20. Nematodoses of the small & large intestine of dogs & cats (strongyloidosis, toxocarosis, toxascariosis, ancylostomatidoses: Ancylostoma, Uncinaria, trichurosis)
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
43 Terms
What are the species of Strongyloides affecting dogs and cats?
Strongyloides stercoralis (FH: dog, rat, Hu, monkey) Zoonotic
Strongyloides tumefaciens (FH: cat - not zoonotic)
What is the location of Strongyloides spp. in the definitive host?
Small intestine (only females)
What are the transmission routes for Strongyloides spp.?
Skin penetration, ingestion of contaminated faeces, lactogenic (dog only), auto-infection (S. stercoralis)
What are the clinical signs of Strongyloides spp. infection in cats?
Usually without disease or small white nodules in colon, chronic diarrhoea.
What are the clinical signs of Strongyloides spp. infection in general?
Gastrointestinal symptoms (diarrhoea, flatulence, nausea, lack of appetite, abdominal pain)
Respiratory symptoms (dyspnoea, wheezing, cough)
Dermatologic symptoms (itching, erythema, urticaria, larva migrans cutanea)
Eosinophilia
Autoinfection → hyperinfection syndrome (in immunocompromised)
How is Strongyloides spp. diagnosed?
Serology, PCR, ELISA, flotation or laparoscopic methods (bearman), Koga agar plate.
What is the treatment for Strongyloides spp.?
Only effective against intestinal stages.
Benzimidazoles (fenbendazole, flubendazole)
Macrocyclic lactones (ivermectin, doramectin).
What are the definitive hosts for Toxocara spp.?
Canines (Toxocara canis), felines (Toxocara cati)
What are the transmission routes for Toxocara spp.?
Oral ingestion of eggs or L3 infected paratenic host, prenatal (transplacental; dogs only!), lactogenic.
What is the infective larval stage for Toxocara spp.?
L3
What type of migration do Toxocara spp. undergo?
Entero-hepato-pulmonal
Larva migrans (visceral and ocular) in humans, too
At what age does Toxocara canis undergo EHP migration?
If animal is < 3 months
At what age does Toxocara canis undergo larva migrans?
If animal > 3 months
Is there a an age dependence to complete the migration cycle in Toxocara felis infections, and if so, when?
No
What are the clinical signs of Toxocara spp. infection?
Light to moderate infections: asymptomatic or occasional vomiting, diarrhoea, & retarded development in young individuals.
Heavy infections in puppies
Tissue damage: caused by migrating larvae (liver, lungs, kidney) w/ formation of granulomas. Pneumonia, cough.
Intestinal infection: Vomiting, bloated abdomen, obstipation & diarrhoea, bloody faeces, anaemia, fever, anorexia, emaciation, scrubby coat, neurological disorders. Perforation of intestine - peritonitis.
Older dogs: asymptomatic
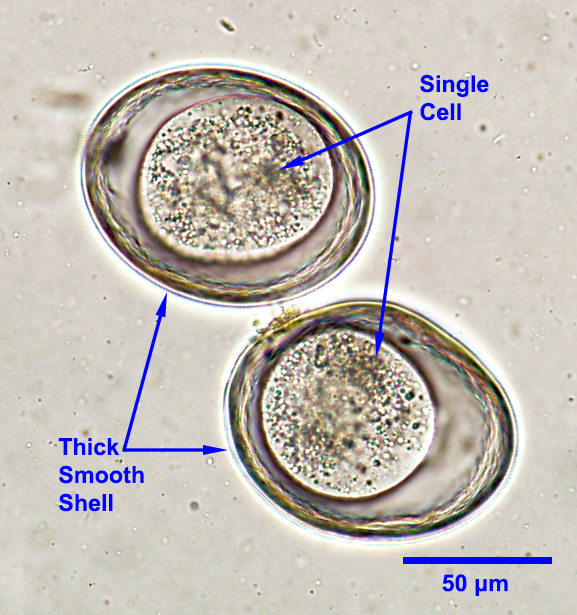
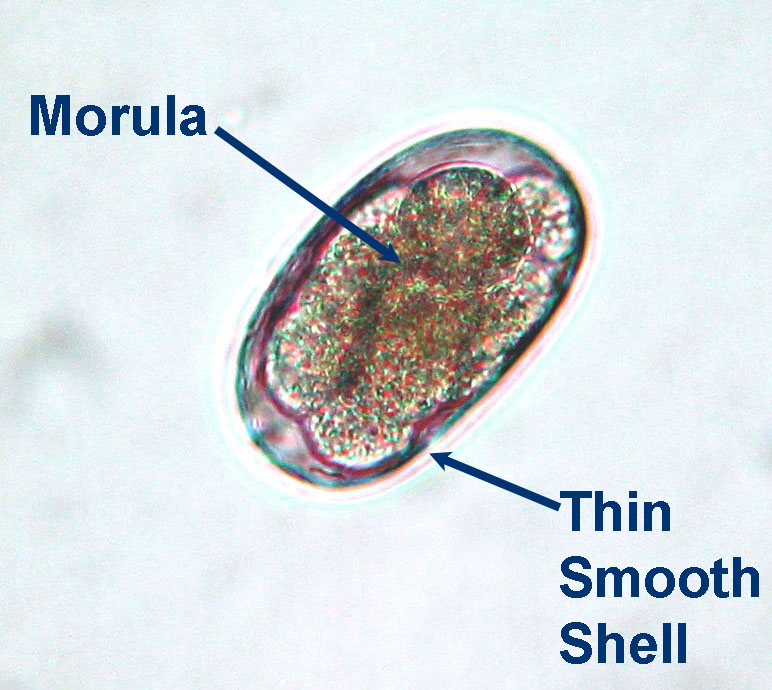
How is Toxocara spp. diagnosed?
Flotation technique.
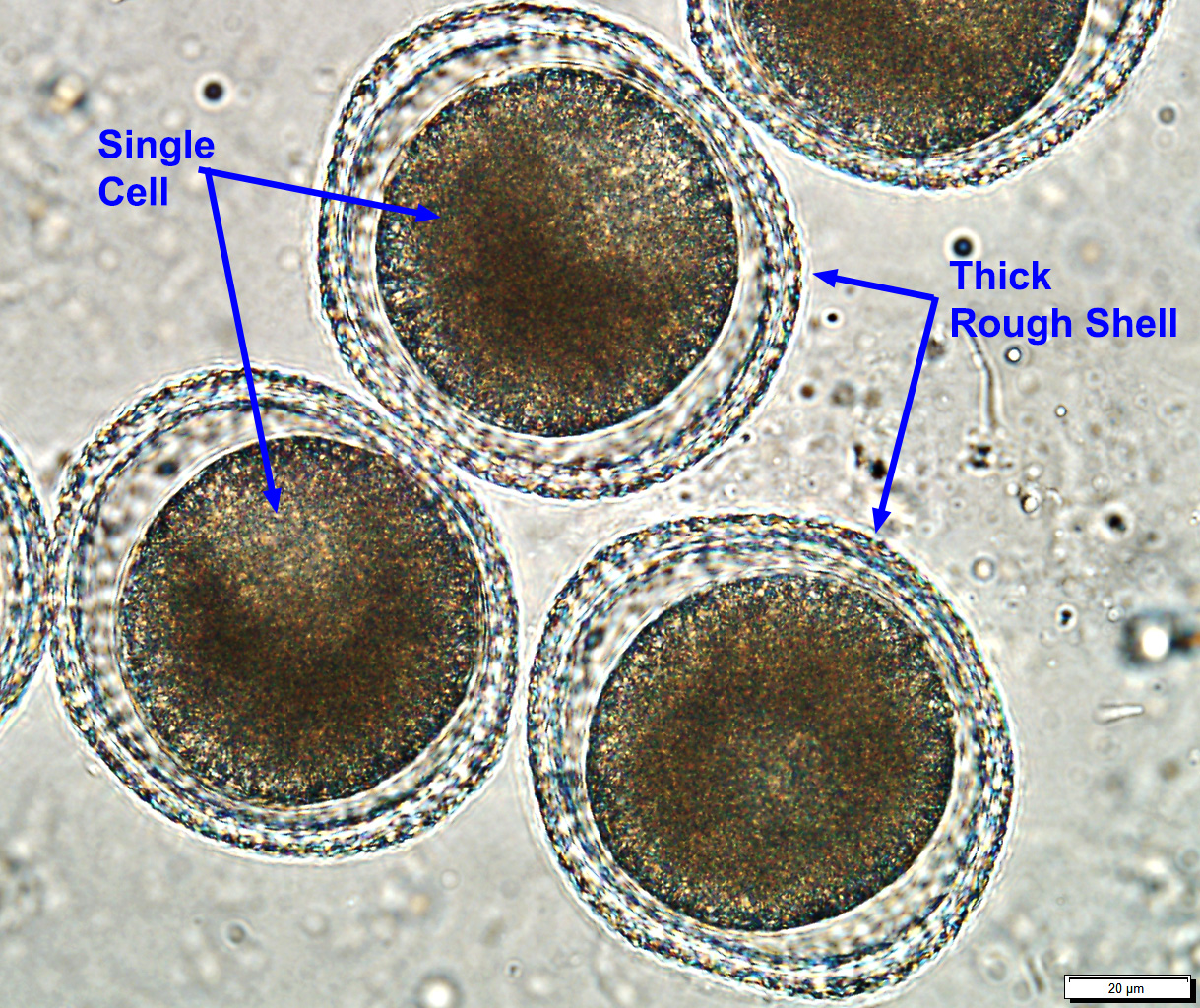
How can Toxocara and Toxascaris eggs be differentiated?
Toxascaris is smaller and lighter brown with a blastomere at one pole
What is the treatment for Toxocara spp.?
Adult worms: fenbendazole, albendazole, pyrantel
Larval stages: benzimidazoles (fenbendazole, flubendazole).
What is important for the prevention of Toxocara in puppies and kittens?
Puppies:
1st treatment: 10-14 days (transplacental; eliminate larval stages)
Subsequent treatments: every 2 weeks until 12 weeks; monthly until 6 months
Bitches: 2 weeks postpartum + after birth together with puppies
Kittens:
2-3 weeks old + weaning + 14 days post weaning (recommended monthly until 6 months)
Deworm nursing queen with kittens
What is the difference between Toxocara and Toxascaris life cycles?
Toxascaris does not migrate
What are the clinical signs of Toxoscaris leonina infection?
Potbelly and diarrhoea.
What is the treatment for Toxoscaris leonina?
Fenbendazole (larvae), fenbendazole (adults).
What is the species of Ancylostoma?
Ancylostoma caninum
What are the hosts of Ancylostoma?
FH: carnivores - small intestine
PH: rodent
Zoonotic
What are the transmission routes for Ancylostoma spp.?
Oral ingestion, skin penetration, prenatal, lactogenic.
How does Ancylostoma migrate through the body?
Intestines → lungs → trachea → mouth → intestines
What is the pathogenesis of Ancylostoma infection?
Intestines: attaches to and bites mucosa → melena
Larva migrans cutanea→ dermatitis and pruritus
What are the clinical signs of Ancylostoma spp. infection?
Anaemia, respiratory problems
Chronic: underweight, poor coat, loss of appetite, hypoalbuminemia, mild digestive upset, diarrhoea, bloody diarrhoea, dermatitis, pruritus.
How is Ancylostoma spp. diagnosed?
Flotation method, clinical signs, haematological examination.
What is the treatment for Ancylostoma spp.?
Adult worms: fenbendazole, selamectin, moxidectin
Larval stage: fenbendazole.
What is the species of Uncinaria?
Uncinaria stenocephala
What are the hosts of Uncinaria stenocephala?
Carnivores - small intestine. Cats less affected. Zoonotic
How is Uncinaria stenocephala transmitted?
Oral ingestion of L3 or PH
Skin penetration (rare)
What are the clinical signs of Uncinaria stenocephala infection?
Hypoalbuminemia, anaemia, mucoid diarrhoea, pedal dermatitis.
How is uncinaria stenocephala diagnosed?
Flotation method & larvoscopic for difference between species

What is the treatment for Uncinaria stenocephala?
Benzimidazoles (fenbendazole, mebendazole), macrocyclic lactones (ivermectin).
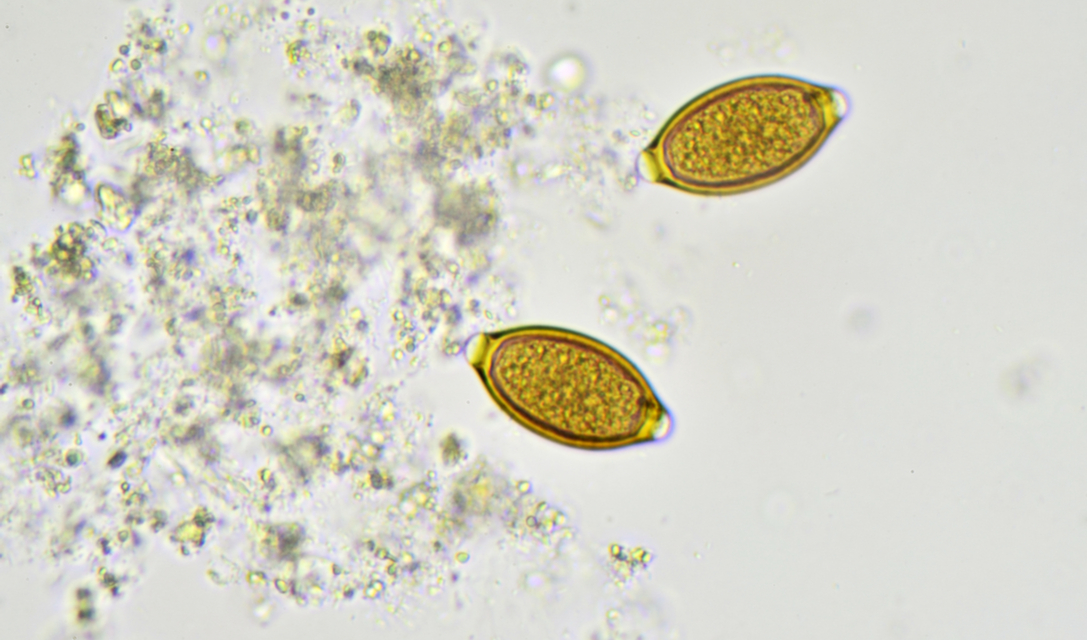
What is the species of Trichuris affecting dogs and cats?
Trichuris vulpis (FH: dog, fox)
Trichuris felis
What is the location of Trichuris vulpis in the definitive host?
Large intestine (caecum and colon).
What type of life cycle does Trichuris vulpis have, and what is the infective stage?
Direct. L1
What is the pathogenesis caused by Trichuris vulpis?
Travel into the intestinal mucosa
Low worm burdens are harmless.
Heavier infections: catarrhal inflammations, haemorrhagic colitis
What are the clinical signs of Trichuris vulpis infection?
Bloody diarrhoea, anorexia, anaemia, hypoalbuminemia.
How is Trichuris vulpis diagnosed?
Flotation method.
What is the treatment for Trichuris vulpis?
Fenbendazole, febantel, milbemycin, moxidectin.