Homeostasis Topic 23
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
49 Terms
Define Homeostasis
maintaining a constant internal environment
Describe blood pH in terms of homeostasis
- Blood pH is regulated between 7.35 - 7.45
- If pH is too high or too low, enzymes may become denatured
- Hydrogen bonds that hold the tertiary structure together can be broken changing active site shape so less ES complexes form so less efficient metabolic reactions take place
Describe core temperature in terms of homeostasis
- If temp is too low, hypothermia begins
- If temp too high hyperthermia begins
Too high temp
- Enzymes may become denatured
- Hydrogen bonds that hold the tertiary structure together can be broken changing active site shape so less ES complexes form so less efficient metabolic reactions take place
Explain why high blood glucose conc is potentially dangerous
- Hyperglycaemia
- Glucose affects water potential of the blood
- If BGC is too high then the WP falls and water enters the bloodstream from tissues
- This increases blood pressure and dehydrates important organs
Explain why low blood glucose conc is potentially dangerous
- Hypoglycaemia
- It is a main respiratory substrate so is important to maintain sufficient glucose levels to maintain respiration in cells
Define negative feedback
change from a set point and this brings about physiological mechanisms to return to the set point
(results in negative feedback loops)
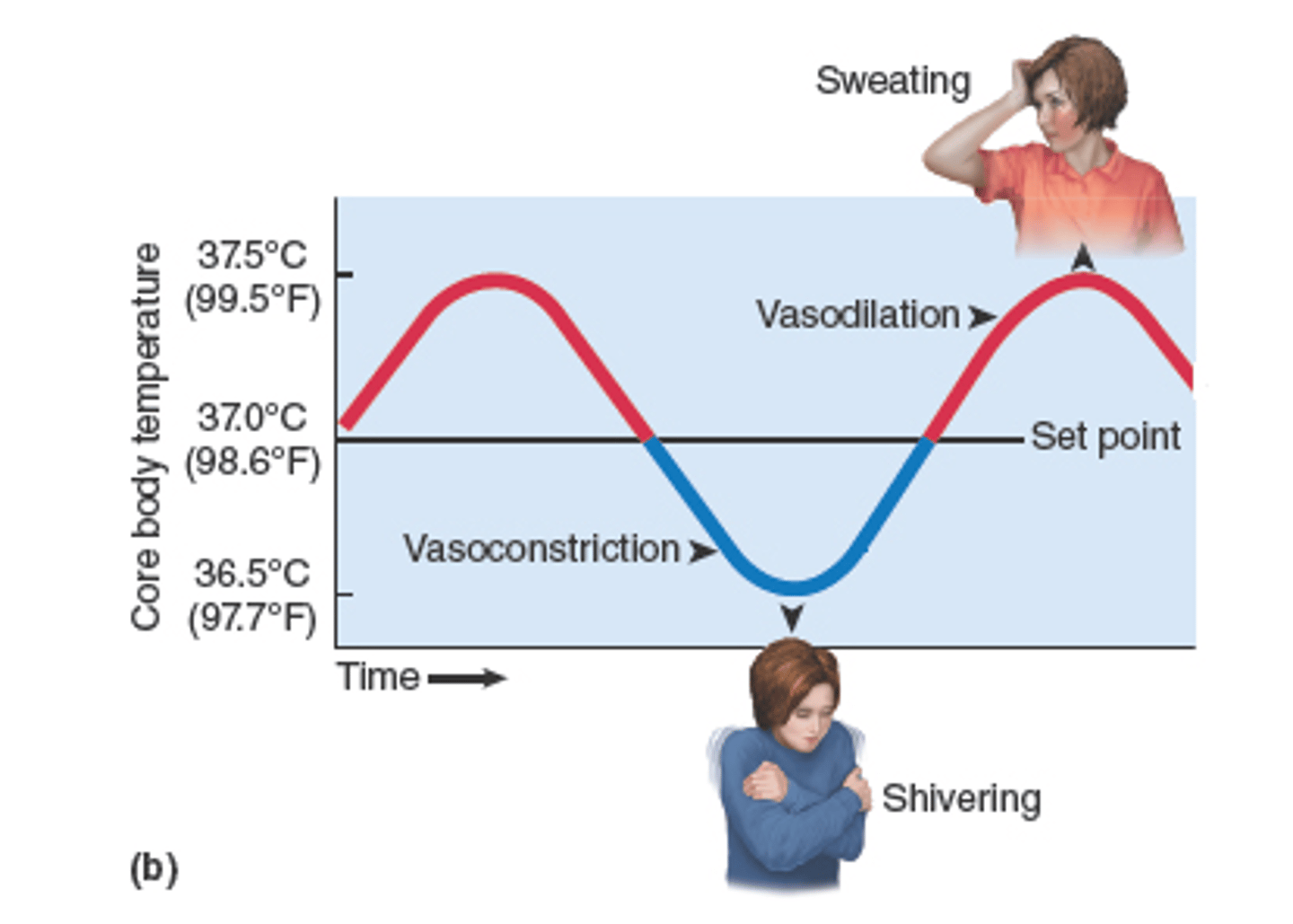
Define positive feedback
- Not a homeostatic mechanism
- Any change away from the norm creates more change
- eg if body temp falls from 37 to 35, the temp continues to drop further
What are the 3 sources of blood glucose?
1) Directly from the diet - in the form glucose from carbohydrates eg starch, maltose
2) From the hydrolysis of glycogen stored in the liver and muscles - glycogenolysis
3) From gluconeogenesis - production of glucose from amino acids / glycerol in the liver (non carb sources)
Define Glycogenolysis
Hydrolysis of glycogen stored in the muscles and liver to produce glucose
Define Gluconeogenesis
Formation of glucose from amino acids / glycerol in the liver (non carb sources)
Describe how changes in blood glucose levels are detected
- Pancreas contains tissue called the Islets of Langerhans which contain receptors that are sensitive to BGC
- Control of blood glucose involves 2 types of islet cells
- a cells - produce the protein hormone glucagon in response to low BGC
- b cells - produce the protein hormone insulin in response to high BGC
Describe Hormonal action
- Hormones are produced by endocrine glands
- They are transported in the blood to target cells in different organs
- They have specific receptor proteins in the plasma membrane or cytoplasm
- Receptor proteins are specific due to the specific tertiary structure that only binds to a hormone of complementary shape (specific binding site)
Describe what happens after a meal to BGC
- BGC will be above normal
- This is detected by b cells
- They secrete insulin
- Travels to target cells - mainly liver and muscles
- Insulin binds to specific receptors on target cell membrane and activates enzymes
How does insulin reduce BGC?
1) Increases uptake of glucose by cells - glucose usually enters by facilitated diffusion through specific channel proteins. Extra channel proteins are present in the cytoplasm which insulin causes them to be added to the cell membrane increasing permeability
2) Insulin activates enzymes that convert glucose to glycogen in liver and muscle cells for storage - glycogenesis
3) Insulin activates enzymes which convert glucose to fats for storage in adipose tissue
4) Increases respiration rate of cells
Describe what happens when BGC falls
- Islets of Langerhans detect fall in BGC the a cells release glucagon
- Bind to liver and muscle cells
- Binds to specific receptor protein on the target cell membrane
How does glucagon increase BGC?
- Activates enzymes that convert glycogen into glucose - glycogenolysis
- Activates enzymes that convert amino acids / glycerol to glucose - gluconeogenesis
Describe the role of adrenaline
- It is secreted from the adrenal glands when BGC and low, during stress and exercise
- Adrenaline binds to receptors on the cell membrane of the liver
This increases BGC by:
- Activating an enzyme that converts glycogen into glucose - glycogenolysis
- INactivates an enzyme that synthesises glycogen from glucose
- Glucose passes into the blood to raise BGC
Describe the second messenger model of hormone action for adrenaline
- Mechanism for glycogenolysis (glucagon and adrenaline act with second messenger model)
1) Adrenaline approaches complementary receptor site on liver
2) Adrenaline attaches to receptor site which activates the enzyme adenylate cyclase inside the membrane
3) Activated adenylate cyclase converts ATP to cyclic AMP (cAMP) which acts as the second messenger that activates protein kinase A
4) Protein kinase A activates a chain of reaction to break down glycogen into glucose (glycogenolysis)
Describe diabetes mellitus
- Body is no longer able to control BGC effectively
There are 2 main types
- Type 1 - inability to produce insulin
Usually appears in childhood, autoimmune response, BGC stay high for a long period of time after eating - the hyperglycaemia can be fatal, some glucose in urine
BGC monitored regularly by biosensor, insulin injections
- Type 2 - insulin independent / late onset
Due to gradual loss in responsiveness of target cells to insulin, linked with obesity, risk factors - {age, lack of exercise, poor diet}
Treated by careful diet regulation, losing weight may be advised
Why can't insulin be taken orally in tablet form?
- It is a protein and so will be hydrolysed in the stomach and small intestine by proteases / low pH of the stomach
What are the functions of the kidneys?
2 main functions -
1) Excretion - filtration of the blood to remove urea (urea made in liver)
2) Osmoregulation - kidneys maintain the blood at a constant water potential despite wide variations in salt and water intake (homeostasis example)
Kidney diagram

What are the 3 main regions of the kidney
1) Outer cortex
2) Medulla - region in the middle and is organised into renal pyramids
3) The pelvis - drains urine into the ureter
Nephron diagram
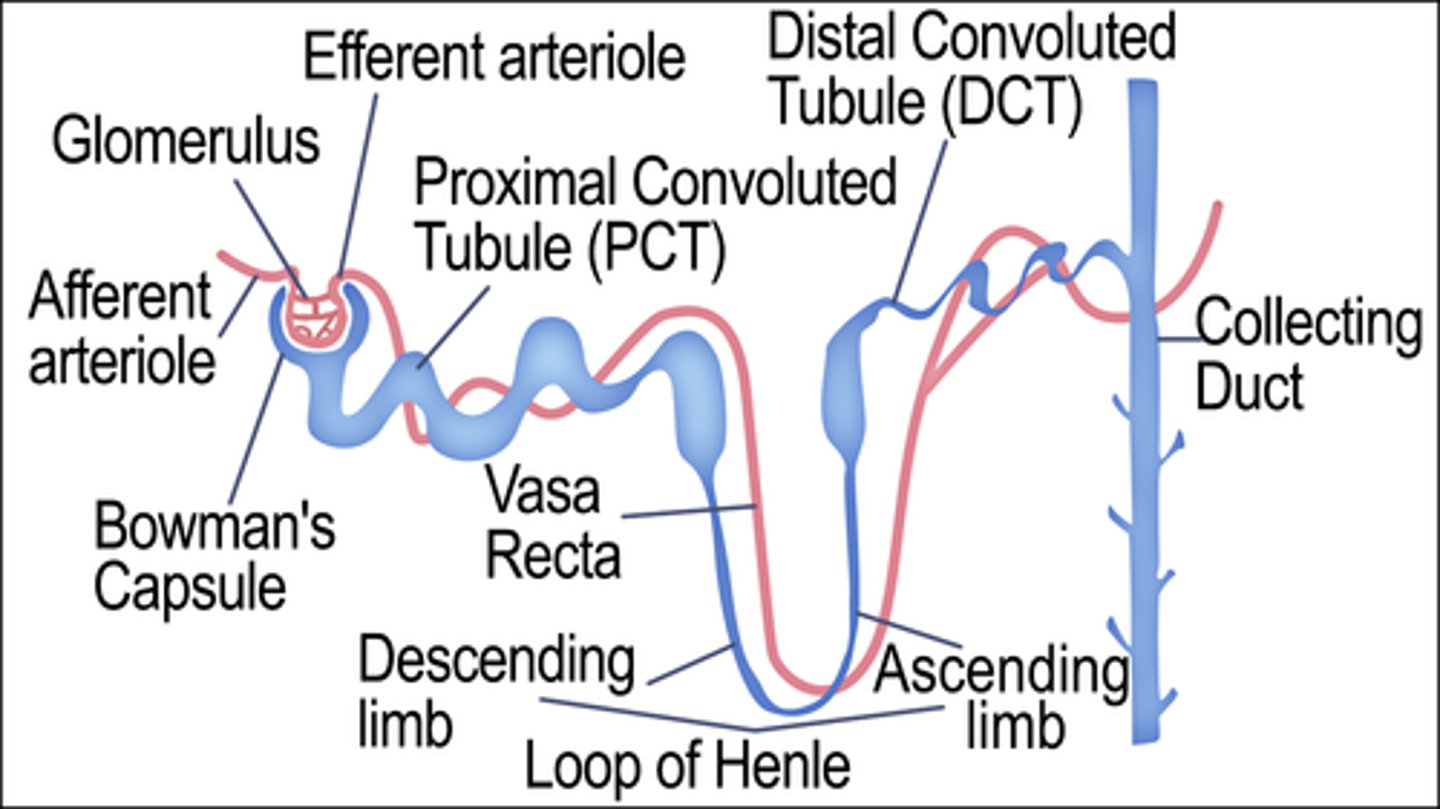
Describe the structure of a nephron
- Starts with Bowman's capsule which contains the knot of blood capillaries called the glomerulus
- Blood brought into glomerulus via afferent arteriole and leaves via efferent arteriole
- Afferent is wider than efferent arteriole
- The proximal convoluted tubule is next then the loop of henle (LoH produces concentrated urine)
- Returns to distal convoluted tubule then to the collection duct
- Urine passes from here through the pelvis of the kidney to the ureter and finally to the bladder
What are the layers of the glomerulus?
- Capillary endothelial cells
- Basement membrane
- Podocytes
Describe podocytes
- Have many finger like processes that interdigitate / close together and wrap around the capillaries making up the glomerulus
- Forms tiny filtration slits
Describe basement membrane
- Between capillaries and podocytes
- Mesh of fibres
- Very thing and only continuous barrier so acts as a filter
- RBC's, plasma proteins and platelets too large to pass through
How is the hydrostatic pressure generated in the glomerulus?
- Afferent arteriole is wider than the efferent arteriole
- Creates a bottleneck in the capillaries
- This pushes water and small molecules from the blood in the capillaries of the glomerulus through the endothelial cells, through the basement membrane (filter), through the podocytes filtration slits into the lumen of the bowman's capsule
- This is ULTRAFILTRATION
- Fluid formed is the filtrate and flows from the Bowman's capsule into the PCT
- Filtrate contains water and small molecules eg glucose, urea, sodium ions but no cells or proteins
State 4 things that will be found in the filtrate after ultrafiltration
- Glucose
- Water
- Urea
- Sodium ions
What is reabsorbed by the PCT and how?
- Glucose, water, amino acids, sodium ions
- By combination of active transport and facilitated diffusion
How is the proximal convoluted tubule adapted for reabsorption?
- Microvilli - maximise SA for reabsorption (by active transport and facilitated diffusion) of glucose from PCT
- Many mitochondria - carry out aerobic respiration to provide ATP needed for active transport of sodium ions
Explain the reabsorption of glucose
- Glucose and sodium ions enter the PCT cells together from the filtrate using specific carrier proteins/ by cotransport
- Glucose leaves PCT other side of PCT cell to enter the vasa recta/ bloodstream of efferent arteriole
- Low glucose conc in blood due to ultrafiltration and high conc in PCT cell so glucose enters by facilitated diffusion
- Sodium ions are actively transported out of the PCT cells and into the blood to maintain the conc gradient from the filtrate to the PCT cells so glucose can enter the cells
What happens to the conc of the tissue fluid and loop of henle as you go deeper into the medulla?
- Conc increases further down you go
Describe the processes of the Loop of Henle
- Cells near the top of the ascending limb pump out sodium ions by active transport (near bottom out by diffusion due to conc gradient) but they are impermeable to water so water can't leave. This creates a low water potential in the tissue fluid of the medulla due to high Na+ conc
- Cells of descending limb are highly permeable to water but impermeable to Na+ ions. Water moves out of the descending limb and enters the tissue fluid of the medulla by osmosis. This makes the filtrate more concentrated, lowers wp
- Water in the tissue fluid is reabsorbed by the vasa recta (blood capillaries) by osmosis
- Action of the loop of Henle creates a conc gradient of sodium ions in the medulla, which allows water to be reabsorbed from the collecting ducts
- The deeper in the medulla the loop of Henle goes, the lower the wp is in the medulla
What is the function of the Loop of Henle?
- Create a high Na+ conc so low wp for the collecting duct to pass
Describe the DCT
- Enters DCT after leaving Loop of Henle
- In the cortex
Give an overview to the collecting duct
- Collecting duct drops into the medulla
- Deeper in the medulla is a lower wp so has the potential to move water out of the filtrate by osmosis and be reabsorbed into the vasa recta
Desert animals have as thicker medulla. Explain the advantage of this
- Thicker medulla means longer Loop of Henle
- More Na+ ions pumped out of the ascending limb so higher Na+ conc in the medulla
- More water can be reabsorbed from the loop/ collecting duct by osmosis
Describe ADH and osmoregulation
- Osmoregulation - homeostatic mechanism that controls wp of the blood
- Body maintains wp of the blood by balancing water lost from the body with water uptake from the diet
- ADH is a peptide hormone synthesised in the hypothalamus and stored in the posterior pituitary gland to be released into the bloodstream
- On reaching the CD it acts by using the second messenger model of hormone action
Give ways in which water can be lost from the body
- Egestion
- Sweating
- Evaporation
- Exhalation
- Urination
Describe osmoregulation when the wp falls
- Osmoreceptors in the hypothalamus detect the fall in wp and send nerve impulses to the posterior pituitary gland to release more ADH into the blood
- This travels to the kidney to the CD cells to make them more permeable to water
- As the filtrate move via CD, the low wp of the medulla means water moves out of the CD by osmosis into the medulla then into the blood from the filtrate
- This produces small volume of conc urine - helps conserve water
Describe osmoregulation when the wp increases
- Osmoreceptors in the hypothalamus detect the high wp so send nerve impulses to the posterior pituitary gland to secrete less ADH
- The CD is less permeable to water
- Less water is reabsorbed as it passes down the CD
- Large volumes of dilute urine are produced - helps remove water
How does ADH increase and decrease permeability of the CD?
- ADH increases transcription and insertion of aquaporins into the membranes of the CD cells
- Aquaporins are protein water channels that allow water to move down their wp gradient out into the medulla then into the vasa recta from the filtrate
- When ADH levels fall, aquaporins and removed from the membranes and the collecting ducts are less permeable to water
What symptoms would you expect of a person with a lack of ADH?
- Frequent need to urinate
- Large volumes of dilute urine
- Persistent feeling of thirst
- Mineral imbalance
- Dehydration
Describe what happens when ADH release is inhibited on the volume and conc of urine produced
- Volume of water increases
- Conc decreases
- Collecting duct impermeable to water
- Aquaporins removed from the collecting duct cells
- Less water reabsorbed by the filtrate by osmosis
- Drinking increases liquid intake therefore liquid loss
People with type 2 diabetes don't respond to insulin
Explain how this leads to a reduced ability to regulate BGC
- Less receptors on cell membrane
- Fewer glucose transport proteins
- Less glucose can enter the cells
- Less glucose converted into glycogen
- BGC isn't lowered when high
Exam style
How does insulin reduce BGC?
[- Binds to receptors on the liver / muscles]
- To convert glucose into glycogen / glycogenesis
- BY ACTIVATING ENZYMES
Give a name to Loop of Henle / it's actions
Countercurrent Multiplier