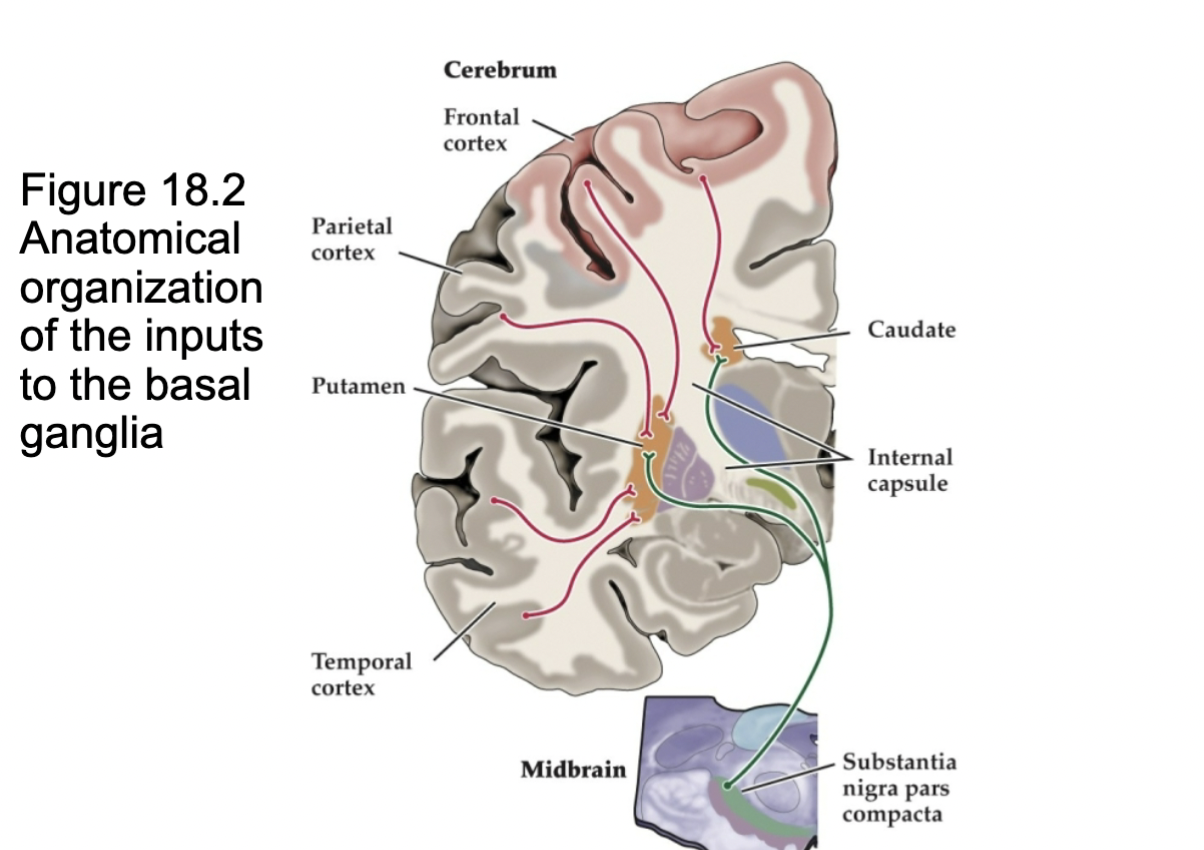
Figure 18.2- Anatomical Organization of input to basal ganglia
Idealized coronal sections through the human forebrain and midbrain, showing the projections from the cerebral cortex and substantia nigra pars compacta to the caudate and putamen.
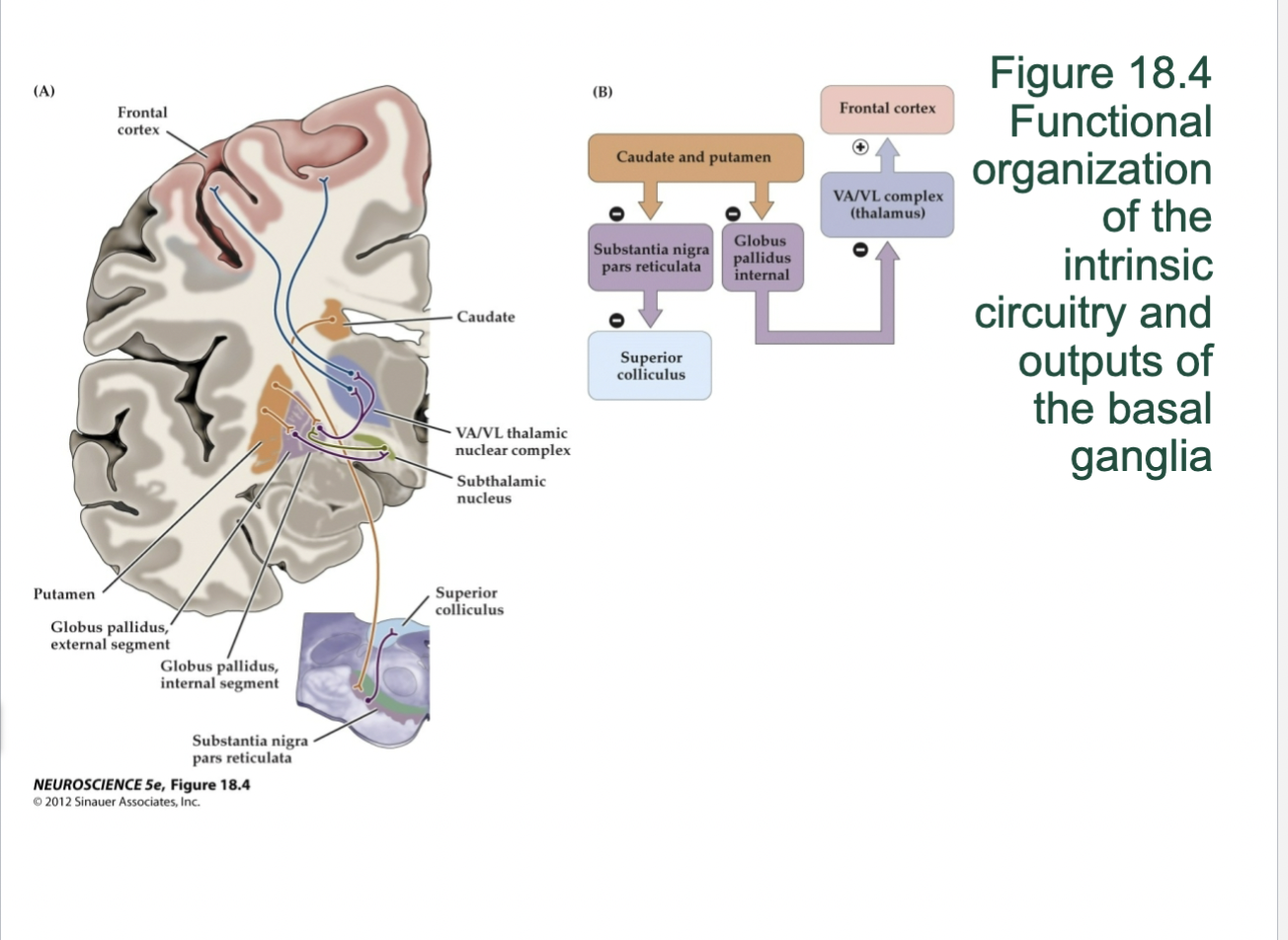
18.4- Functional organization of the intrinsic circuitry and outputs of basal ganglia
(A) Idealized coronal sections through the human forebrain and midbrain, showing the intrinsic connections and output projections of the basal ganglia.
(B) Schematic diagram of the projections illustrated in
(A); the plus and minus signs indicate excitatory and inhibitory projections, respectively
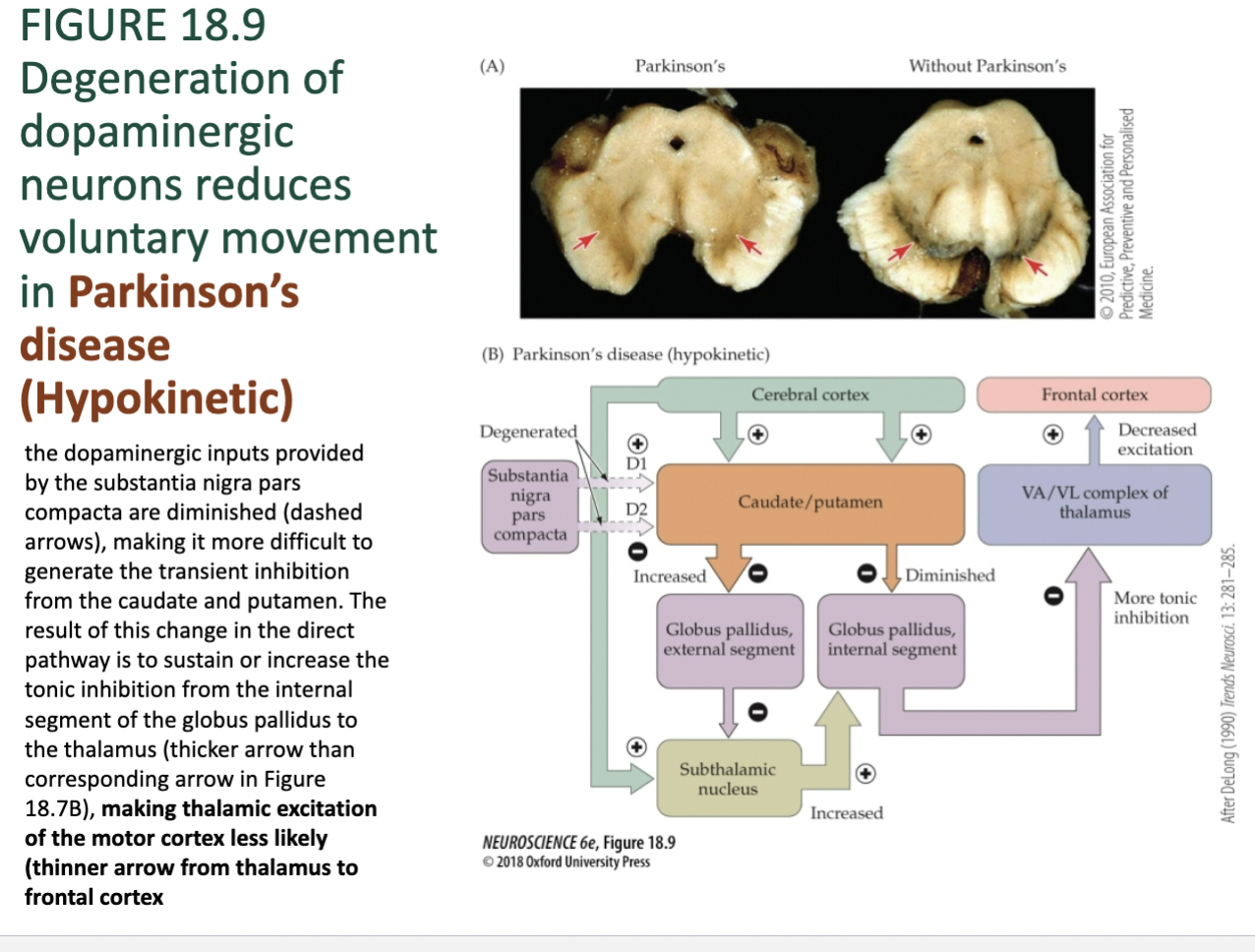
Figure 18.9- Neuropathology of Basal Ganglia – Parkinson’s
Parkinson’s disease (Hypokinetic) the dopaminergic inputs provided by the substantia nigra pars compacta are diminished (dashed arrows), making it more difficult to generate the transient inhibition from the caudate and putamen. The result of this change in the direct pathway is to sustain or increase the tonic inhibition from the internal segment of the globus pallidus to the thalamus (thicker arrow than corresponding arrow in Figure 18.7B), making thalamic excitation of the motor cortex less likely (thinner arrow from thalamus to frontal cortex
Parkinson’s Disease – pathology,
Dopamenergic neurons in sub. nigra are degenerated, lose imput of circuitry
Accumulation of lewy bodies
Parkinson’s Disease – causes
Proteolytic stress
• Accumulation and aggregation of abnormal proteins
• Lewy bodies – accumulation of alpha-synuclein
• Neurons particularly vulnerable
• Oxidative stress
• Generation of reactive oxygen species (ROS)
• Depletion of glutathione (anti-oxidant) and increase in iron (promotes
formation of ROS) in diseased brains
• Mitochondrial dysfunction
• Decreased mitochondrial complex activity (by 30–40%)
• Inflammation
• Overactivation of microglia
• Excess production of neurotoxic factors
Parkinson’s Disease – Symptoms
Clinical manifestations
• Insidious onset – gradual subtle way
• Motor features
• Tremor
• “Pill-rolling” resting tremor of hand
• Tremor of lips, chin, jaw, tongue, legs
• Rigidity from increased muscle stiffness and tone
• Bradykinesia – slowness of movement
• Postural instability
Parkinson’s Disease affects what?
Main area of the brain
affected is the
substantia nigra
• Loss of dopamine
neurons in this area
• Substantia nigra
• Part of the basal ganglia in
the midbrain
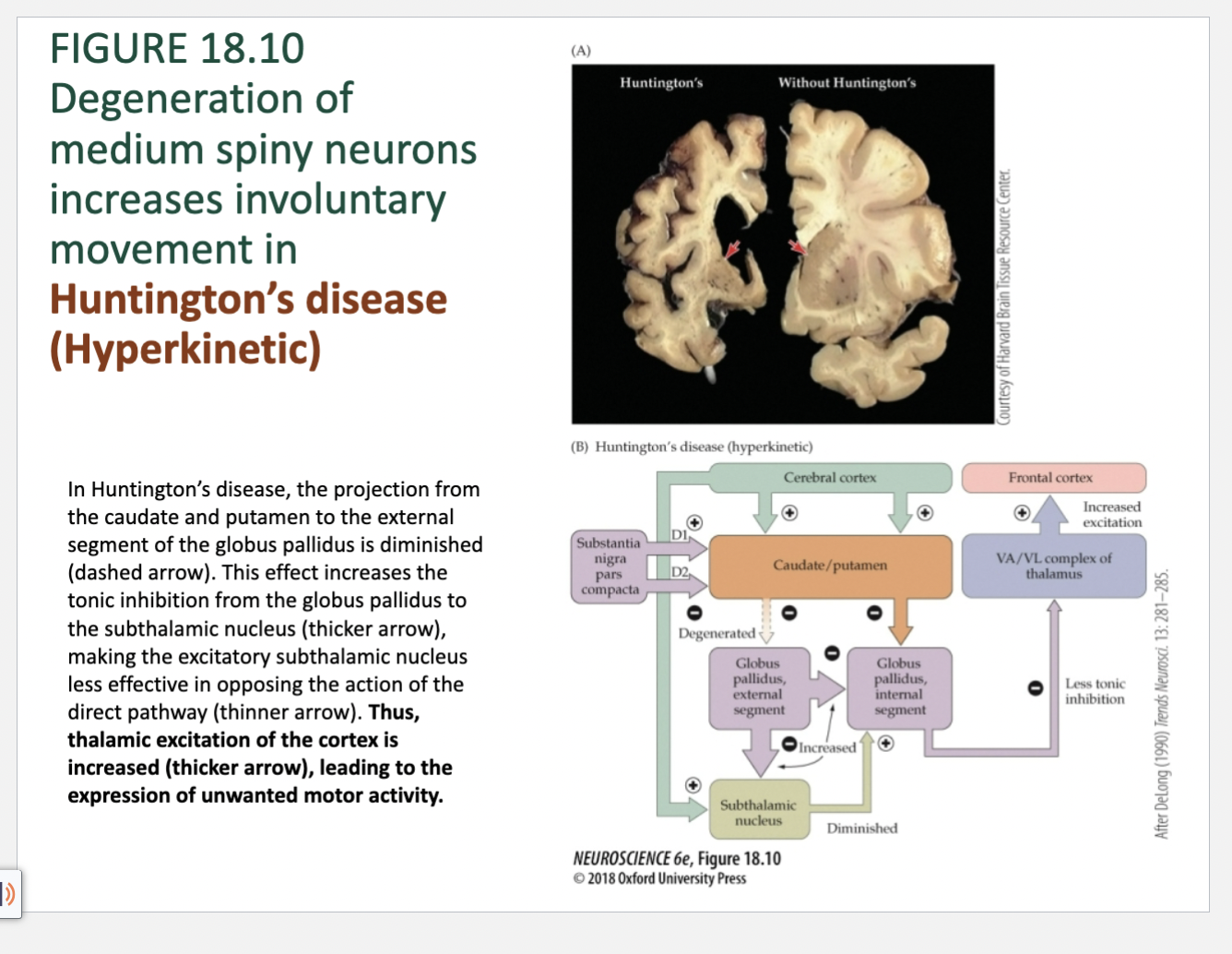
Figure 18.10- Neuropathology of Basal Ganglia – Huntington’s
In Huntington’s disease, the projection from
the caudate and putamen to the external
segment of the globus pallidus is diminished
(dashed arrow). This effect increases the
tonic inhibition from the globus pallidus to
the subthalamic nucleus (thicker arrow),
making the excitatory subthalamic nucleus
less effective in opposing the action of the
direct pathway (thinner arrow). Thus,
thalamic excitation of the cortex is
increased (thicker arrow), leading to the
expression of unwanted motor activity.
Huntington’s Disease – pathology,
Gross atrophy in caudate nucleus and putamen
accompanied by selective neuronal loss and
gliosis
• Neuronal loss in cerebral cortex
• Varying degrees of atrophy in other areas in
midbrain and cerebellum
• Shrinkage of brain (in volume)
• Numerous biochemical defects
Huntington’s Disease – causes
Etiology and pathogenesis
• Mutation in huntington gene (HTT) on short arm of chromosome 4
• HTT gene encodes for protein called huntingtin
• CAG segment is repeated 36–120 times
• Leads to huntingtin accumulation and formation of
inclusion in nucleus
• Alters transcription and transport; leads to neuronal cell
death
• Excitotoxicity, oxidative stress, impaired metabolism,
apoptosis
• Autosomal dominant pattern of inheritance
• Age of onset = 30-40
Huntington’s Disease – Symptoms
Involuntary movements
• Chorea – abnormal involuntary movement
disorder
• Parkinsonian features
• Akinetic–rigid syndrome
• Dysarthria – slowed or slurred speech
• Dysphagia – difficulty swallowing
• Abnormal eye movements
• Tics
• Myoclonus – quick involuntary muscle jerk
Huntington’s Diagnosis/ Treatment
Diagnosis
• Genetically proven family history
• Clinical presentation
• MRI or CT scan measure brain atrophy
• Referral to neurologist who specializes in HD
• Treatment
• Reduce symptoms and improve quality of life
• Tetrabenazine for chorea
• Antidepressant or antipsychotic medications
• Levodopa or dopamine agonist medications
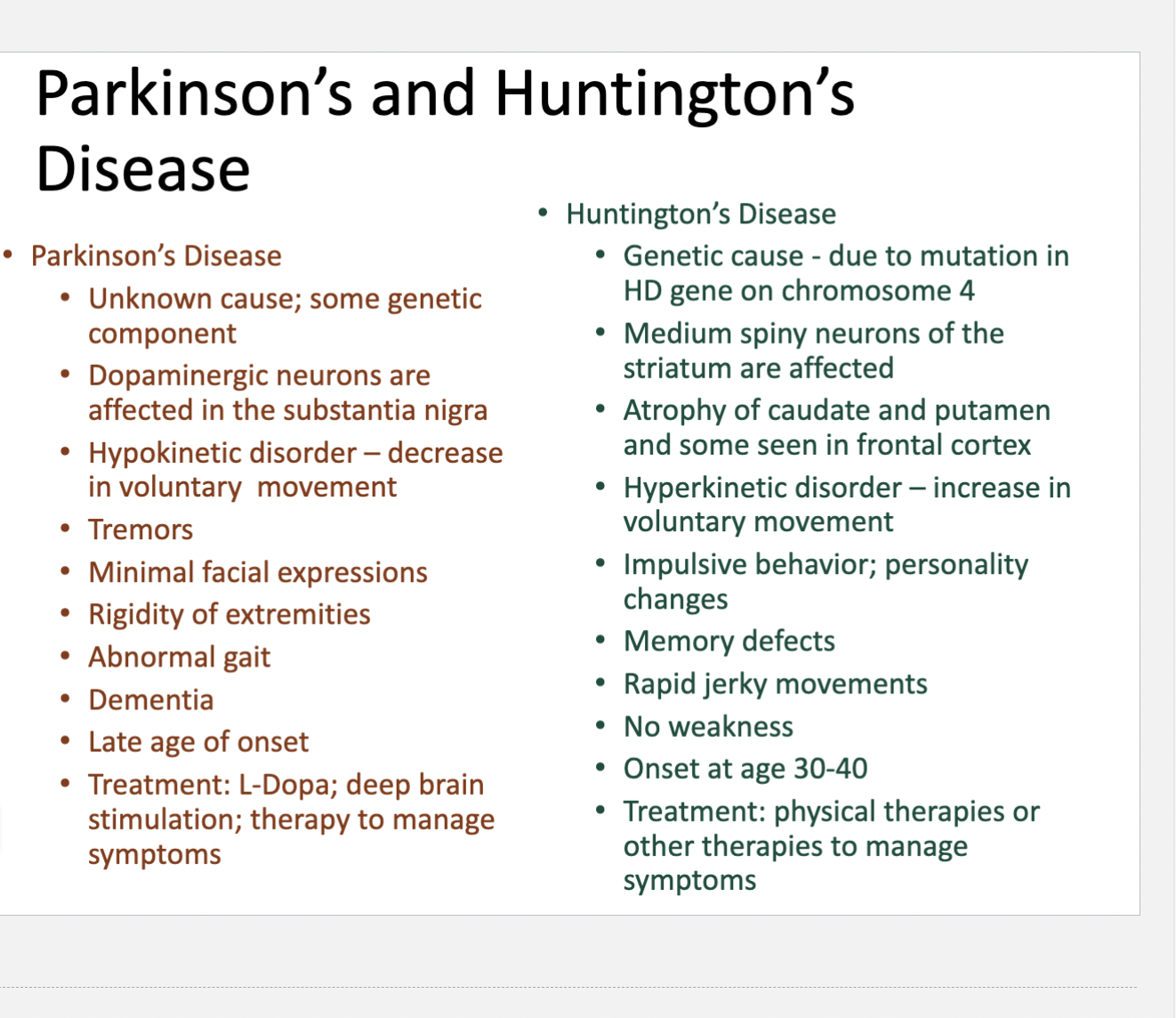
Parkinson’s vs Huntington’s
Cerebellum
Primary function is to detect the difference (motor
error) between an intended movement and the
actual movement – then influence upper motor
neurons to reduce the error
• Corrections made during the course of the
movement and as a form of motor learning
• Damage leads to persistent errors when executing
movement
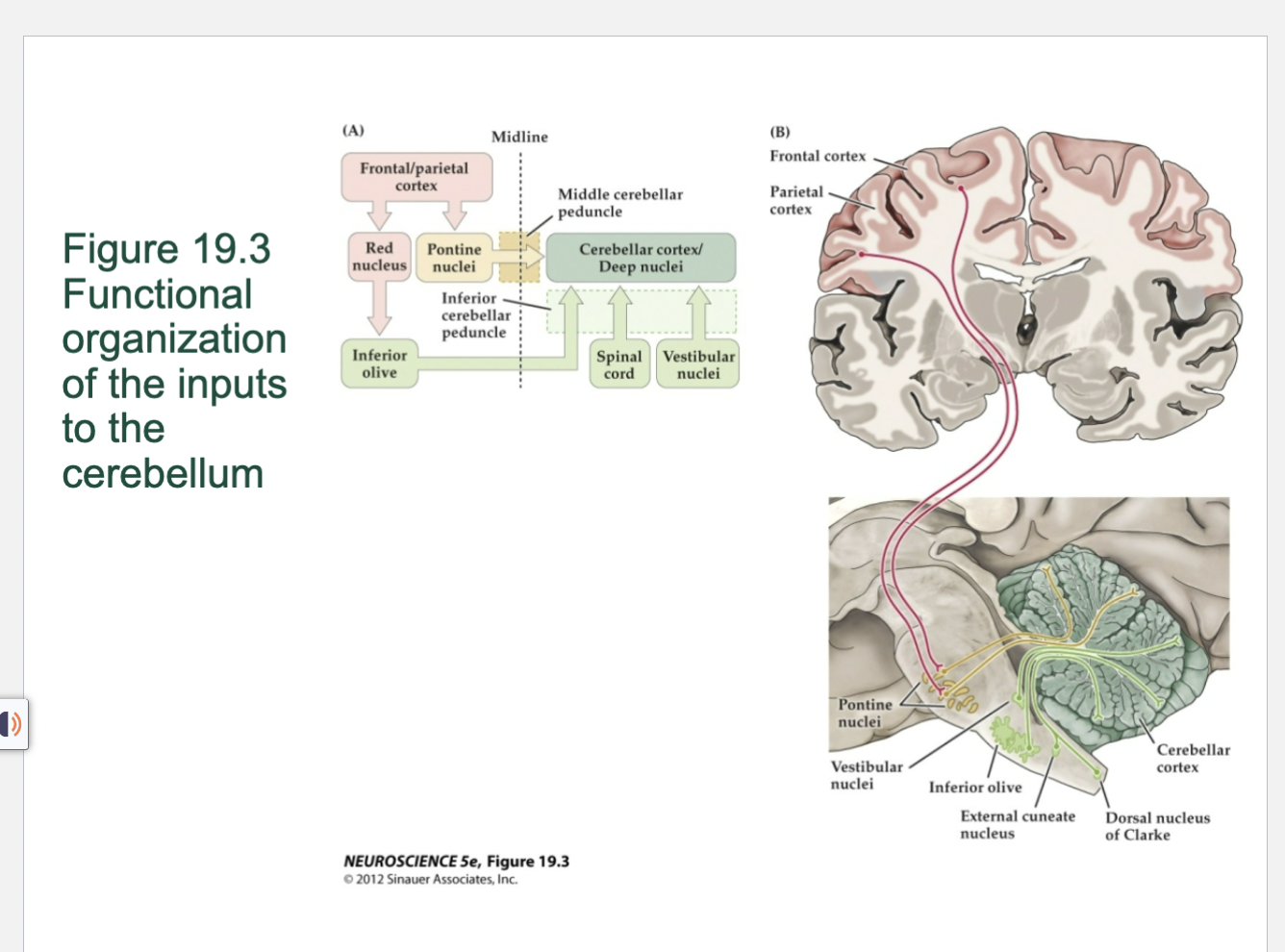
Figure 19.3- Cerebellun functional organization of the inputs to the cerebellum
(A) Diagram of the major inputs. (B) Idealized coronal and sagittal sections through the human brainstem and cerebrum, showing inputs to the cerebellum from the cerebral cortex, vestibular system, spinal cord, and brainstem. The cortical projections to the cerebellum are made via relay neurons in the pons. These pontine axons then cross the midline within the pons and project to the cerebellum via the middle cerebellar peduncle. Axons from the inferior olive, spinal cord, and vestibular nuclei enter via the inferior cerebellar peduncle.
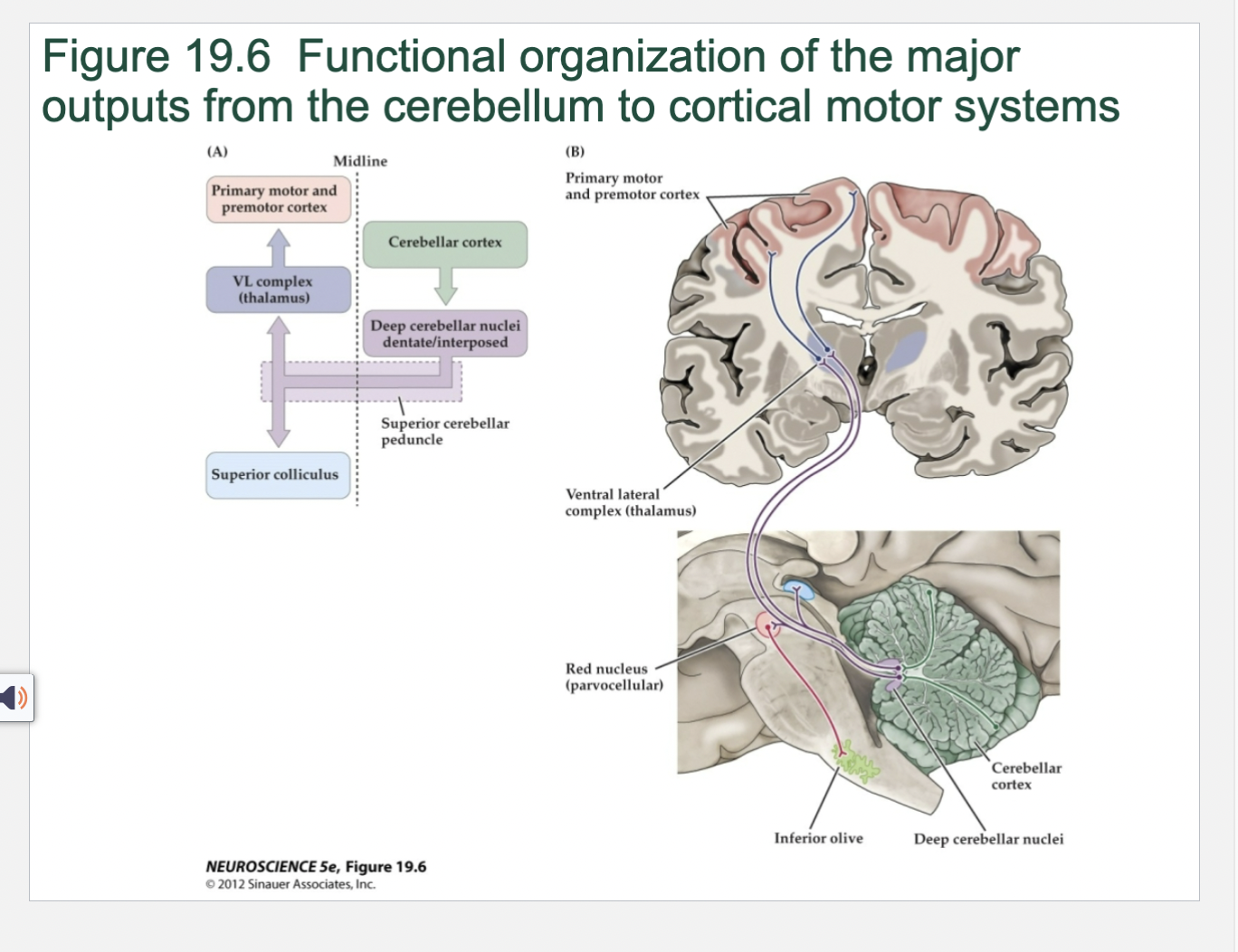
Cerebellum Figure 19.6 Functional organization of the major outputs from the cerebellum to cortical motor systems
(A) Diagram of major outputs that affect upper motor neurons in the cerebral cortex. The axons of the deep cerebellar nuclei cross in the midbrain—in the decussation of the superior cerebellar peduncle—before reaching the thalamus. (B) Idealized coronal and sagittal sections through the cerebrum and brainstem, showing the location of the structures and pathways diagrammed in (A) and a feedback circuit by which cerebellar output is directed to the inferior olive via the red nucleus.
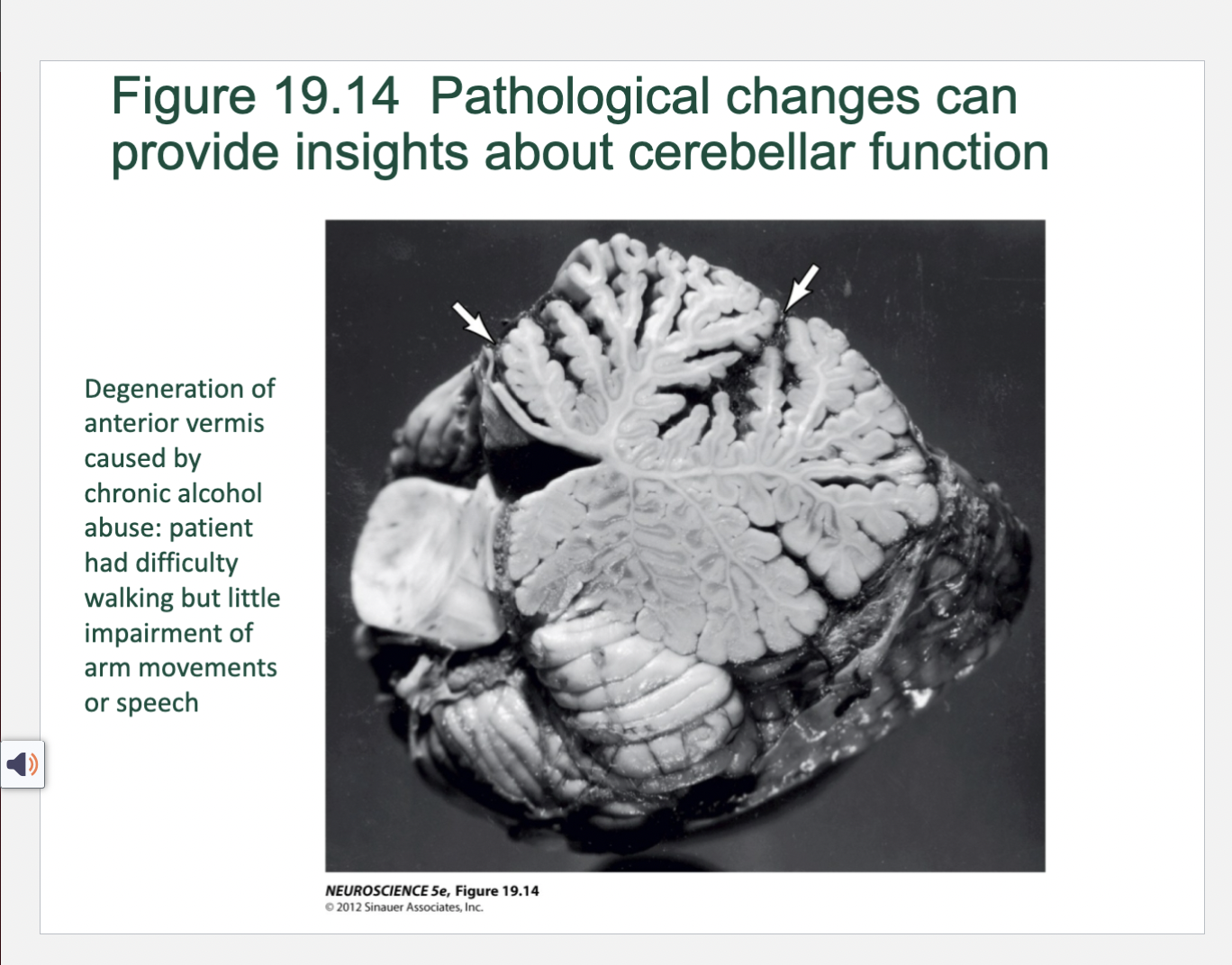
Figure 19.14- Pathological Changes can provide insight into cerebellar function
Degeneration of anterior vermis caused by chronic alcohol abuse: patient had difficulty walking but little impairment of arm movements or speech