Biomed Neoplasm
1/50
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
51 Terms
Fundamental Hallmarks of Cancer
- Sustaining Proliferative Signalling
- Evading growth supressors
- activating invasion and metastasis
- enabling replicative immortality
- inducing angiogenesis
- resisting cell death
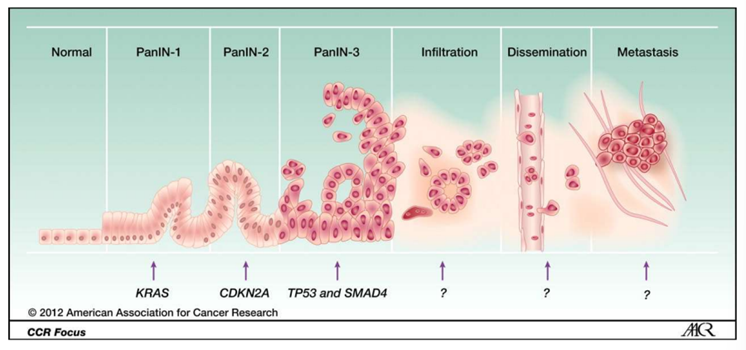
Most Frequent mutated oncogene in pancreatic ductal ademocarcinoma (PDAC)
K-Ras arises from the cells lining the pancreatic ducts, activation (frequency mutation >90%)
Difference between a benign and malignant neoplasm
invasion of surrounding tissues
Properties of Neoplasm
slow growth rate, growth stimulus is cell intrinsic, resemblance to tissue of origin, non-invasive
cancer most common in Australia in 2012 according to AIHW
breast cancer
cancer most lethal in Aus 2021
lung cancer
key event leading to death of most cancer patients
Metastasis
what is pre-metastatic niche
promotes establishment of metastasised tumour cells in other organ. location in body by creating right microenvironment. Ensures that when tumour cells reach destination they have
supportive stromal cells
growth factors
reduced immune surveillance
a matrix structure that facilities attachment and proliferation
AA most abundant in plasma in cancer cell catabolic processes
Glutamine
Glutaminolysis - cells convert glutamine into TCA cycle metabolites (provide intermediastes for AA and drive energy aquisition)
upregulated in cancer cells
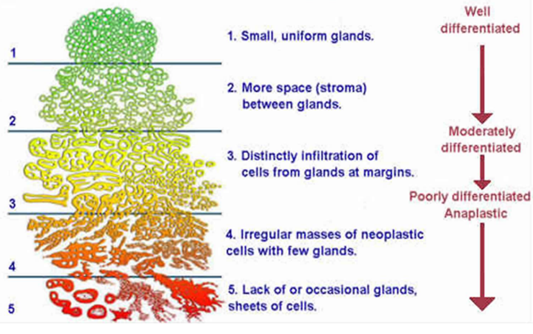
The Gleasons System of tumour grading is applied to describe which cancer
Prostate Cancer
two most common patterns of growth seen in the biopsy sample are each given a number from 1-5, then these two numbers are added together to give the Gleason score
Goes from well differentiated —> poorly differentiated (Anaplastic)
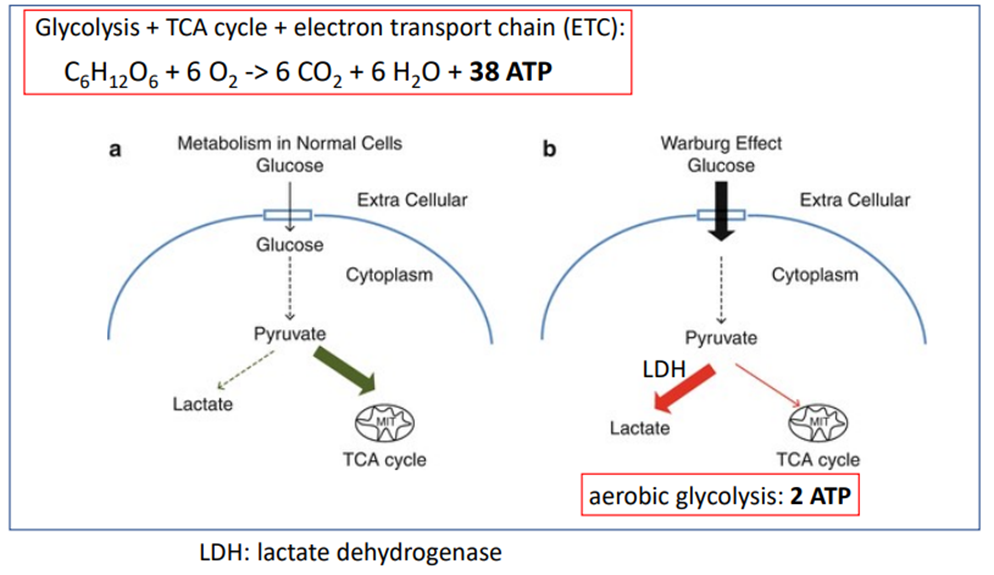
what imaging technique takes advantage of the tendency of cancer cells to use Warburg effect to obtain energy
FDG-PET
uses radioactive tracer to visualise how tissues and organs function in relation to glucose metabolism
A patient with breast cancer has a 4 cm tumour, with cancer cells identified in 7 lymph nodes in the armpit, and metastases present in the liver. What stage describes their cancer?
Stage IV
only stage where cancer is found somewhere else is Stage IV
Category 1 = breast cancer found 1-3 lymph nodes in armpit
Category 2 = breast cancer found
4-9 lymph nodes in the armpit
1 or more lymph node under breast bone NOT any in lymph nodes in armpit
Category 3 = breast cancer found
10 or more lymph nodes in armpit
1 or more lymph nodes above or below collarbone
1 or more lymph nodes under breast bone AND 1 or more lymph nodes in armpit
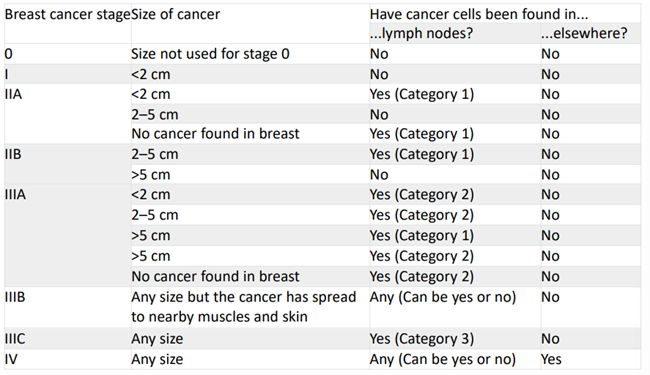
A patient with breast cancer has an 8 cm tumour, with cancer cells identified in 9 lymph nodes in the armpit, and metastases present in several long bones. Which of the following stages describes their cancer (according to the breast cancer-specific staging system)?
Stage IV
What clinical activity is tumour markers most generally used for
Follow-Up
all tumour markers are useful for follow up
what are the activators for angiogenesis
- VEGF-A
- VEGF-B,-C
- FGF1 (aFGF)
- FGF2 (bFGF)
- Other FGFs
what are the inhibitors of angiogenesis
- Thrombospondin 1, 2
- Interferon alpha/ beta
- Angiostatin
- Endostatin
- Collagen IV fragments
How does p53, the ‘guardian of the genome’, protect against the accumulation of DNA damage in normal cells and contrast this to cancer cells in which p53 is mutated?
Normal Cells = Stalls cell cycle until DNA damage is repaired. Promotes DNA repair processes. If DNA damage cant be repaired, induces apoptosis
Cancer cells = without p53 activity, DNA is not repaired and cell cycle progresses, leading to the accumulation of multiple DNA lesions in a single cell lineage.
Name the two genes most frequently associated with hereditary breast cancer and the role they play in a normal cell.
BRAC1 and BRAC2, which play a role in homologous recombination/ repair of DNA damage
Contrast external beam radiation and brachytherapy.
External beam – linear accelerator focussed on tumour
Brachytherapy – locally placed nuclear isotopes that undergo radioactive decay
What do the terms T, N, M, X and O refer to in the TNM method of cancer staging?
T = size and extent of primary tumour
N = number of nearby lymph nodes that have cancer
M = whether cancer is metastised
X = cannot be measured
O = not present/ cannot be found
Name the two major histological subtypes of lung cancer and indicate which is the most common.
Small cell carcinoma
Non-small cell lung carcinoma (NSLC) (most common)
Which organs are the most common sites for metastases across all cancers?
Bone, Brain, Liver, Lungs
What is the most common type of cancer in Australia?
Non-melanoma skin cancer (aka keratinocyte cancers)
Name the two different types of graft used in haematopoietic stem cell transplantation and a specific or type of tumour that this technique is used to treat.
Autologous
Allogeneic
Myeloma/ Leukaemia/ Lymphoma
Describe one way in which you could make a mouse model of Pancreatic Cancer.
KPC mice
Patient-derived xenografts - take a tumour cell from patient and put it into an immunodeficient mice
- Immunodeficient mice
- Subcutaneous or orthotopic
match the terms
1. Herceptin a. Chemotherapy
2. Given prior to primary treatment b. Adjuvant therapy
3. Topoisomerase inhibitor c. Targeted therapy
4. Given after primary treatment d. Neoadjuvant therapy
Herceptin – targeted therapy
Given prior to treatment – neoadjuvant therapy
Topoisomerase inhibitor – chemotherapy
Given after primary treatment – adjuvant therapy
Examples of benign neoplasms
adenomas - glandular epithelial tissue
hemoangiomas - blood vessels
meningiomas - meninges
fibroids or fibromas - connective tissue
lipomas - adipose cells
hamartomas - mixture of tissue
oncogene
mutated proliferative gene (gene that has potential to cause cancer)
Proto-oncogene: normal cellular counterpart of an oncogene
function is activated in cancer cells
e.g., K-Ras, cSrc, cMyc
Tumour Suppressor
inhibitor of cellular growth
function is inactivated in cancer cells
both alleles need to be mutated/ deleted
e.g., p53, Rb
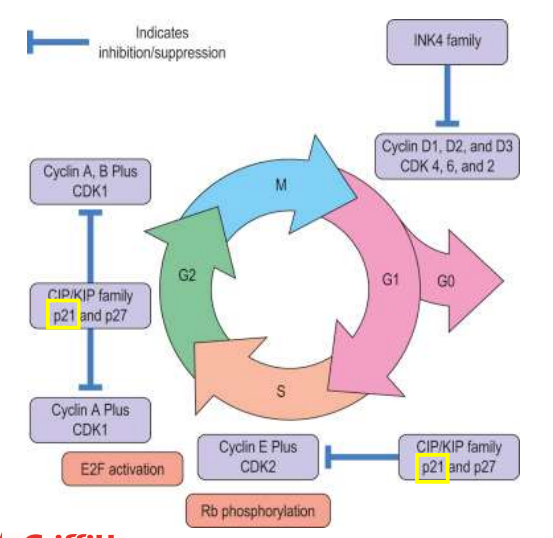
Cell Cycle Regulation
Ras and Myc proto-oncogenes infuse D and E type cyclins
these cyclins complex with cyclin-dependent kinases (CDKs) and promote S phase entry/ transition (checkpoint progression), after which cell-cycle progression is GF independent
Apoptosis
Caspase 8 - directly activates caspase 3, intrinsic pathway
caspase 3 = executioner
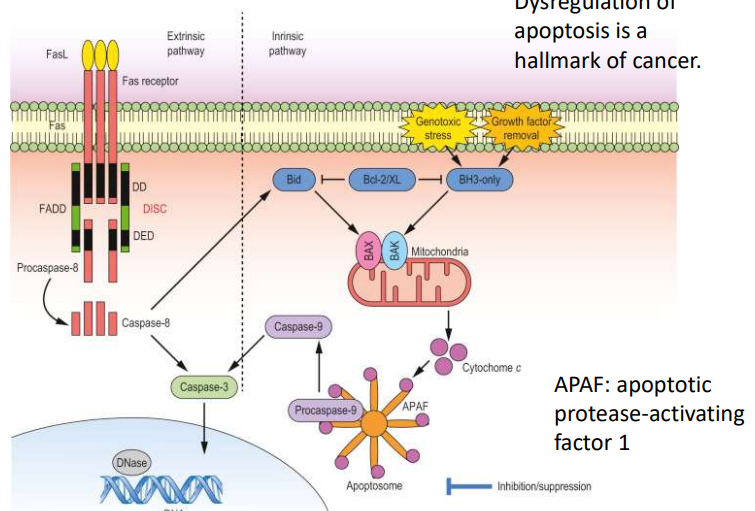
Dysregulation of Apoptosis (things that stop apoptosis)
hallmark of cancer
impaired receptor signalling pathway
disrupted balance of Bcl-2 family of proteins
defects/ mutations in p53
reduced expression of caspases
increased expression of IAPs
additional hallmarks of cancer
avoiding immune destruction
tumour promoting inflammation
genome instability and mutation
deregulating cellular energetics
Genome instability in a cancer cell
Cancer cell —> DNA damage/ mutation —> damages repair mechanisms, inability to sense damage, inability to arrest —> damage —> damage to apoptotic pathway, mitosis —> perpetuation of error to daughter cells, rapid accumulation of genomic damage —> leads to accumulation of more key cancer cell characteristics
normal cell - mediated by p53 predominantly
DNA damage/ mutation —> arrest —> repair attempt —> 1. Extensive damage —> Apoptosis OR 2. correction —> mitosis
Autophagy
Vesicle nucleation
vesicle elongation
vesicle docking and fusion with lysosome
vesicle breakdown and content degradation
“self-eating”
important for maintenance
digested into precursor molecules e.g., proteins to AA’s
Cancer classification
defined by cell/ tissue type of origin
carcinoma - epithelial cells
sarcoma - connective tissues
melanoma - melanocytes
lymphoma - lymphocytes
leukaemia - bone marrow resident cells
myeloma - bone marrow resident lymphocytes
glioma - glial cells
2 categories of Lymphoma
hodgkin lymphona
non-hodgkin lymphona
Cachexia
weakness and wasting of the body due to severe chronic illness
tumour markers
hormone - e.g., human chorionic gonadotrophin (HCG) secreted by choriocarcinoma
enzymes - e.g., prostate-specific antigen in prostate carcinoma
tumour antigens - e.g., carcinoembryonic antigen (CEA) in colorectal carcinoma
useful for:
screening
monitoring treatment
assessing follow up
diagnosis
prognosis
Screening for cancer
Test must detect the disease earlier than routine methods
Earlier treatment must lead to improved outcomes
Benefits of screening must be greater than the risks of any subsequent diagnostic and therapeutic treatment
Screening for breast cancer
self-examination
clinical examination/ mammography
genetic testing: BRAC1/2
Lung Cancer Staging
NSCLC
Occult (hidden) stage - cancel cells found in sputum or other fluids from lung, but no cancer in other tests
Stage O (carcinoma in situ) - cancer in top layers of cells lining the air passages (not spread to lymph nodes or distant areas of the body
Stages I, II & III ( all have A and B parts) - involve cancer increasing in size and spreading to nearby lymph nodes
Stage IV - cancer may have spread to opposite lung, space around lungs or heart or other organs, e.g., bone, liver and brain
small cell lung cancer
limited stage - caner is only 1 side of chest (possibly incl. lymph nodes) and can be treated with a single radiation field
extensive stage - cancer spread widely throughout the lung, to the other lung, to lymph nodes, on the other side of the chest or distant organs
imaging
non-invasive medical imaging at multiple times in the course of the illness for managemet
detection
characterising lesions
locoregional and systemic staging
prognosis
assessing therapeutic responses
precisely guiding biopsies and therapies
radiogrpagy, CT, ultrasonography
MRO and nuclear medicine methods, PET
Adjuvant therapy
additional treatment given after the primary treatment to lower the risk that the cancer will come back
neoadjuvant therapy
treatment given as a first step to shrink a tumour prior to the main treatment
targeted therapies
act on specific molecular targets
often cytostatic (block tumour cell proliferation)
prostate cancer treatment
rely on testosterone to grow —> prostatectomy
external beam radiation and brachytherapy
BUT - the tumours themselves can produce their own testosterone
what is neoplasm
Abnormal mass of tissue that forms from dysfunctional cells (non cancerous)
Define Cancer
Diseases where abnormal cells divide without control and can invade nearby tissues (aka ‘malignant’ tumour)
screening for colon cancer
colonoscopy: polyps; early cancer
stool testing for blood/ DNA
carcinoembryonic antigen (CEA) in blood
screening for prostate cancer
prostate specific antigen (PSA) in blood - activated by androgen receptor in prostate cells
benign enlargement and acute chronic inflammation leads to increased PSA levels