(26-28) Organ Systems: Kidney
1/26
Earn XP
Description and Tags
L26-L28
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
27 Terms
One function of the kidney is the production of hormones/enzymes. List the other 4 functions, and then the 3 hormones/enzymes/enzymatic processes the kidneys produce.
1. Regulation of Water, Salts, Acid-Base balance
2. Removal of metabolic waste
3. Removal of foreign chemicals
4. Gluconeogenesis (formation of glucose)
5. Production of hormones / enzymes
• Erythropoietin (controls red blood cell production)
• Renin (controls blood pressure and sodium balance)
• Activates Vitamin D (regulates calcium)
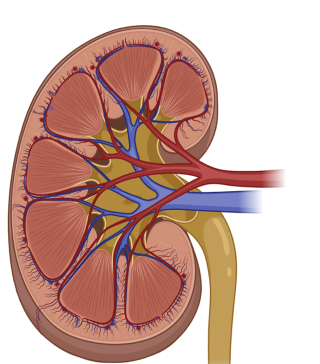
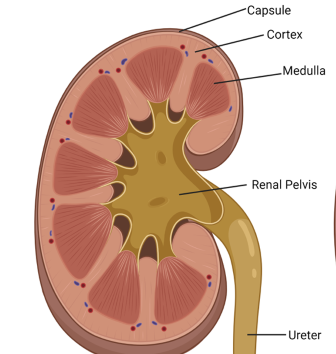
Label the kidney (7 labels)
+
renal vein
renal artery
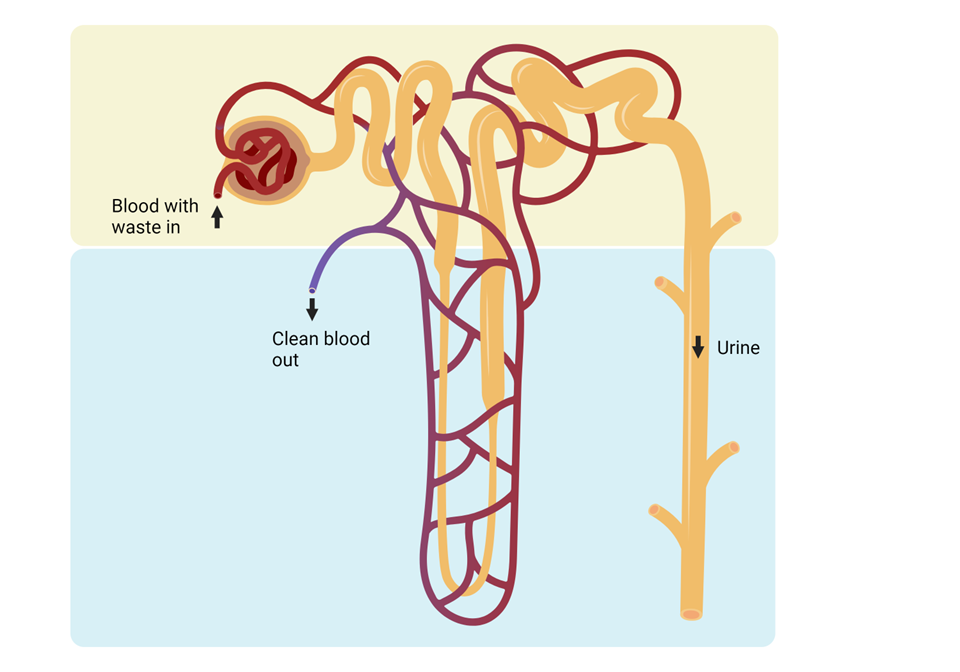
The capillaries surrounding the nephron are called the “peritubular capillaries”, while those surrounding the loop of Henle are specifically called the “vasa recta”.
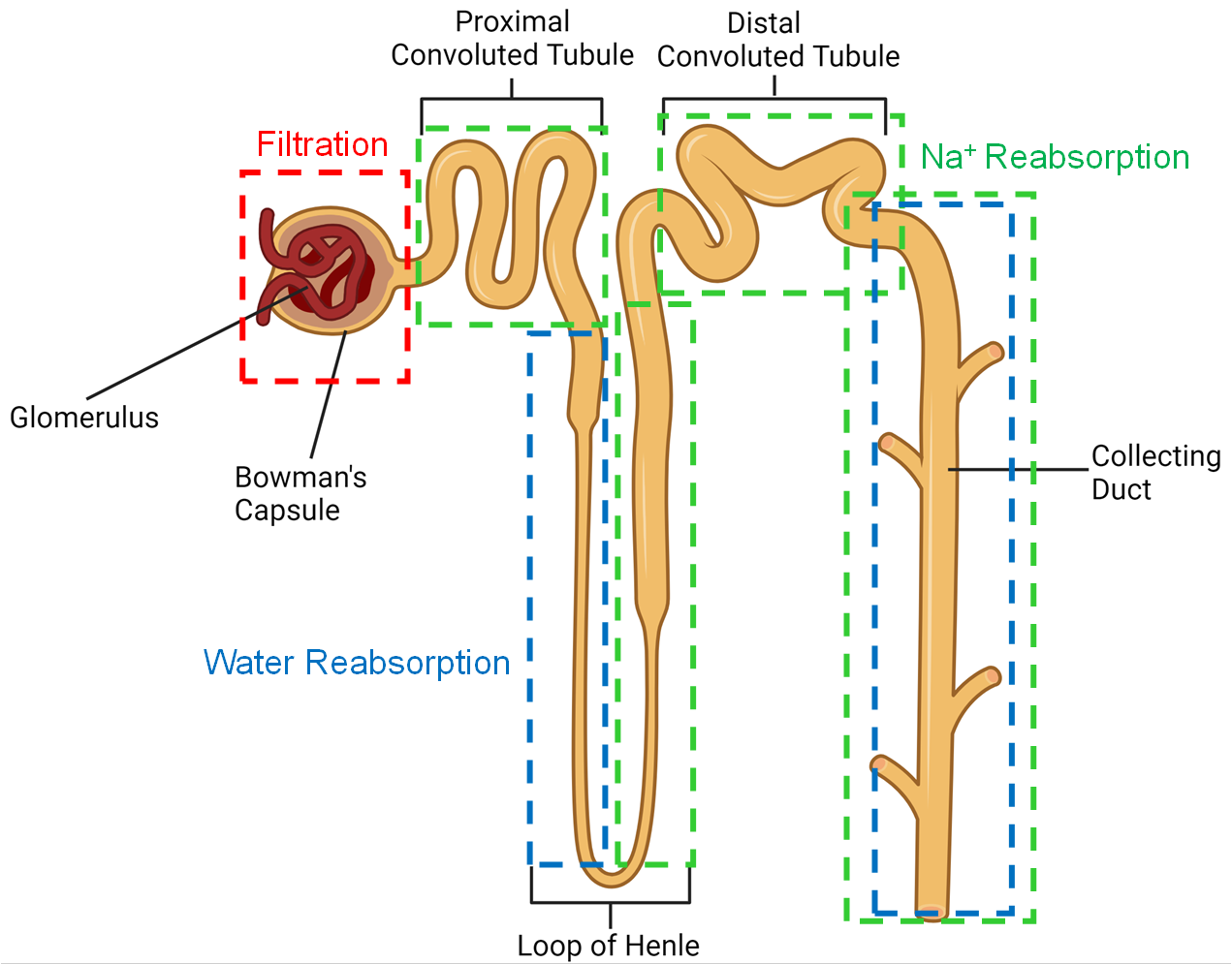
Label all other parts of nephron (6 labels)
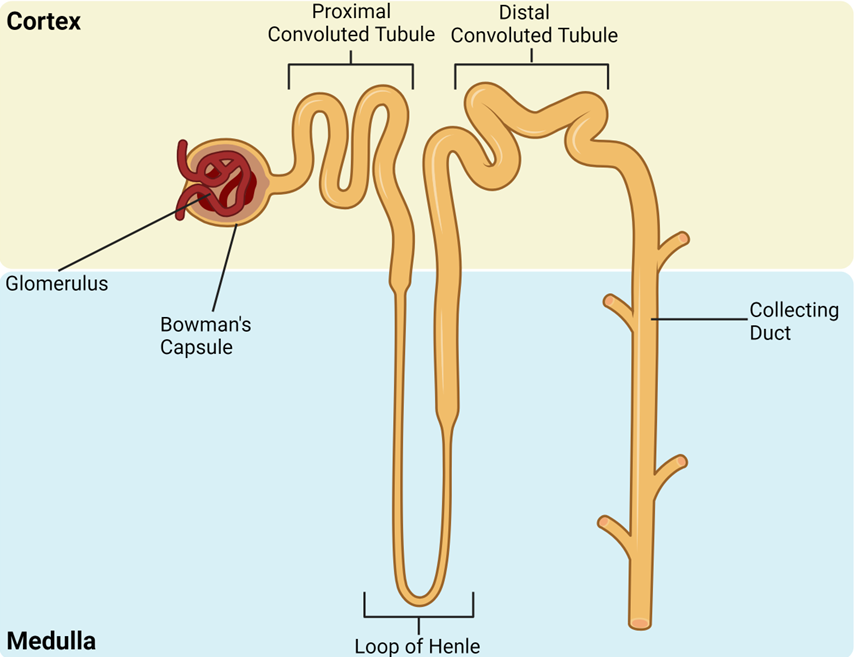
Identify nephron structures in cortex
glomerulus, Bowman’s capsule, proximal & distal convoluted tubules
Identify nephron structures in medulla
loop of Henle & collecting duct
identify 3 main functions/steps to nephron function
glomerular filtration * tubular secretion * tubular reabsorption
Describe the process of glomerular filtration & describe which substances can/(not) pass through
Podocytes surround blood vessels within the glomerulus
Foot-like process create a sieve-like structure
Allows free passage of small molecules from blood to kidney tubules
Define Glomerular Filtration Rate (GFR)
Glomerular Filtration Rate (GFR) - Volume of fluid filtered from glomeruli to bowman’s space per unit time
What causes the flow of fluid through the glomeruli? How is Glomerular Filtration Rate regulated?
Fluid filtered through glomeruli by pressure of flow through blood vessels
GFR regulated by adjusting blood pressure either side of glomerulus
What reduces GFR (by reducing pressure in glomerulus) and what is the effect on water & salt loss/excretion?
Constricting afferent vessels
Dilating efferent vessels
Thus, Lower force pushing substances through
Thus, water and salt loss reduced through excretion
What increases GFR (by increasing pressure in glomerulus) and what is the effect on water & salt loss/excretion?
Constricting efferent vessels
Dilating afferent vessels
Thus, Greater force pushing substances through
Thus, water and salt loss increased through excretion
What does it mean that capillaries in the glomerulus are “fenestrated”, and what is the purpose of this?
"fenestrated" :- a unique type of capillary that has numerous small poresin their walls, which water and small solute molecules to pass into Bowman's capsule, while blocking larger components (like blood cells)
What is the largest size a substance can be to pass into Bowman’s capsule (in nm), and describe the selectivity of this.
Allows free passage of small molecules (<8nm) from blood to kidney tubules;
Removes based on size, regardless of if it should or should not remove from body
Causes useful substances to be lost in filtrate, along with intended toxic metabolites
Proteins (& drugs bound to proteins) cannot pass through, and are retained in the blood
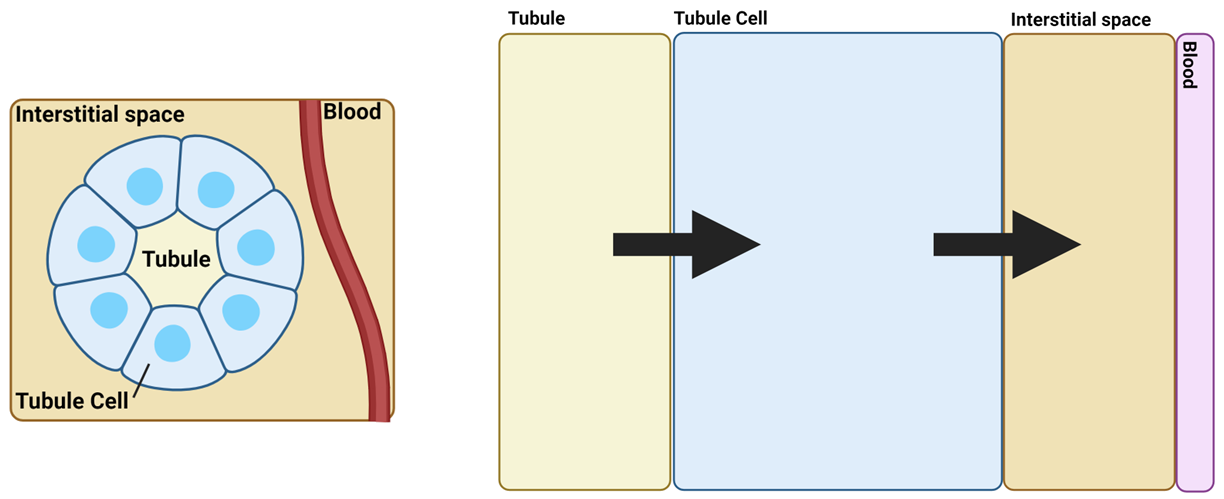
which side of the tubule cell is the apical vs. the basolateral
Arrow 1 - apical surface
Arrow 2 - basolateral surface
Describe the two mechanisms by which Na+ is reabsorbed through the apical surface of the tubule cell, in the proximal convoluted tubule. (2 mechanisms)
Co-transport (X) with other molecules. E.g. Glucose
Everything moves the same way
Counter-transport of Hydrogen ions (Na+ in , H+ out)
Substances moving in diff. directions
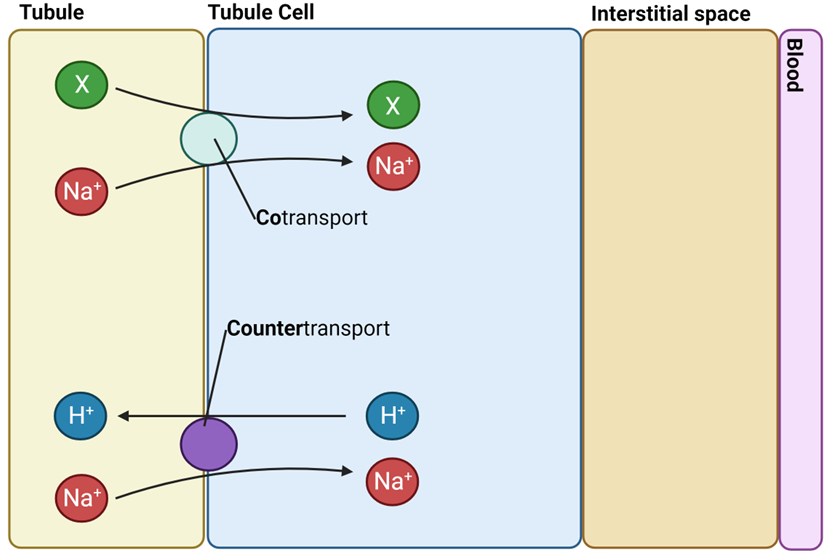
Differntiate between co-transport & counter-transpprt
co: substances leave cell tg
counter: substances go opposite ways
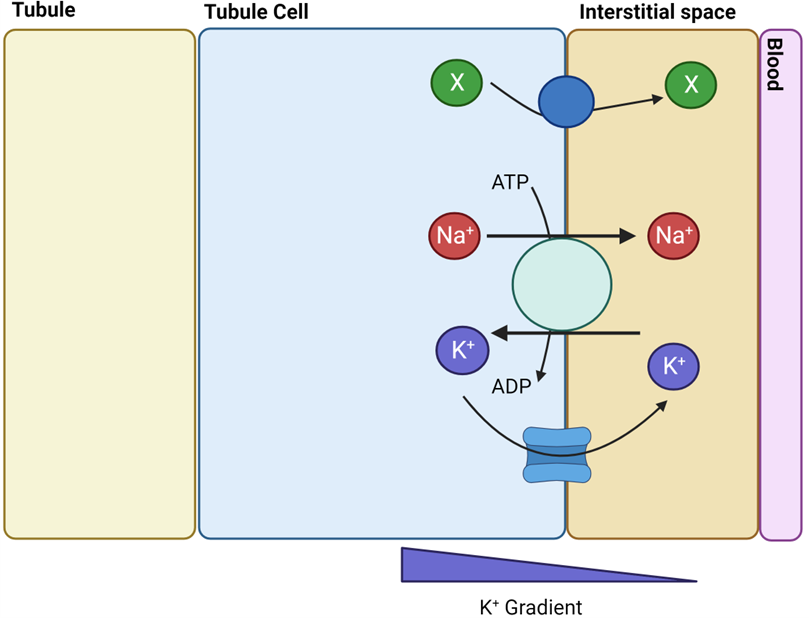
Describe the mechanism by which Na+ is reabsorbed through the basolateral surface of the tubule cell, and other previously co-trasnported substances, in the proximal convoluted tubule.
Na+ moved from cells to interstitial space and then blood via active transport
Na+/K+ ATPase pump, requires ATP
K+ returns to interstitial fluid via K+ specific ion channels
Down concentration gradient
Co-transported molecules (X) moved specific transporters (e.g Glucose-specific transporters via glucose transporters)
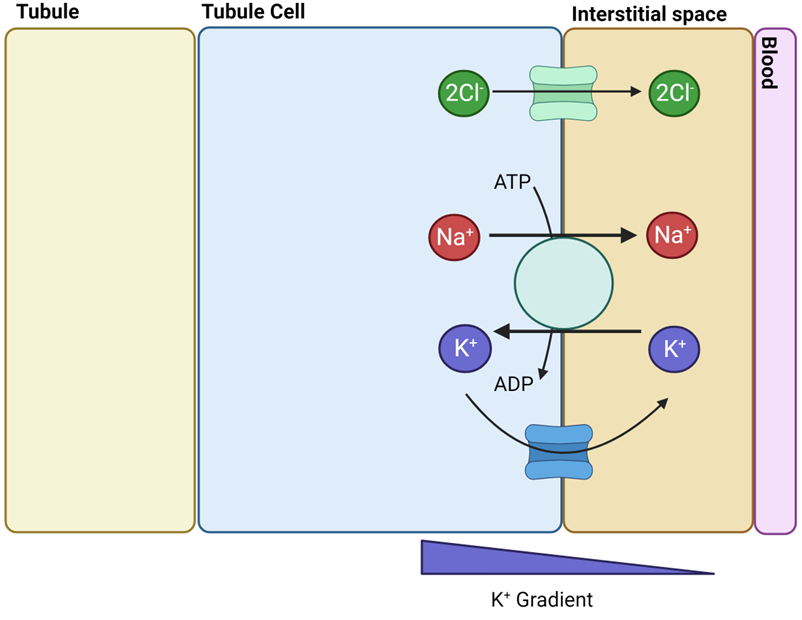
Describe the mechanisms by which Na+ is reabsorbed through the apical surface of the tubule cell, in the ascending loop of Henle.
Na+ moved from tubules into cells through cotransport with K+ and Cl-
Na-K-Cl cotransporter (NKCC)
K+ moves back into tubule via ion channels
Down concentration gradient
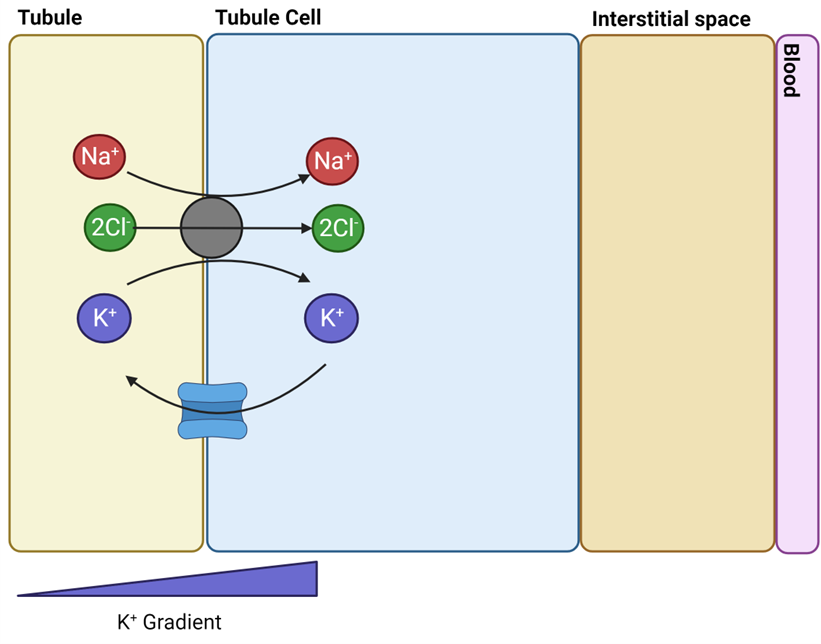
Describe the mechanisms by which Na+ is reabsorbed through the basolateral surface of the tubule cell, in the ascending loop of Henle.
Na+/K+ ATPase moves Na+ out to interstitial space and K+ into cells
K+ returns to interstitial fluid via K+ specific ion channels
Down concentration gradient
Cl- returns to interstitial fluid via Cl- specific ion channels
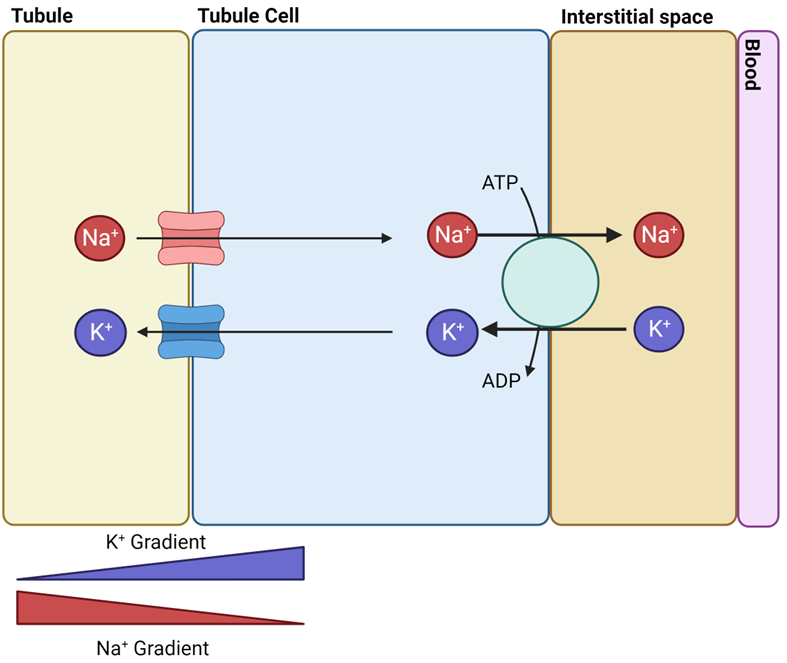
Describe the mechanisms by which Na+ is reabsorbed through the apical & basolateral surfaces of the tubule cell, in the collectng duct.
Tube – Cell (Apical Surface)
Channels specific to Na+ & K+ each individually present
Na+ moves into cell and K+ moves out through ion channel
Down concentration gradient
Cell – Body (Basolateral Surface):
Na+/K+ ATPase moves Na+ out to interstitial space and K+ into cells
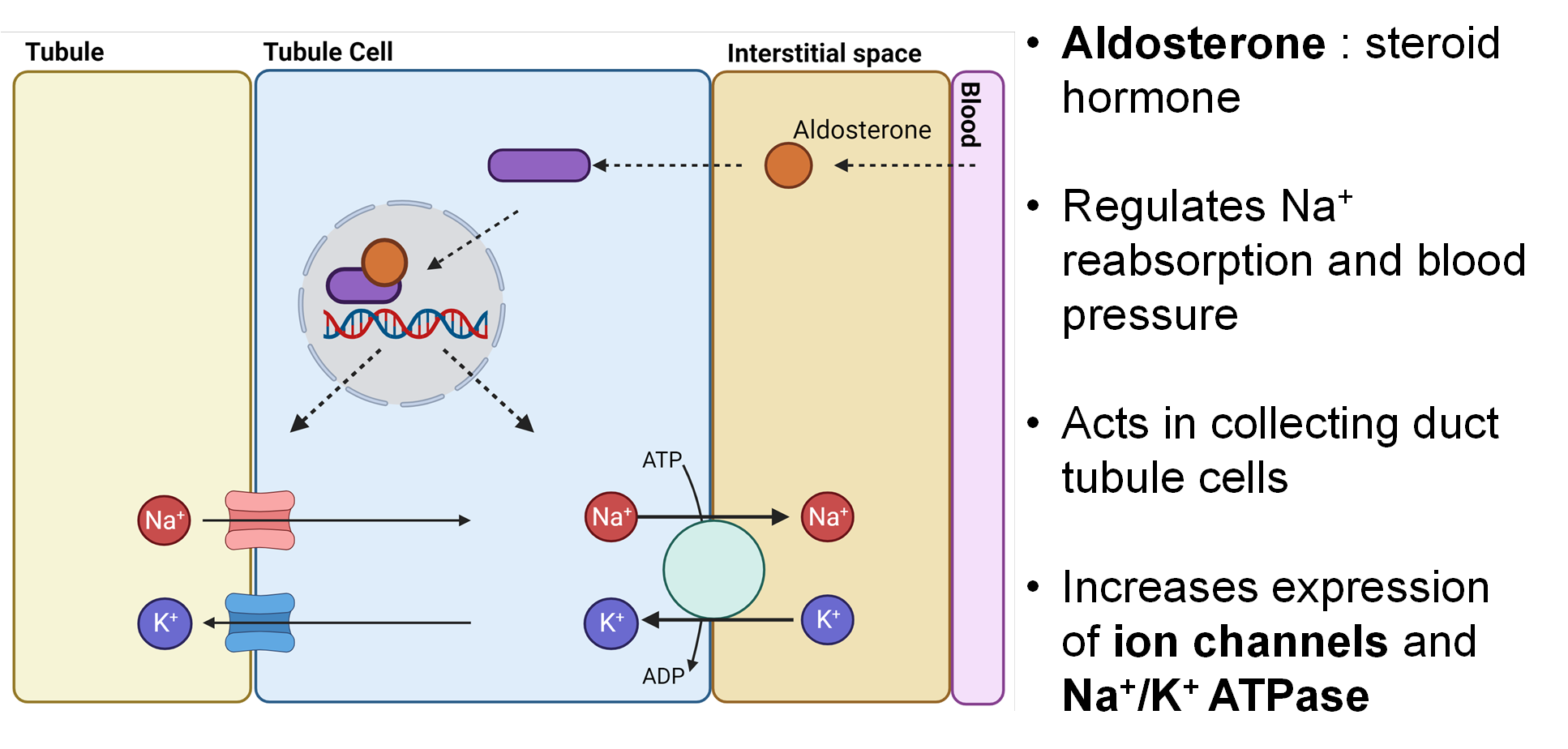
What hormone acts on the collecting duct to regulate Na+ reabsorption? Describe the mechanism.
Aldosterone : steroid hormone
Acts on nuclear receptors
Regulates Na+ reabsorption and blood pressure
Acts in collecting duct tubule cells
Increases expression of Na+ & K+ ion channels and Na+/K+ ATPase
Since there are more channels/pumps, there is higher reabsorption
Since it takes time to synthesize more proteins, etc. (other cellular processes), this process take time
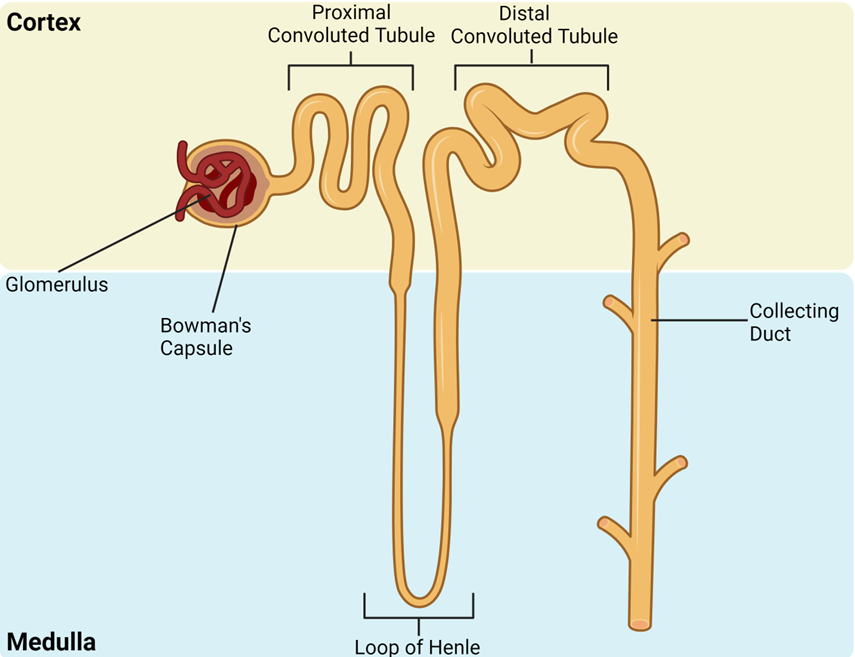
Identify the areas of the nephron involved in: filtration, Na+ reabsorption, Water reabsorption
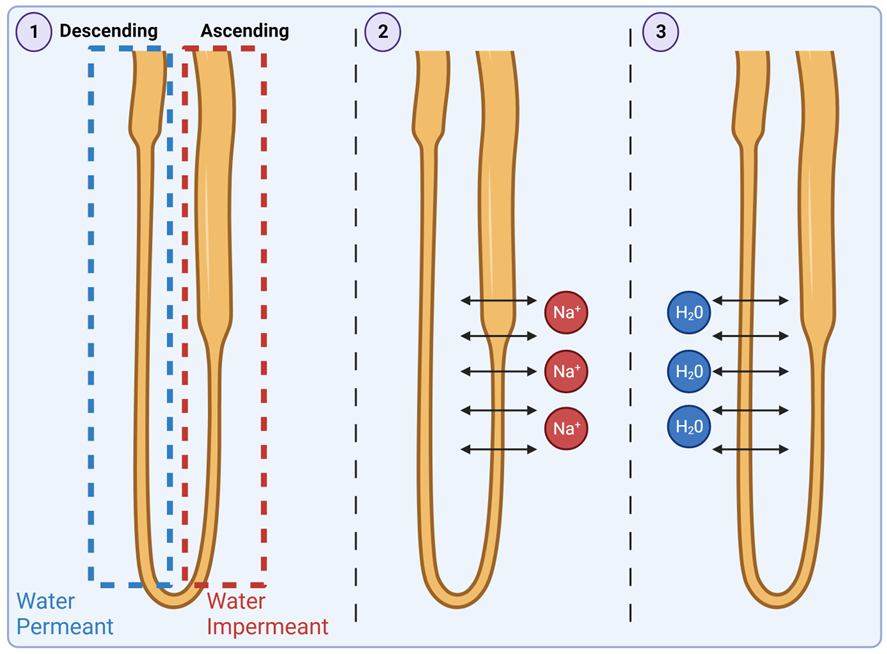
Describe the mechanisms by which water is reabsorbed, in the descending loop of Henle? (Must hit all points in the answer, extra points for illustrating w/ diagram)
1. Only descending loop permeant (permeable) to water (i.e. water cannot exit ascending tubule)
2. Ascending ↑ loop releases salts, which become reabsorbed by interstitial fluid/blood – creating hypertonic solution (higher salt conc.) in interstitial fluid around loop
3. This hypertonic interstitial fluid causes water to diffuse out of descending loop
• Blood flow around loop of Henle is counter to flow through loop of Henle.
• Freshly filtered blood (low in salt) first encounters ascending loop of Henle (pumping out salt)
• Encourages salt absorption
• This salt-rich blood then circulates around descending loop
• Water from descending loop moves into blood
• Maintains concentration gradients
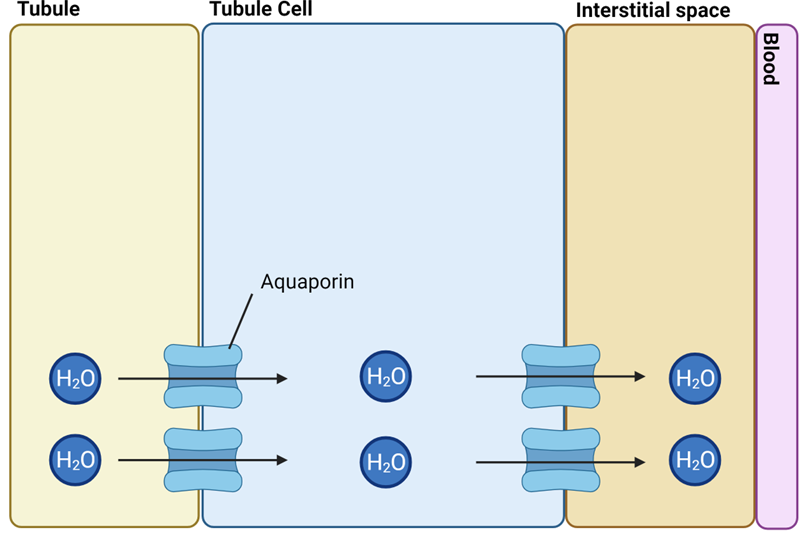
Describe the mechanisms by which water is reabsorbed, in the collecting duct? (Must hit all points in the answer)
• Collecting duct tubule cells contain lots of water channels (Aquaporins)
• Interstitial space full of salt from Na+ reabsorption
• Allows free flow of water out of tubule, through cell, and into interstitial space
What hormone acts on the collecting duct to regulate water reabsorption? Describe the mechanism.
Vasopressin: hormone that controls water reabsorption
Acts on receptors on collecting duct cells
This causes aquaporin-rich vesicles inside cell to fuse with cell membrane
Thus delivering aquaporins to apical cell surface
Increases number of channels water can use to cross into body
Thus more water absorption into blood
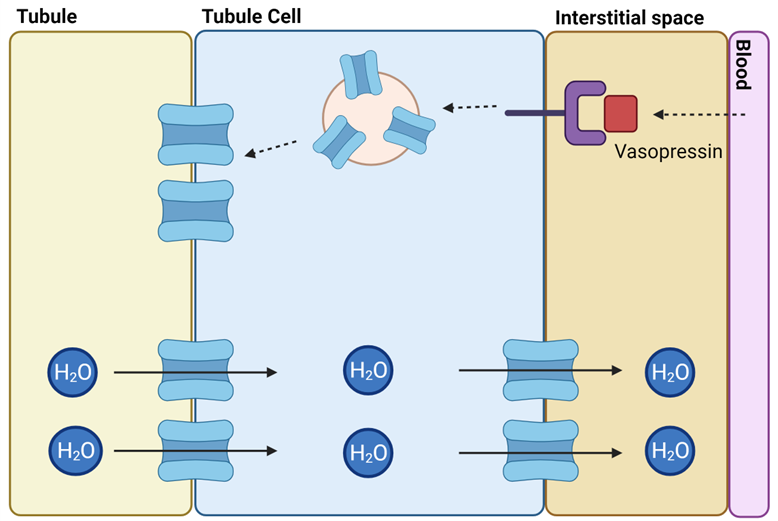
Identify the key distinctions between with aldosterone vs. vasopressin?
In aldosterone, action takes hours as more transport proteins need to be synthesised
With vasopressin, action takes minutes as aquaporins are already present in vesicles