GV6: Inducible transcription factors
1/20
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
21 Terms
Endogenous corticoids: Mineralocorticoids
Where: Adrenal cortex
Examples: Mineralocorticoids, aldosterone, glucocorticoids
Function: Water and electrolyte balance
Endogenous corticoids: Glucocorticoids
Glucocorticoids - hydrocortisone and corticosterone
- affect carbohydrate and protein metabolism
- anti-inflammatory and immunosuppressive effects
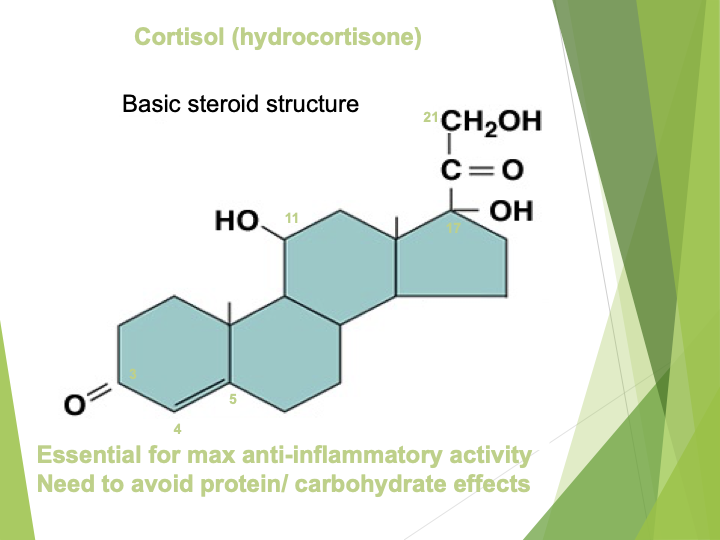
Describe the cortisol structure
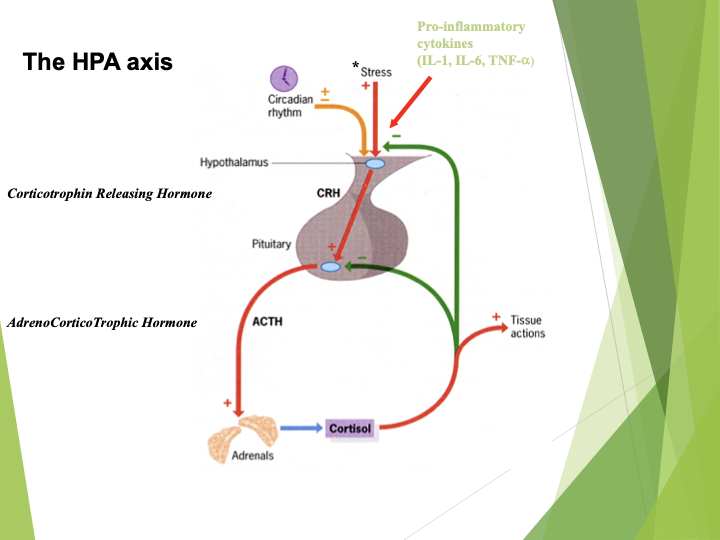
Hypothalamus
Pituitary
Adrenal axis
Natural circadian rhythm releases cortisol
Also stress e.g. infection, environmental
1.Hypothalamus
2.CRH
3.Pituitary
4.ACTH
5.Adrenals
6.Cortisol
What is an issue with steroids
Weaning patients off slowly
Prone to rebound inflammatory mediators
as the patient hasn’t developed endogenous steroids this will take a few weeks to reinstate
What is a consequence of excessive glucocorticoids
Cushing’s syndrome
moon face
high blood pressure
CVD
Diabetes
Skin thinning
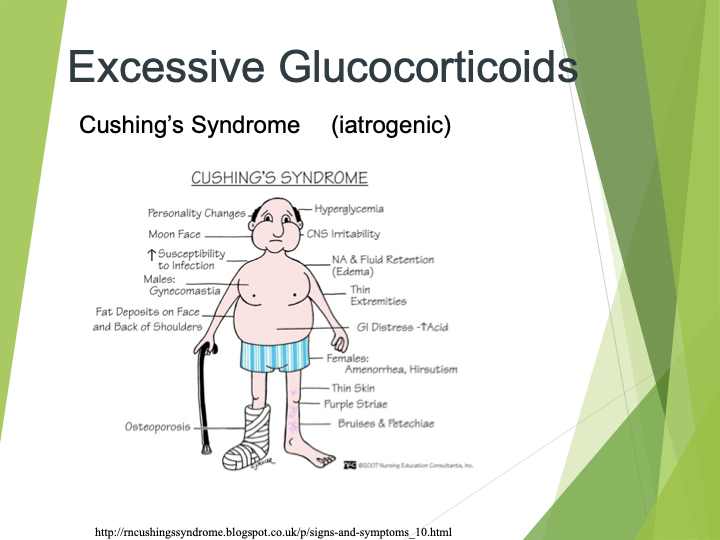
Metabolic side effect: Osteoporosis
Caused by lack of vitamin D (steroid)
reduced calcium absorption
decreased collagen synthesis
Parathyroid hormone then increases Ca++ resorption from bone leading to bone thinning
Diabetogenic
Decrease in glucose uptake and utilisation
increase in gluconeogenesis
increased appetite – obesity
Mineralocortocoid effects
Na/ H2O retention, hypertension, oedema and CV events
list 5 steroids
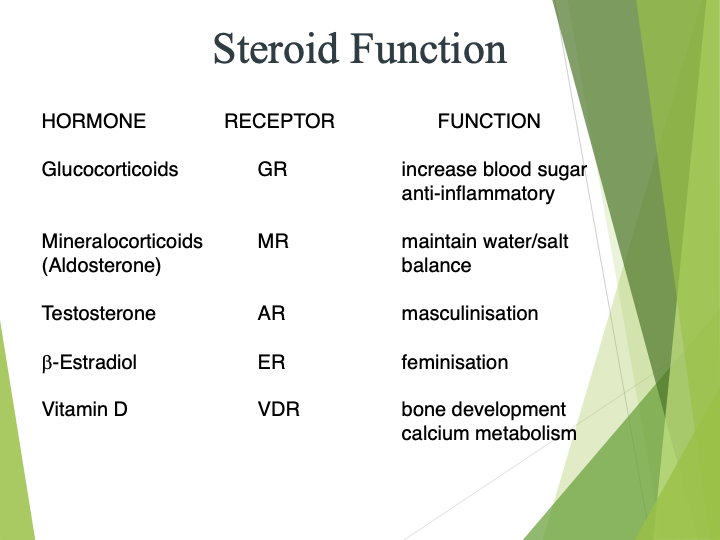
Describe what are steroid transcription factors
Lipophilic hormones
Bind intracellular receptors
Bind as homo (GR) and hetero (Vit D) dimers
What can steroid TF activate
Can act as transcriptional activators and suppressors
Works for multiple weeks
Regulate gene transcription and mRNA stabilisation
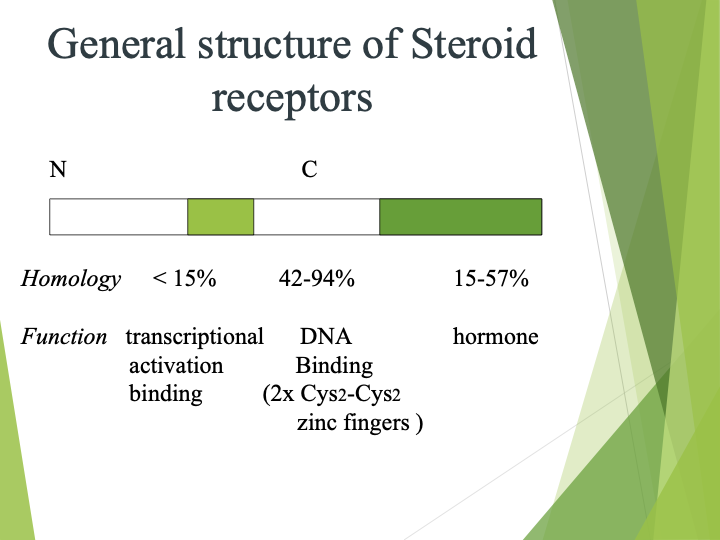
Describe the steroid receptor structure
high homology between family members
not much specificity
doesn’t allow for adjustment
Steroid MOA
steroid
displaces protein
binds to receptor itself
Steroid mOA
Glucocorticoids enter cells and bind to cytoplasmic receptors.
Complex translocates to the nucleus to act as transcription factor
Can bind to response elements and activate anti-inflammatory gene transcription (eg IL-10)
Can bind and repress pro-inflammatory gene activation
(eg COX-2, PLA2)
Can interact and inhibit binding of other transcription factors
(AP-1 and NFkB)
Half site
Will have different spacing between the sequences
Gene control of vitamin D
vitamin D receptor (VDR)
- calcium binding proteins
- osteocalcin (bone development)
Glucocorticoid gene control
•Steroid-activated glucocorticoid receptor
- inhibits expression of IL-1
- collagenase genes
What anti-inflammatory effects do steroids have
Not very effective
Overall broad spectrum dampening agent which works on many parts of immune system
needs to be controlled to prevent immunosuppression
Decrease vasodilation and extravasation
Inhibit cell activation- TH (inhibit IL-2 and clonal expansion)
Decrease production of inflammatory mediators (ROS, prostanoids and leukotrienes, complement and histamine)
Which patient groups are mostly affected by steroids
SLE: systemic lupus
systemic disorders
immunosuppressed patients
Toxicity of corticosteroids
with high dose, long term
Immunosuppression can increase risk of infections
Impaired leucocyte traffic can delay wound healing e.g. ulcers impair blood flow
Suppress HPA axis through feedback inhibition patient must be weaned while endogenous system reactivates