Cardio exam 3... pray for me
1/77
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
78 Terms
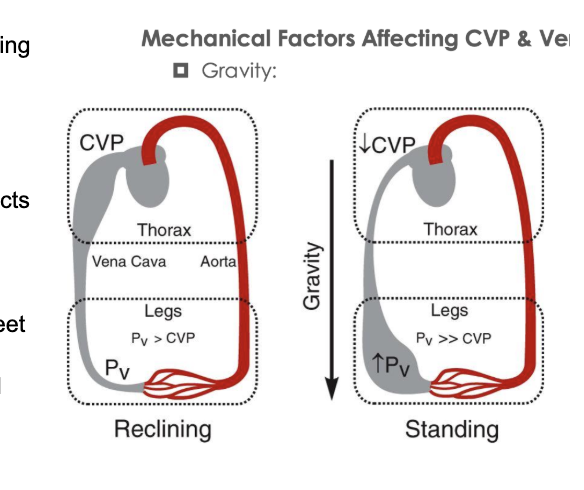
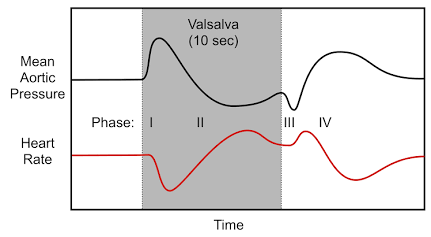
What are some of the manical factors affecting CVP and venous return. what is the relationship vetween venous pressre and central venouspressure when standing and when reclining
Gravity
reclinig= relatively uniform blood distribution
Standing= gravity acts on vascular volume and blood accumulates in the lower extremites
venous presure in the feet can reach 90mmhg
reduction of preload and sv by frank starling in the right ventricle
systematic areterial pressure falls more than 20mmhg upon standing
orthostatic hypostension
Skeletal muscle pumps
1 way valves allow blood to return to the heart (prevents back flow)
deep veins are surrounded my msucles = causes compression that opens and clsoes the vlaves
uses rhymatic contractions to enhance enous return and CO
Wat is the map equation
MAP = CO (SVxHR)xSVR
What causes varcose veins
damage in the valve sof the veins which causes swelling and venous twitingg
what is the resporatory pump
increaed rate and depth of breathin increases venous return and CO
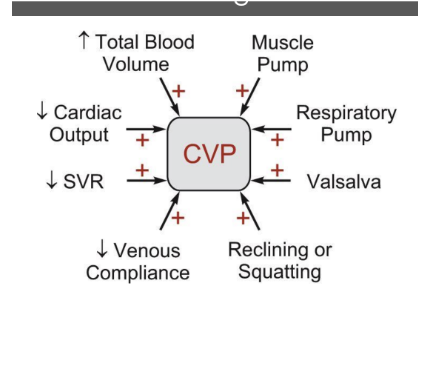
What are some of the factors affecting CVP
blood voulme (positive assotiaion
cardiac outuput (negative association)
SVR (negative association)
venous compliance (negatinve association)
muscle pumps (postive assoication
resporatory pump (positive association)
postural changs (reclining or squatting increases central venous pressure.)
What is the relationship betwen venous returnand cardiac output
Venous return = map - RAP/SVR
venous return acan equal cardiac output in stayd state conditions
bloodflwo through the entire system (CO or VR) depends on cardiac fucntion or systemic vascular function
sysstemic vascular and cardiac curves guton lots
Describe the interdependance of CO and VR. what are the 2 rules
REturn supports output
cardiac output is dependant on preload. reload is determeind by filling pressure (CVP)
Output creates return
high hrs can cause a lwoer CVP
lower hrs can cause CVP to increase
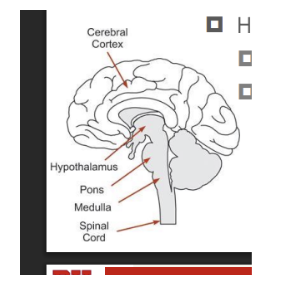
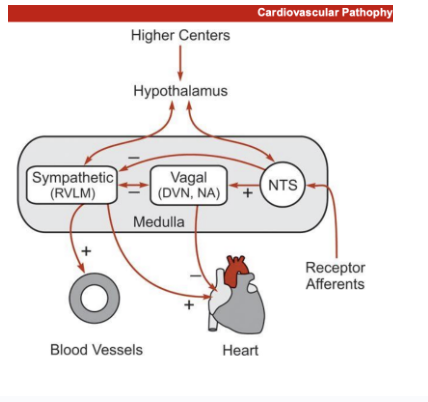
What are the functions of the medulla, hypothalamus an dhiger centers to controlingautonomic innercation. what are the structures involved
Medulla
contains cell bodies for parasympathetic and sympatheti efferent nuerons
hyppothalamus
pareaventricular nucleas and dorsal medial nucleas
they integrates and mdulate medullary neuronal activyt
higher centrs
cerebral cotes, limbic, and midbrain structures
connect with the hypothalamus and meddual to modculate activty during emotaional stres
Top down control
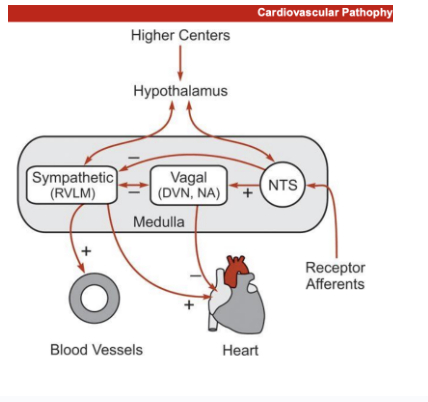
Understanding the diagram (medulla). How does functional autonomic control from sympatheic, vagal, and nts (receptor afffernetns) impact lbood vessle sand the heart (all in the medulla)
only one parasympathetic or sympathetic cna be turned on
Sumpathetic activity controled by the hypothalamus
increases vasoconstriciton of the blood vessles
increase contractility of the heart
reduces activity of vagal nerves
vagal nerves
reduces the activity of sympathetic structures
controlled bby NTS from receptor afferents
reduces contraciitlity of the heart
nts
impacted by the hyothalamus and receptor afferents
increases vagal activity
What is parasympathetic innervation from the medulla. what is the DVSN and NA
DVn -dorsal vagal nucleus
NA- nucleus ambiguous
reduces SA nodal firing (negative choromotrofy
slowls AV conduction (negative dromotrophy
minimal impact on ionotrophy bc parasympathetic primarlay impats the aorta
afferent nerves modualte activity of the vagla neruon
baroreceptors from the NTS
What is the anatomy of parasympathetic innervation: pregangion fiers
postgangion fivers
wehre do they work. what hcan they impact
preganglionic fivers
efferent fivers synapse within or near the target tissue and form small ganglia
they projet form the cs to a ganglion (cluster cell of vodie)
short postgangion fivers
innervate secific tissue cites
cell body is in the gangion long pre gannlgion
not ture gangion will tyically synase in or near target tissue short post gangion fiver innervates local target tissue
Increased ns activit can cause
ACH induced direct vasodialation (genitals)
Indirect vasodialation by stimualtion productio nof vasodialttory substances (gi circulation)
enhances blood flow to promote nutrient pickup
What is the function of sympatheic innervation. what does it originate form and what doe sit impact
originates from nneurons in the medulla (Rostral ventrolateral medulla RVLM)
icncresed SNS firing =
increased cardiac stimulation
increased chronotrohy dromoropy, and ionotropy
increased vsoconstriction
What do barrorreflex affernet neruons impact
the NTS and valal functioning
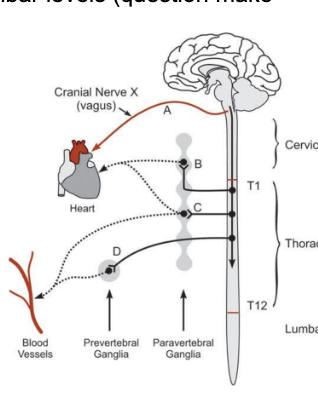
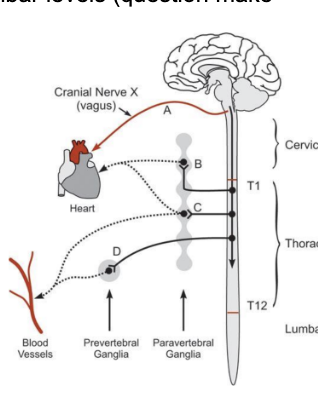
What is the anatomical structures of sympathetic innervation. parav ertebral gangliea, prevertebral ganglia. how does it travel down. post ganglionic sympathetic fibers
SNS axons leave the medula, travel downw the psinal cord and snapse within the inermediolateral cell colum of the spinal cord
axons exit at hte thoratic and lumbar sine
preganglionic fibers then synapse within syphatetic paravertebral ganglia (bundle of cells) on both sides of the spinal cord
or they synapse iwthin prevertebral gangila located in teh abdomen
post gangionic fibers travel to target organs where they inervate the arteires and veins
Draw out and understand the diagram .the remation between the higer structures of the brain. paravertebral gangia
prevertebral ganglia. blood vessles. the heart. the spinal cord. sympathetic projections. cranial nerve x ( vagus nerve)
parasympathetic innervation
fiters from spinal cord to pregangionicc fibers from the medolla to preautonomic fivers
1) sympateic project from RVLM down the cord to preganglionic neuron region (thoractic)
t1 to t12 pregnanglionic nerves
2) synapses onto the pregnalionic neuron which projects out of he cord (paravertebral ganglia)
3? post gangionic neurons projects onto the heart
B/c = paraverebral gnaglia. used to inervate the post gangion neurons that project to the heart and blood vesls
es
C. projects into the post gangion neuron projects in both the heart and blodov essles
D/ synapses to the post gangion projects in the blood vessels form the revertebral ganglia
Describe the impacto f sympathetic and parasympathetic funcitonig on: chronotorphy, ionotropy, dromotrophy, vessles, resistance, and capitance
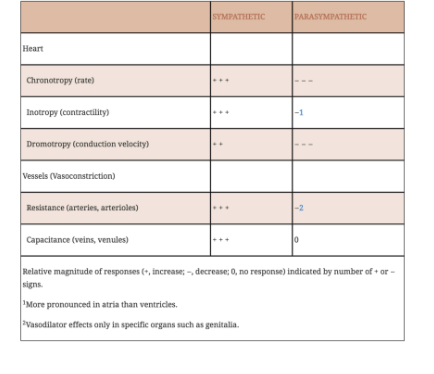
how does reciprocal integration aid in acue and ongterm control of blood prssure. what is stronger. waht can alter these functions
reciporcal integration of the PNS and SNS aid in acute control of blood vessle
vagal influences are dominant over sympathetic influences of the heart
hr.< sa nodal firing pace
without reciprocal intgration = continuous parasympathetic activity.. no response to external stimulus
higer corticla regions alter atuonomic (parasympathetic) functioning
fear
vasovagal synchope
stressd
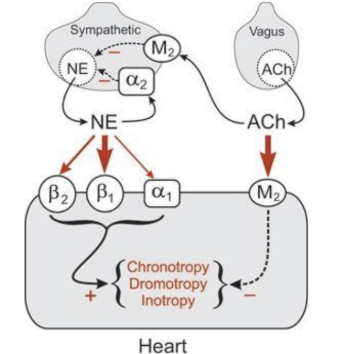
Draw the dagram Where is ACH and NE released from in the symathetic and parasympathetif ccuntionig
What are the receptors of the parasymathetic system/nerves
what are the receptors of the vagus nerves (hint hint… this is more dominiant)
What dos NE and ACH react with in the effector receptrs… what is the result (the heart)
where are parasympathetic things found
ACH is released from vegas nerves
NE is released from syapthetic nerves
Sympathetic nerves have alpha 2 and M2 receptors. A2 receptors react with NE. M2 receptors react to ACH
these slow down NE production
Vagus nerves have no receptors (they are found in the cns at the medulla
NE reacts with
A2 (found inthe sympatehtic cellls
cuts down ne productions
A1 ( in the heart cells)
increases sympatheic fucntioing
B1 (highest reception) Heart cells
B2 (found in the heart ceells)
ACH
reacts with M2 receptors in the heart cells for parasympatheticc functining
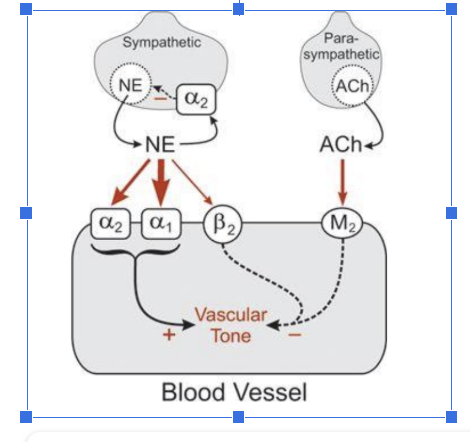
Draw the dagram Where is ACH and NE released from in the symathetic and parasympathetif ccuntionig
What are the receptors of the parasymathetic system/nerves
what are the receptors of the vagus nerves (hint hint… this is more dominiant)
What dos NE and ACH react with in the effector receptrs… what is the result (the blood vessles)
where are parasympathetic things found
Symatpehtic nerves
have a2 receptors (responds to A2)
relesase NE
Parasympathetic nervse
releases ACH
no receptors on it
note there is no interaction iwthsympathetic nerves because there are barey any parasympathetic nvers in the blood vessles
NE
responds to a2, a1 (primary) and b2 receptors
ACH respponds to m2 (minimally becuase there is baly any symatheir c nerves in the vvasculatore
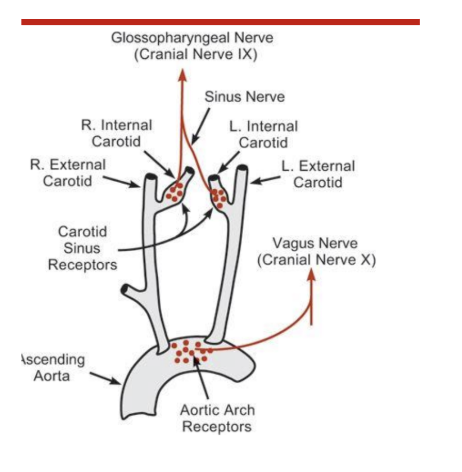
how to baaro receptors regulate arterial pressure. where are they found. waht nerves are involved (sinus nerves, glossopharyngela nerve, vagus neerves, aortic nervs)
Areterial barorecepotrs are found in the cartoid sinus and the aortic arch
the sinus nervve (glossopharyngeal nerve (cranial nerve IX)
innervates the cartoid sinus
travels from the carotid sinus in the glossopharyngela nerve up to the brainstem wehre they synase at the NTS
afferent fibers from the cartoid sinus travel i
the aortic arch barro receptosres are innervated by the aortic nerve (combines with teh vagus nerve) before traveling to the nts
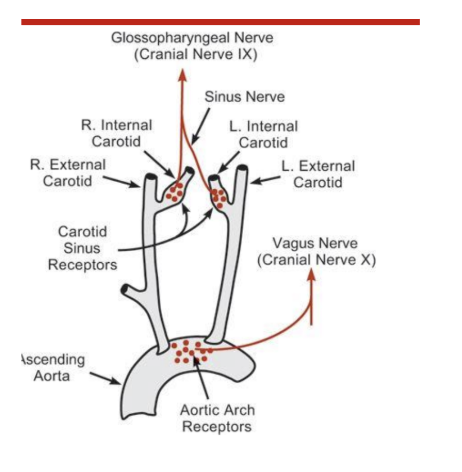
understanding the diagram. wehrea re these nerves found. Glossophryngeal nervs. Aortic arch receptrs.
where is the sinus nerve. werhe is the bvagus nerve
ahhhh
HOw does the stres response to barro receptors impact the heart or whateer
arterio barro recepotrs reposnd to stretching of vessel walls produced by an increases in arterial blood ressure
increase in arterial pressure = increase in firing rate of individual receptors and enrves
the aortic arch baroreceptors function simlar to carotids
have higher threshold pressure fo r firing and are less sensitive than the cartoid sinus receptors
cartoid baroreceptrs are prdominate acute bp regulators
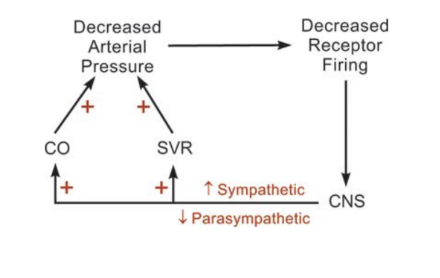
how does a change in arteriaal pressure imact CO and SVR. draw out the diagram
how does it relate to receptor firing, the CNS. CO and SVR (barroreceptors)
low bp decreases arterial blood pressure
decreased receptor firing increased
stop activation of the NTs (NTS will not inhibit sumpathetic activation)
increase in sympathetic nerves and decreases in parasympatheic
increase in both CO and SVR
both increases arterial rpessure
Where are additional low pressure rreceptors found in the body
Waht do they respond to
what is more dominant
riight atrium, low venoatrial junction, and the pulmonary arterial cirnculation
reponses
they respond to atrial filling and are tnically active
increased venous return
increaed PNA (acardiac) and reduces SNA due to para sympathetic nerve activation
Decreased ADH release - adh come sform pituitary but some comes form the heart
used to reudce blood vlume
As the cardiopulmonaries become more sielent = sns becoems more dominant
areterial baroreceptors also help due to low stretch
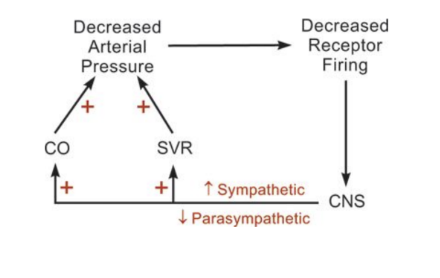
how does sanding impact parasympathtic and sympathtic activity
1.standing = pooling of blood at the feet = reudced filling ofthe heart = increaed sympathetic activity
ANS responds with baroreceptor reflexis
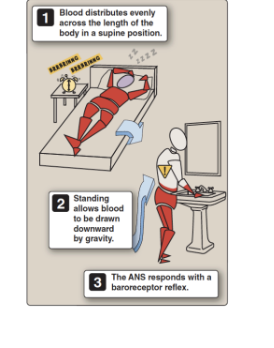
describe and draw out the valsalva manuver. whatare the different phases and what would happen in changes in alteration
phase 1
begning of the forced expiration
aortic pressure increases due to aortic cpomression and the heart rate decreases refleixively - barro receptors are stimulated
causes reciprocal cahges in bp and hr (decrease
phase 2
aortic pressure falls during pahse 2
compression of throatic veins reduces venosurs return and cardiac output = reflex tachcardia occurs (reduced stimulation of the barro receptors
phase 3
small fall in aortic pressure do the loss of thoractic pressure. increase in heart rate due to reduced barroreceptor stimulation
increase venous return raises aortic pressure onece again = rediuction in heart raate
phase 4
normal cardiac ouptut while svr is elevated from sympathetic activation durigng phase 2
overshoot in aortic pressure
heart rate falls a little bit
What are the steps by phases
phase 1
infrease in intrathorastic pressure
phase 2
increase in aortic pressure
baroreceptor response to drop the bp
hr plummets
svr and ivc colapse. no vagus return to the heart = reduced s
bp drops hr increases to make up for the decreases in stroke volume
phase 3
breathing normally
small fall in aortic pressure do the loss of thoractic pressure. increase in heart rate due to reduced barroreceptor stimulation
increase venous return raises aortic pressure onece again = rediuction in heart rate
drops in intrathorastic pressure increase hr
the backued up venous return in the heart drops donw hr and increas stroke volume
What ar echemoreceptors and what can they do in the heart
they cna influence medullary cardiovascular centers drectly or indirectly
through altered pulmonary strech receptor activity
specialied cells located on artieres in the medulla motor blood po2, pco2. orr ph
function is to regulate resporatory activity to maintain arterial stable pressrues
sympathetic funcioning is stimulated by what
decrease in po2
increase in pco2
decrease in blodo ph
what areperipheral chemoreceptors and where are they found
lcoaeted in small caroitid bodies and aoritc boides.
respond to a fall in po2
an elevation in pco2
a decrease in ph
what are chentral chemoreceptors. hwere are they foudn and what do they respond to
located in the medulla *can directly sense blood bc not surroudned by blood brian barreir)
responsd
increased co2
decreaed ph
increased h+ ions
does not detect po2
What hormonesdoes the adrenal medulla secrete
80% e and 20% ne
what is the use of pinephrine in the cardiovascular system. waht receptors does it bind to
it depeodn son the distribution of cadreneric reepcetors and the afinites of the recpeotrs for epinephrine
primary repsonsive to b receptors (b1 mostly). still reacts ot b2 and a receptors (a andrireceptors)
b1 in the heart
what is the sue of norepinephrine in the heart and what recpetors are they most responsive with
norepinephrine = neurtranspitter and alpha hormoen
released form sns neoursons as a neurortransmitter
released form the adrenal medulla as a hormone
afinity for noe for b1 (heart) and a1 (vessles) receptors = greater than a2 and b2 receptros
causes an increase in hr and vasoconstriciotn
What happens if you adminiserter ne and e clinically
(look at terries slide im tired)-
Epineprine
increase in hr from binding to b1 receptors
decrease perhiperal resistance because increasei nhr = barroreflex withdraws sympathetic tone
vasodialation
increase in CO because e is still present
arterial pressure and puls pressure widesns but maps stays the same
tpr decreases =. diastolic pressure decreases ore impactuflly = not a change in map
NE (works more strongly in the vasculature)
increase pherhiperal resistance. svr/tpr becuase of thea ctivity of a receptors
ne at the heart but parasympathetics will cancel it out (ne isnt as strong)
parasympathetics dont have an effect on the vasculature = increase in tpr decreases in co increase in diastolic pressure and increase in map due to increase in diastolic
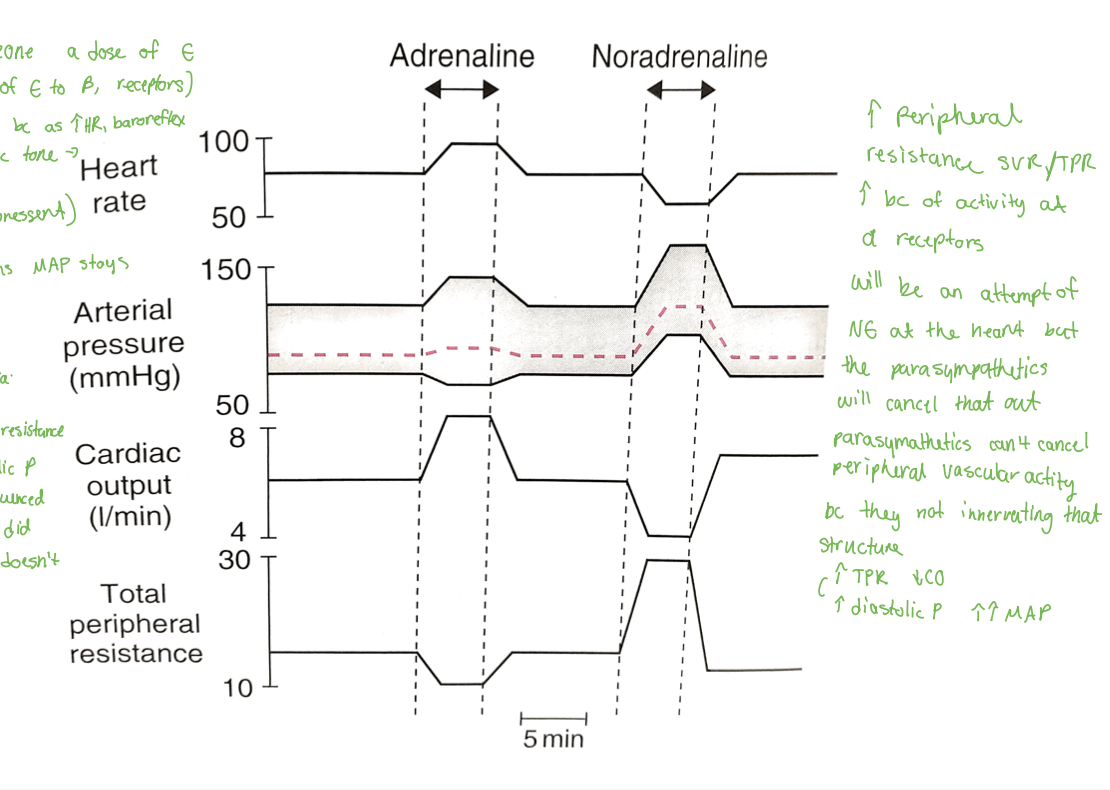
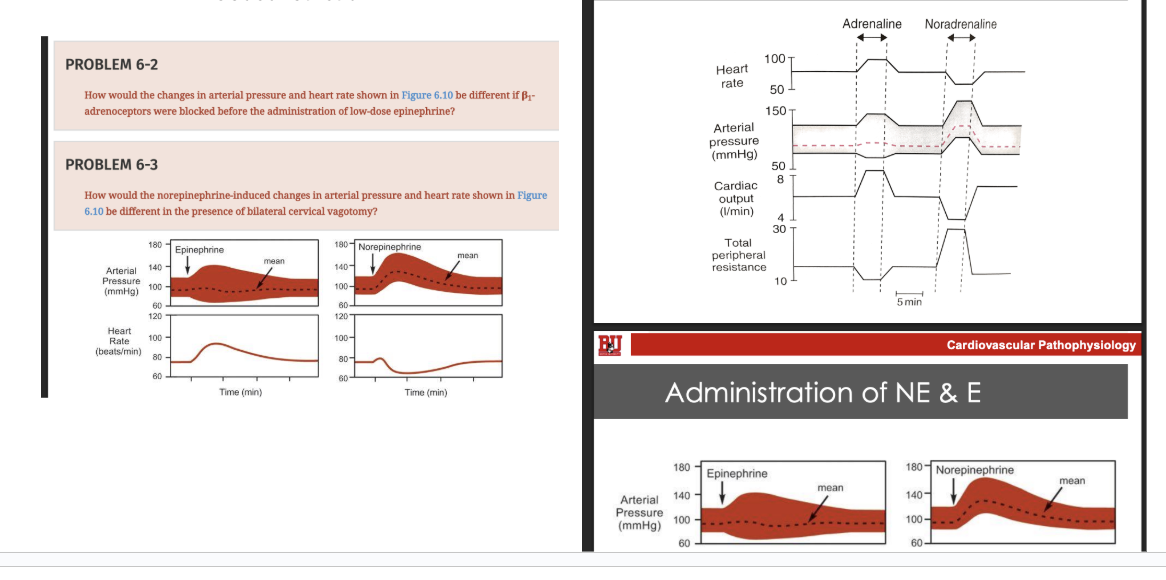
figure this shit out
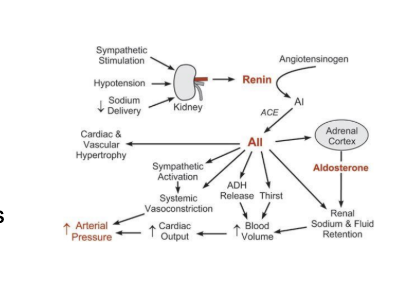
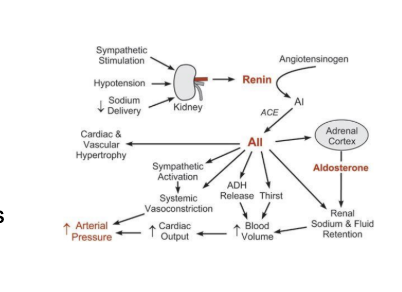
What is the function of the RAAS sytem. what does it do and what does it contorl
impacts blood volue cardiac otuput, and total peripheral resistance
Understanding the RAAS cycle. draw it out
. which factors are the most impactful chainging arterial pressure. what is the fucnction of the kindeys, renin, angiotensinii ace, angeotesin 1 and aldosterone
Renin is an enzyme that acts on angiotensiongen
Angiotensisin then transforms to angiotensin 1
Vascular endothelium (in the lungs) - uses ACE that cleves off two amino acids to from angiotensin II
coontroling cardiac output through sv (blood volume) is th emost impactful
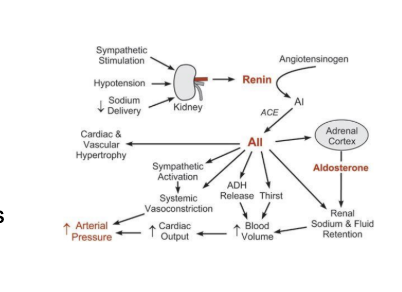
What is the fucntion of angiotensin ii in the RAAs system
Constricts resistance of vessels = increasing SVR and TPR’
Enhances sympatheti andrenic activity (TPR, HR, SV)
Acts on the adrenal cortex = aldostrone release (fluid)
Stimulates vassopressin release from posterior pituitary (SV, TPR) (ADH)
Stimulates thirst centers in the brain (SV)
Stimulates cardiac and vascular hy[ertrophy (SV-long term)
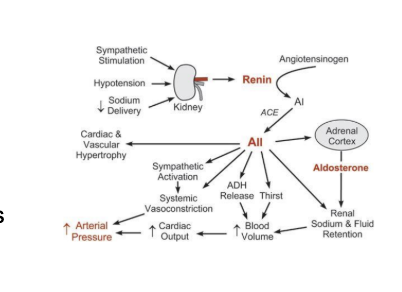
what are teh different ways to manipulate raas and what are the result form them. Aledosterone, ACE, renin. Kindey disfuction. Adrenal corte x disfunciton. DRAW it out
Very common for hypertension and heart failure
ACE inhibitor s and AT1 receptor blockers do teh following
Decrease arteriol pressure, ventricular afterload, blood volue, and ventricular preload
They inhbit and reverse cardiac and vascular remodeling
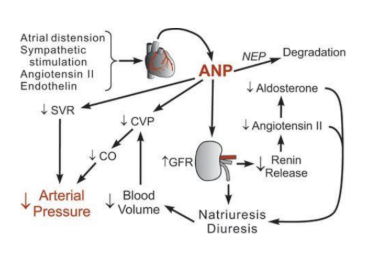
Where is renin released from. Where is ANP released form
Renin= the kidneys
AnP = the heart
Waht is ANP and what does it do. What sitmulates ANP release. Draw out the cycle
ANP- atrial natriuetic peptide
It is a counterregulatory system for the renin-angiotensin-aldosterone system
28 aminoacid peptide synthesized and stored in response to atrial distension, angiotensin ii stimulation, endothelin, and sympathetic stimulation
Elevated ANP are found during hypervolemia and congestive heart failure causes atrial distension)
It helps facilitate offload and create a balance for blood volume volume
atrial distiension
sympathetic stimulation
angiotensin ii
endothelin
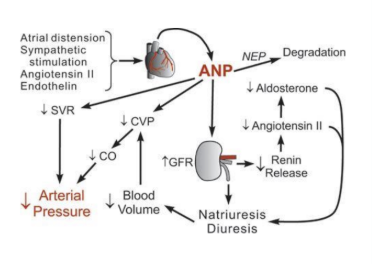
What are the effects of ANp release.draw out the diagram. how is it impacting aldosterone, angeiotensin ii, renin, and caridac ouptut. and the kindesy
Decrease in aldostrone, angiotensin 2, renin release = natural diuresis = reductio nin blood volume reduced cvp
Reduced CVP, readuced CO, reduce SVR and overal reduced atrial pressure
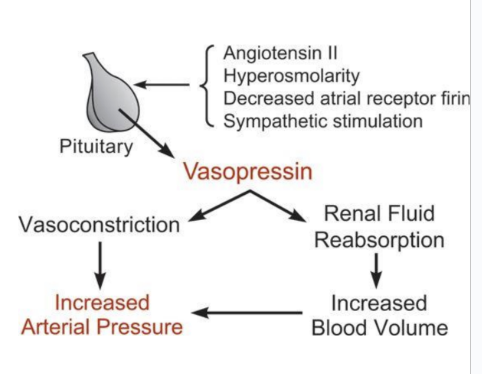
how do you modulate ADH (vassopressin (ADH control)). waht is its function. wehre is it released from
ADH = increases water reabsorption by the kidnesy
increasing water permeability of the collecting duct
ADH = nonapeptied hormone relased from the posteiro pituitary
two principal sites of action: the kidnesy and blood vessels
ADH is antidiuretic via renal v2 receptors
constricts arterial blood vessles but hte normal physiolgoic oncentrations of AVP are blow its vasoactive range
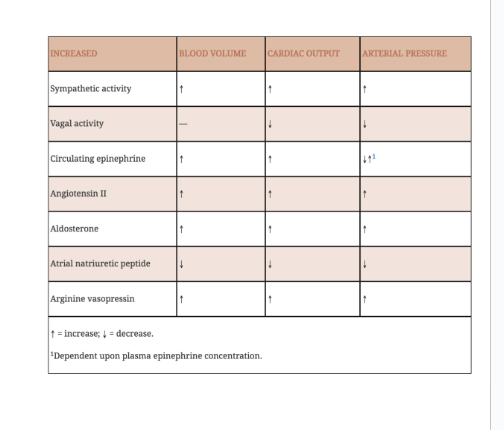
how do the follwing impact blood volume, cardiac output, and arterial pressure
sympathetic activity
vagla activity
crculating epinephrine
angiotensin ii
aldosterone
AnP
and vassopressin
descrobe wju
understand teh diagram… waht does it mean
save meeee
What are the different categories for high blood rpessure: normal, elivated, sage 1-2. sever and hypertensive for both systolic and diastolic
look at diagram
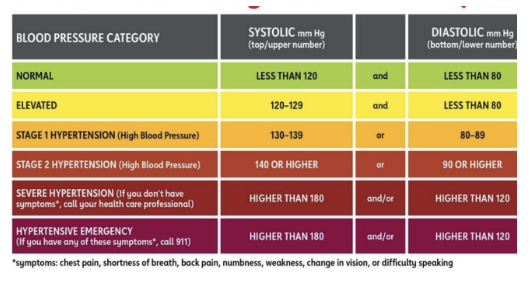
What quantifies severe hypertension vs a hypertension emergency
Severe hy[ertension
Death is not imminent
May be harmful to rapixly lower blood pressure
No need to immediatley treate
Not that acutely dangerous
Treatnment starts with pcp
Htn emergency
End organ damage is evident
Death is possible
Immediate control of bpis critical
What is the difference between pulmonary and systemic hypertension
Pulmonary
Not as well studied
Not as treatable
Worse prognosis
Comes with comorbidities
Systemic hypertension
Common
Mostly treatable
Common precursor for other ocnditions
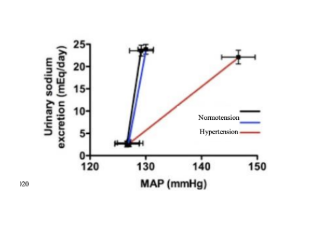
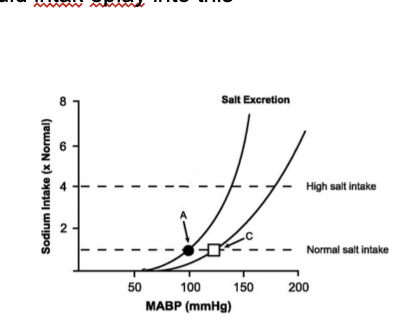
What are some o the causes of hypertesniosn
Typically bigins with hypervolemia
Increased sodium and water retention
Renal pressure natiruesis corve is shifted = higher atrial pressure is required to maintain sodium balance
Altered kidney filtration and sodium balance in renal disease = shift in pressure naturisis = hypervolimia
Understand the diagram. Draw out the kidey RAAS system and understand how kidney disfunction, adrenal cortex disfunction, and how it can i mpac atrial pressure
raghhh
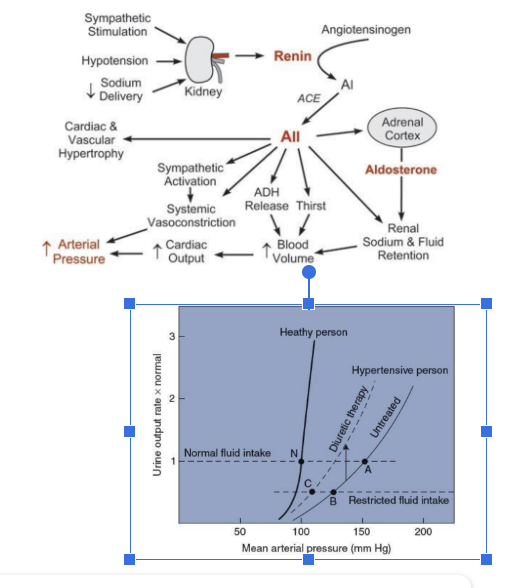
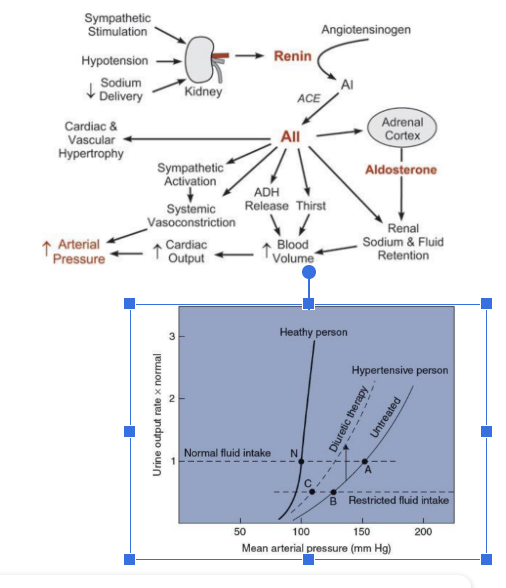
How does urine outut and fluid intake impact map in a healthy perosn, untreated, and treated hypertensive person. How does restricted fluid intak eplay into this
Waht is essential hypertension (90-95 percent of cases)
Diagnosis by exclusion
Increased sodium and fluid retention is a primary factor
Vascular changes = can contribute to hypertensive states
Especially with renal disfunction
Related to heredity, age, race, and ses
Some patients are more strongly influenced by stressful conditions than are normotensive individuals
What is secondary hypertension and how frequent is it found in the body (5%-10% of cases)
Renal artery stenosis
Renal disease
Hyperaldosterone (primary)
Phechromoctoma (cathacholamine- secreting tumor)
Aortic coarctation
Pregnancy (preclampsia)
hyperthyroidms/hypothyrodism
Cushing system
Sleep apnea
How does dysfunction inthe CNS PNS and gut microbiome impact hypterteions
Dysfunction in the Cns
Inhibition of sympathetic outflow (reflex inhibition)
Exaggerating intrinsic firing of sympathic centers
Causes excessive vasoconstriction
Causes excessive sodium retention
PNS
Afferent renal nerves are not functioning properly
Gut microbiome
Alteredgut microbiota generally impacts bp
Inflammation peripherally and in the cns ude to changes in circulating factors
What are some of the common tyes and factors of secondary hypertension: describe the following
renal artery stenosis
renal disease
primary hyperaldosteronism
cushing syndrom
preclapsia
pheochromocytoma
hyperothryrodis
aortic oarctation
sleep apenae
Causes identifiable and possibly treatable
Renal artery stenosis: renal artery becomes narrowed (stenoic) = owing to atheroschelrotic or fibromuscular lesions
Renal deseisse: damaged kidney nephrons
Prymarey hyperaldosteronism: increased secretion of aldosterone by an adrenal adenoma or adrenal hyperplasia
Cushing syndrome: excessive glucoracoitd secretion = leads to hye=pertension
Preclapsea: occurs in 5% of pregnaies during late second and third trimesters
Pheochromocytoma: catehcolamine-secreting tumor (in the adrenal medula)
Hyperthyroidis: increase in blood volume and increaed cardiac activity = hypertension
Aoritc oarctation: narrowing of the cardiac arch usually distal to the left s ubclavian artery
Sleep apnea: a disorder which people stop breathing for short periods of time during their sleep
What are some of the symptoms of cushing syndromeWhen the adrinal glands excrete too mcuh cortosol
Cns irritablity
Hypertension
Cardiac hypertrophy
Hyperphalsia (tumor on kidneys = really bad)
Obesity
Osthero perossi
Muscle wasting
how can ventricular hyertrophy relae to lala’cslaw
afterload = wall stress
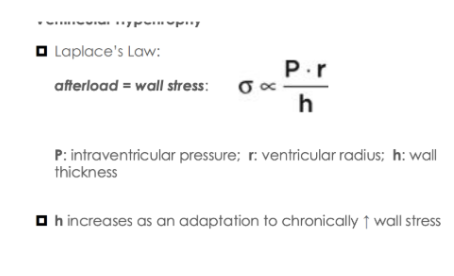
What are some of the compensatory cardiac and ventricular adaptations to high blodpressure
Cardiac
Concentric hypertrophy: more sarcomeres in parallel
Like lifting weights in the gym
Wall stress decrease
Stroke work increases allong with diffusion distance
Vascular
Vascular myocite hyertorpy
Narrwoign of the lumen
Reduces complanced
Accelerated cv agin
What are some of the therapeutic intervention methods
sed to correct secodnary hypertension (treats the underlying cause)
You n eed to addres CO (SV and HR) and SVR
What is the most effectiv evaraible when addrsing hypertension (SV vs HR) - what are the pharmalogical methods used
HR
HR
Use of beta blockers (typically given with diurents to reduce blood volume)
Uses calicum channel blocker
Not verry effectiv bc SV is more affective in CO
SV
Diuretics reduce blood volume (most common treatmetn)
Ace inhibitors
Given with diuretics
Andiotensin 2 type 1 receptor blockers
What are som eof the sytemic methods for fixing ypertension
Alpha-adrenoceptor antagonist causes vasodialation
Other drugs result in dialation
Ace inhbitors
Angiotensin II receptor blocers
Ca+ channel blcoekrs
Direcet acting arterial dialators (hydralazine)
Treating SVR is usually in combination with treating volume issues
What is the ACD regime for therapeutic interventions
AT1 blockatesace in hbitors
Calcium channel blclocker
Diuretics
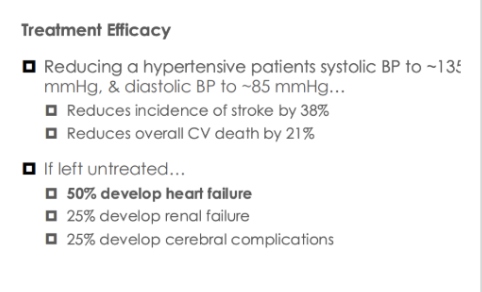
What are trends in treatnemnt efficacy and what is the mortality and compliccation rates for those untreated
Waht is the NTS
nucleus tractus solitarius.
afferent fibers from erhiperal baroreceptors and chemoreceptors and resporatory stretch receptors enter here.
inhibitory interneurons within here project ot the medulala regions to cut back on sympathetic nerves
enhanses vagal efferent nerve activyt
recives inmput fromt he hypothatlamus
What is the DVN and NA
dorsal vagal nuceus and nucleus ambiguus
parasympathetic vagal fibers innervating the heart originate from cell boides found here (medulla of the bbrainstem)
reduces sa nodal firing and slwos the av nodal conduction (agal tone)
Describe the valsalva manuver
reflective test that involves holding your broeath
increasses the pressure i nthe thoractic cavity = increased pressure in the thoractic vessels = increased aortic copmpression = increased aortic pressure
results in bradycardia due to barroreceptor stimulation (parasympathetic
What are teh effects of low does epinephrine and norepinephrine in the body
low does E
increases systolic and diastolic pressure. increases heart rate and areterial puls pressure. very little chagne in map (because they bind to b1 andrenoreceptors = cardiac stimulation)
b2 receptors = sytemic vasodialation
map does not chagnge mych bc cardiac output is offset from teh decrese in systemicvascur resistance
Norepinephrine (low doese)
increase ma and areterial puls pressure. hr increases as well (B1 adrenogenic stimulation)
decreases due to barroreceptor reffelx. map increases due to a1 andronorecpeotrs = increases svr
Where does PNS activity manafest in the vasculature. ACH and others
ACH- induced direct vasodialation (genetals)
Indirect vasodialation by stimulating production vasodialtory substances in the GI circulation
HOw do parasympathetics synapse to their target tissues
they project from the cns directlu to the area (pre and post ganglionic cells)
Why are beta 2 vasodialtory in the vasculature but not in the heart
increases camp production. Camp production is vasodialtory in the blood vessles
camp improces cont3raction in the heart - increases hr and contractility