Chapter 10 Muscle Fibers
1/82
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
83 Terms
Functions of Muscle
Body movement
Maintinance of posture and body position
Potection and support
Storage and movement of materials
heat production
Types of muscles ( where found too and differences between them)
Skeletal- Striated , long, multi nucleated, all voluntary muscles
Cardiac- Striated, short, usually one nucleus, heart only
smooth- not striated, tapered at ends Hollow organs and blood vessels
Properties of muscle Cells
▪ Excitability – ability to respond to stimuli
▪ Conductivity – ability to conduct electrical changes
across entire plasma membrane
▪ Contractility – contractile proteins in cells draw closer
together
▪ Extensibility – ability to be stretched without rupturing
▪ Elasticity – ability to return to original length after
stretching
Skeletal Muscles are made of:
Muscle fibers (myocytes)
Blood vessels
Nerves
Connective tissues
Connective tissues of Skeletal Muscles Function
(1) anchor, (2) separate, (3) organize, and (4) electrically
insulate
Connective Tissues Found on Skeletal Muscles
• Epimysium
• Perimysium
• Endomysium
Tendon
• Aponeurosis
Epimysium
layer of CT surrounding entire muscle
Perimysium
Layer of CT surrounding fascicles (bundle of nerves or muscles)
Endomysium
Layer of CT surrounding each muscle fiber
Tendon
Cord like strand of dense regular CT that attaches muscles to bones
Aponeurosis
Wide flat white sheet of CT that attaches neighboring muscles to bone or other muscles
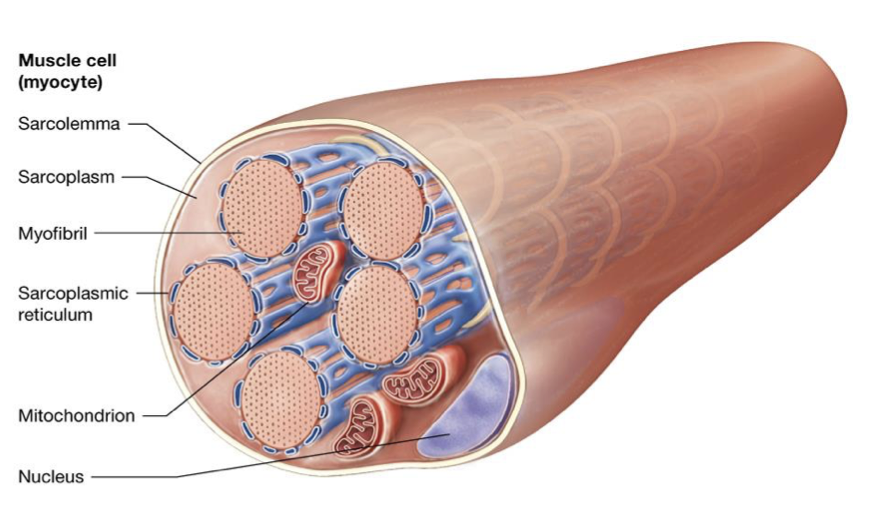
Skeletal Muscle Fiber general shape
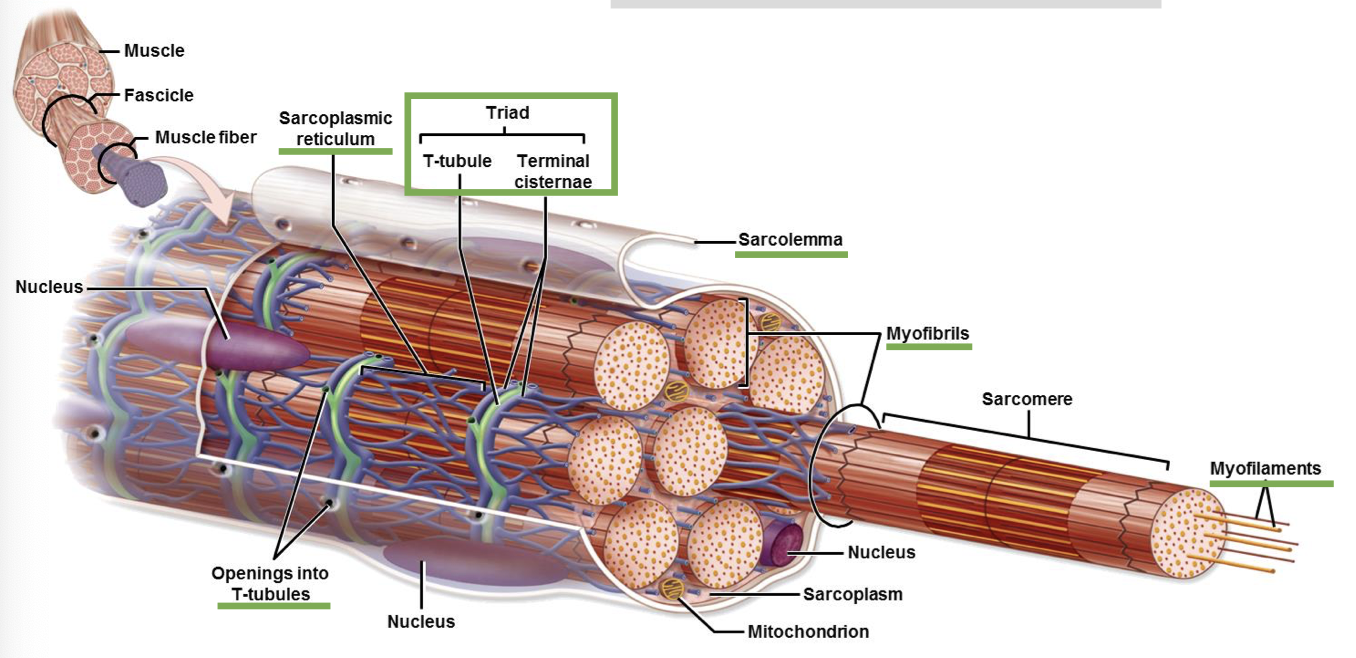
Skeletal Muscle Fiber with Triad general outline
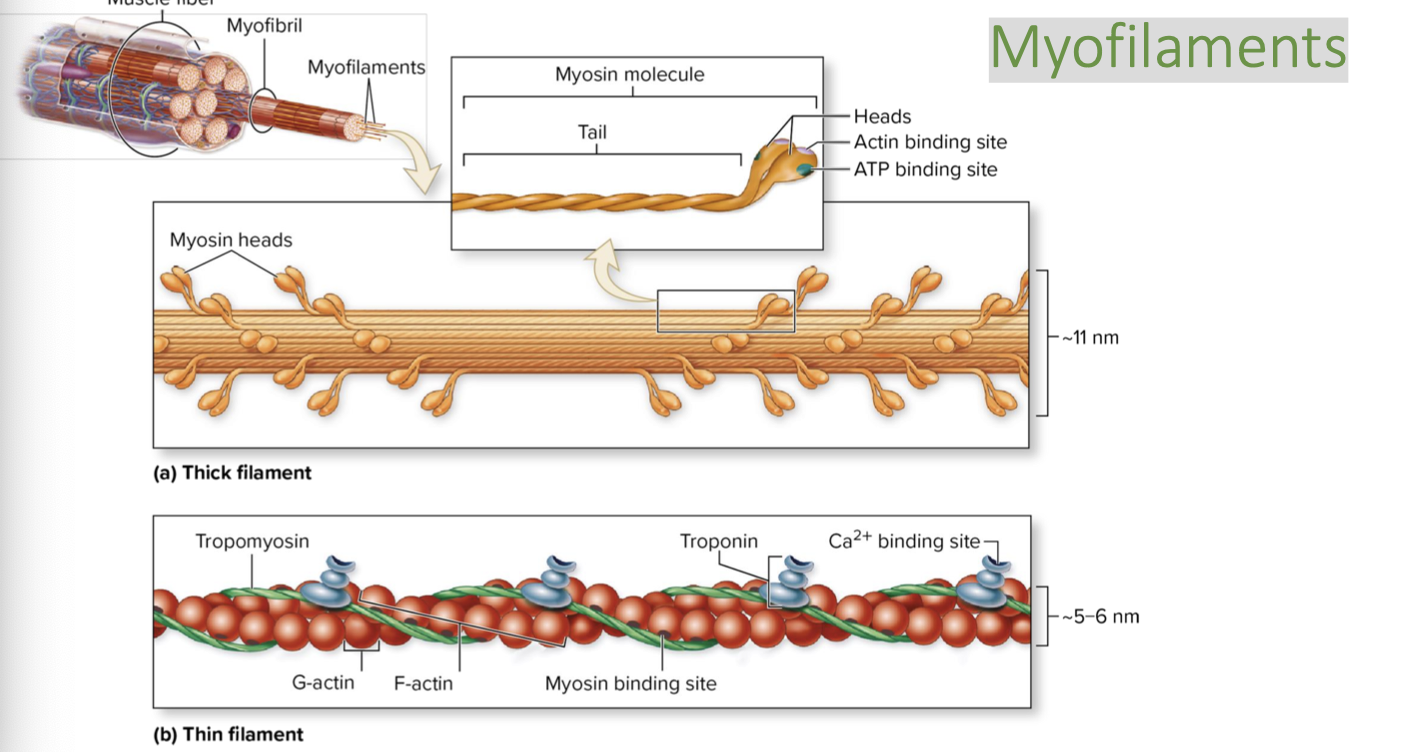
Myofilaments shape (image)
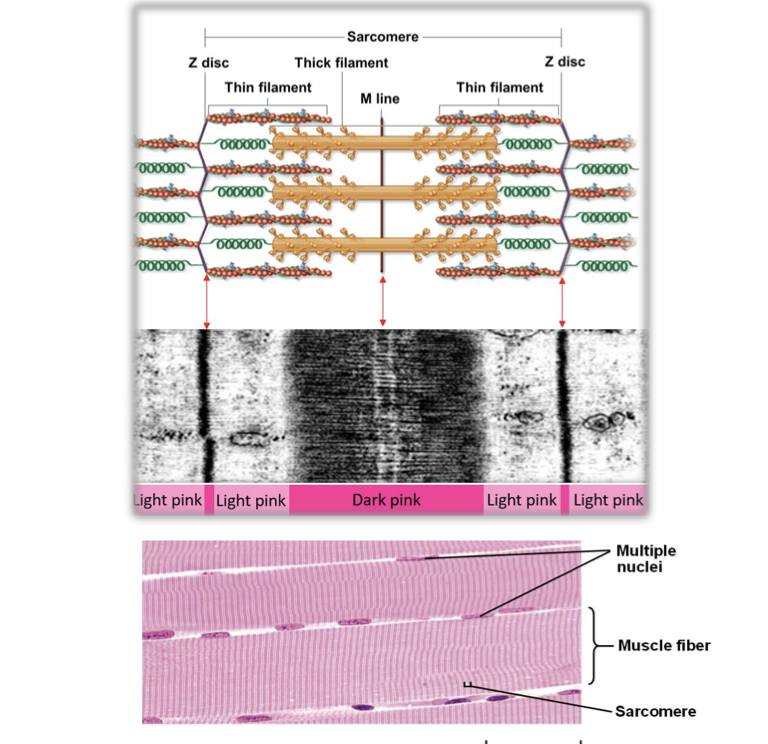
Sarcomere image
Sarcolemma
the plasma membrane; the fine transparent tubular sheath which envelops
the myofibers
Sarcoplasm
the cytoplasm; contains the organelles
Transverse Tubules (T-Tubules)
inward extensions of the sarcolemma; surrounds myofibril
organelles and forms a tunnel-like network through which extracellular fluid flows
Myofibril
long cylindrical bundle of proteins specialized for contraction (myofilaments);
most abundant organelle
Sarcoplasmic Reticulum
modified web-like smooth ER; stores Ca2+ ions; contains end sacs
called terminal cisternae
Myofilaments
two contractile protein filaments that make up myofibrils; known as thin and
thick filaments
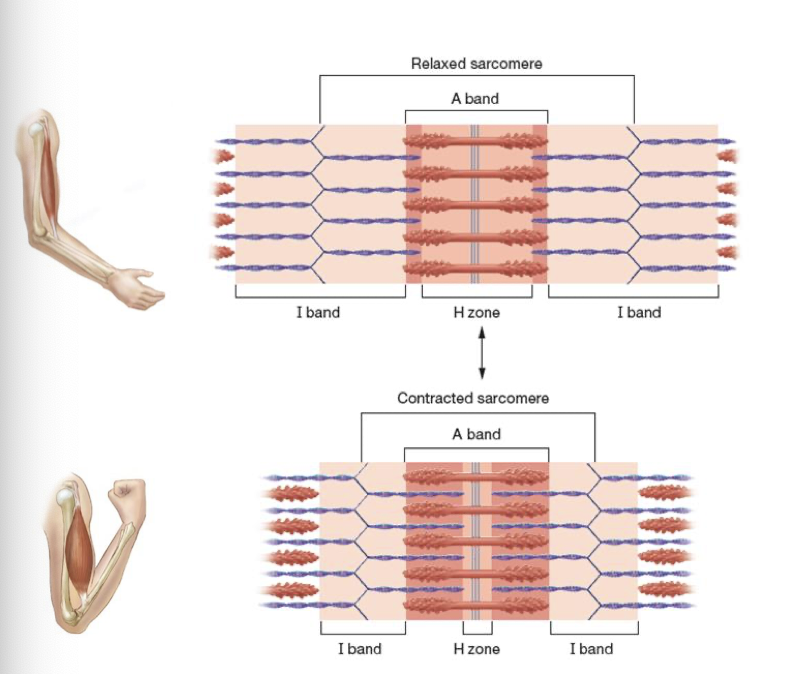
Sarcomere
structural unit of muscle contraction; composed of alternating thin and thick
filaments
Motor Unit image
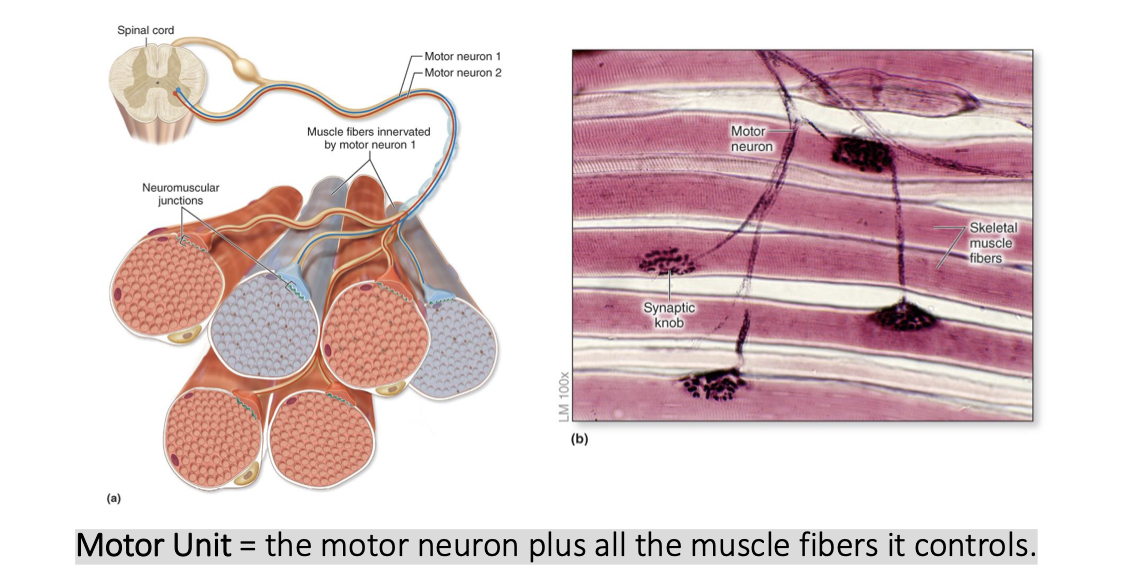
Motor Unit
Motor Unit = the motor neuron plus all the muscle fibers it controls.
A motor neuron is a cell from the nervous system that transmits a signal from the brain or spinal cord to tell
the muscle fiber to contract.
Neuromuscular Junction (NMJ)
Where the motor neuron and muscle fiber meet.
Parts:
▪ Axon terminal: end of the motor neuron; contains
vesicles filled with Acetylcholine (ACh)
▪ Synaptic cleft: small space b/n motor neuron and
muscle cell
▪ Motor end plate: folded surface of the muscle cell
directly under the synaptic cleft
Skeletal Muscle Fiber Contraction
Myosin and actin want each other
(can’t get together because of
tropomyosin and troponin).
Troponin wants Ca++ but Ca++ is
unavailable…
Phase 1 Muscle contraction
Excitation
Action potential arrives at the axon terminal and triggers CA2+ channels in the terminal to open.
CA2 entry triggers exocytosis of synaptic vesicles
Synaptic vesicles release ACh into the synaptic cleft
ACh binds to ligand gated ion channels in the motor end plate
ion channels open and Na enters the muscle fiber
Entry of Na depolarizes the sarcolemma locally, producing Na end-plate potential
Phase 2
Excitation-Contraction Coupling
End plate potential stimulates an action potential
Action potential is propagated down the T tubule
T-Tubule depolarization leads to the opening in calcium channels in the sarcoplasmic reticulum and CA enters the cytosol
Phase 3 of muscle contraction
Contraction
Calcium binds to troponin
Tropomyosin moves and the active site of actin are exposed
Calcium binds to troponin, causing a conformational change in
tropomyosin to expose the myosin binding site on actin.
The myosin heads can bind to actin, forming a cross-bridge
Begin siding filament mechanism of contraction
Sliding filament mechanism of contraction
Sarcomeres are contracted to the A band, bringing z discs closer together
Crossbridge Cycling
▪ ATP bound to myosin is hydrolyzed
causing myosin head to assume
“cocked” position
▪ Myosin head binds to actin forming
cross-bridge
▪ ADP is released resulting in power stroke
▪ New ATP molecule binds to myosin
head, separating the cross-bridge
▪ Cycle starts over
Muscle Relaxation
1. Motor neuron signal ceases
▪ ACh release stops
▪ Acetylcholine esterase degrades remaining ACh in synaptic cleft
▪ Membranes return to resting membrane potential and ion channels close
2. Calcium is actively pumped back into SR
▪ Troponin and tropomyosin return to original conformations
▪ Myosin binding sites are covered
Bacteria which interfere with the muscular contraction control mechanism
Tetanus:
▪ Releases a toxin that interferes with the ability of the CNS to
inhibit unwanted contractions
▪ Results in spastic paralysis → “Lock Jaw”
Botulism:
▪ Releases a toxin that blocks ACh release from synaptic knob
▪ Results in flaccid paralysis of affected muscle
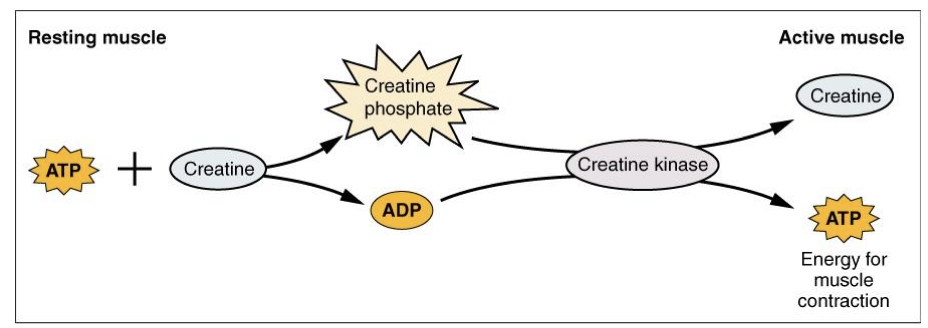
ATP importance in muscular contractions
Required to:
▪ Power Na+/K+ pumps that maintain ion gradients
▪ Release myosin heads
▪ Pump calcium back into SR for muscle relaxation
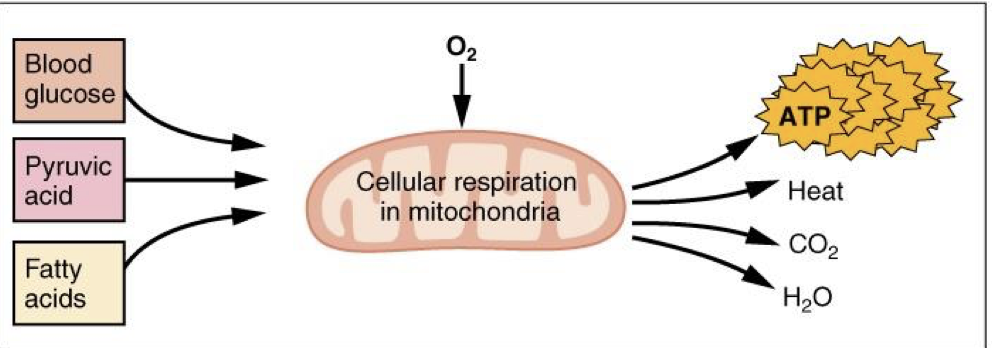
Sources of ATP:
▪ Creatine phosphate metabolism
▪ Anaerobic cellular respiration (glycolysis)
▪ Aerobic cellular respiration
Creatine Phosphate Metabolism
Immediate ATP supply: creatine phosphate can immediately regenerate enough
ATP for about 10 seconds of maximum muscle activity
Anaerobic Cellular Respiration (Glycolysis)
Short-Term ATP Supply: provides energy for muscle contraction once immediate
sources are depleted; can supply ATP for 30-40 seconds of sustained contraction.
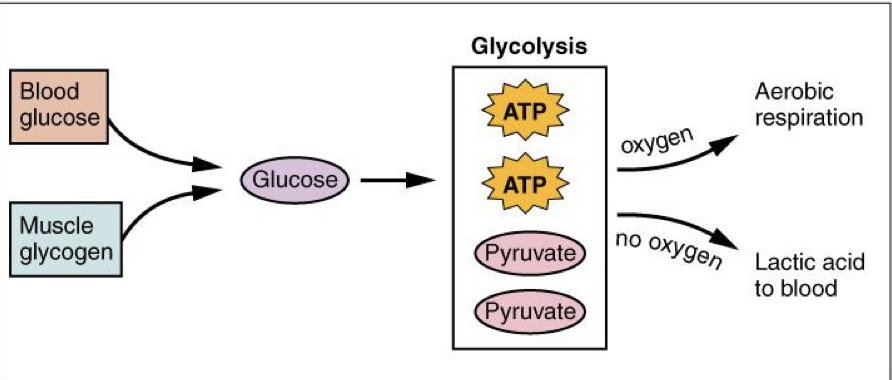
Aerobic Cellular Respiration
Predominant energy source, Long term ATP supply:
allows for longer-lasting muscle contractions (more ATP than glycolysis)
▪ Muscles store small amount of excess oxygen in myoglobin to allow for more efficient muscle contractions and less fatigue
Classes of skeletal muscle
Type 1/ Slow
Type 2/ Fast
Based on Myosin ATPase activity (speed of power stroke)
Type 1 Fibers
Slow oxidative (SO)
▪ Slow, less powerful contractions, but
efficient (Fatigue resistant)
▪ Low myosin ATPase activity
▪ Rely on aerobic respiration
▪ Numerous mitochondria and myoglobin molecules
▪ Well-developed blood supply → “dark muscle”
Type 2 fiber types
Fast oxidative (FO)
Fast Glycolytic (FG)
Fast Oxidative (FO)
▪ Intermediate strength, speed, and fatigability
▪ Moderate blood supply and myoglobin content
▪ “dark muscle”
Fast Glycolytic (FG)
▪ Strongest strength, speed, and fatigability
▪ High glycogen content, little myoglobin and blood supply
▪ “white muscle”
Muscle Tension
The force generated when skeletal muscle is stimulated
Maximum force of contraction can be improved by:
Fast glycolytic fibers
Large motor units
Greater stimulus frequency
Muscles at resting length
Muscle twitch
a single, brief contraction followed by relaxation in response to a single stimulus
Threshold
min. voltage needed to generate twitch
Latent Period
lag time between stimulus and twitch
Contraction period
repetitive power strokes resulting in increased tension in muscle, start of muscle tension to the peak of muscle tension
Relaxation period
Release of cross bridges due to decreasing calcium levels. Where the peak tensions starts to drop to the end of relaxation
Effect of motor unit recruitment on tension
An increase in voltage causes a greater number of motor units to contract,m increasing tension
Effect of stimulus frequency on muscle tension
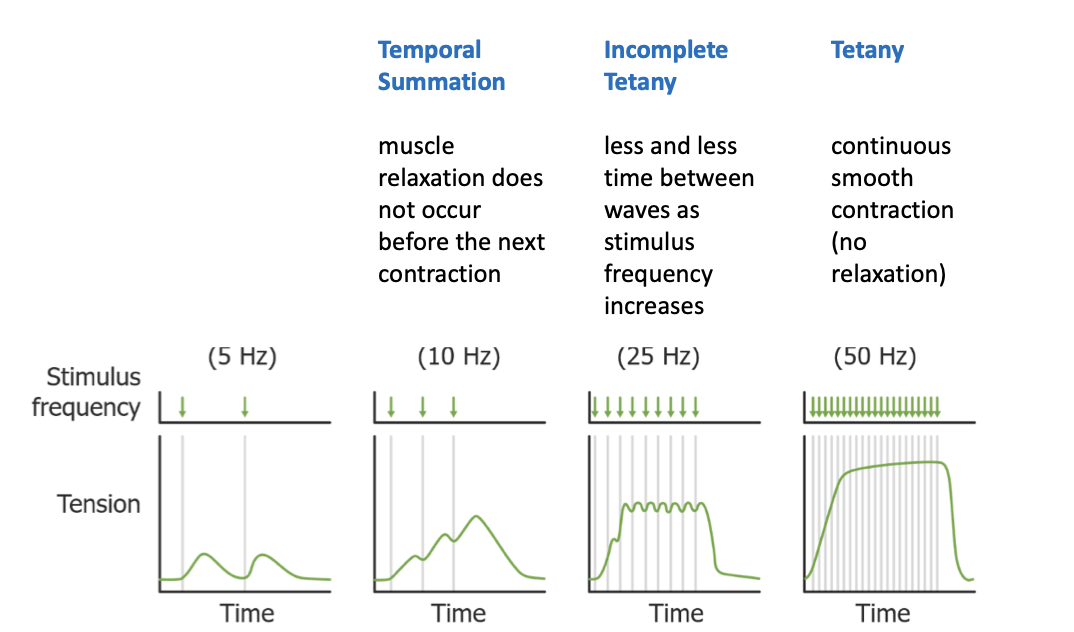
Tetany
Continues smooth contraction of muscle (no relaxation)
Length of sarcomere determines
▪ Amount of overlap between thick and thin filaments
▪ Number of pivoting cross-bridges
Muscle fatigue
Occurs when muscles can no longer perform a required activity
Muscle fatigue is caused by
▪ Depletion of metabolic reserves (creatine phosphate, glycogen, glucose)
▪ Decreased calcium or neurotransmitter at NMJ
▪ Decreased availability of oxygen (oxygen debt) to muscle fibers (increased
demand during exercise)
Major differences of cardiac muscle from skeletal muscle
▪ Shorter, branched cells
▪ 1-2 nuclei in center of cell
▪ Abundant myoglobin and mitochondria
▪ Intercalated discs link cells together (permit
heart to contract as a coordinated unit)
▪ Stimulated by autorhythmic pacemaker
▪ Modulated by autonomic nervous system
Myoglobin and Hemoglobin
Bind oxygen to blood
Smooth Muscle Differences to skeletal muscle
▪ No sarcomeres or intercalated discs (no striations)
▪ Myosin and actin filaments arranged differently
▪ Fatigue-resistant
▪ Modulated by autonomic nervous system
Primary muscle cells
Myocytes
Sarcoplasmic reticulum
SR, plasma membrane of muscle sarcomeres
Sarcolemma
outermost membrane covering each individual muscle fiber
Sarcomere
structural unit of myofibril (one segment of myofibril)
myofilaments
each individual filament inside of a myofibril
Myofibril
Elongated contractile thread made of myofilaments
Organization of muscle fiber
Myofilaments make myofibrils
sections of myofibrils are called sarcomeres
Myofibrils are covered by the sarcoplasmic reticulum
Bundles of myofibrils make one muscle fiber covered by sarcolemma
T-tubule
Invagination of sarcolemma that transports electrical signals into cell
Terminal Cisternae
Enlarged regions of SR that store and release calcium
Triad
Combination of T-tubules and terminal cistern that release calcium into cells cytoplasm when the muscle is stimulated
Thick myofilament
Thick and made from myosin heads
Thin myofilament
More resembles beads on a string and has tropomyosin, troponin, and myosin binding sites
Sarcomere structure
Thin filaments bundle around thick filaments to form the median line. Z disk is the outside edge where thin filaments end
Synaptic cleft
small space between motor neuron and muscle cell
Axon terminal
end of the motor neuron, contains vesicles filled with acetylcholine
motor end plate
folded surface of the muscle cell directly under the synaptic cleft
Myosin binds to
Actin
Troponin binds to
Ca2+
Thick and thin filaments contract muscle in a
ratcheting motion where myosin heads bind to actin and pull it forward, called crossbridging
Power stroke
muscle contraction where myosin binds to actin and pulls
z disc
Structural end of a sarcomere. Marks the end of a sarcomere and the beginning of another.
myosin heads bind to
Actin