EXAM 1- JONES
1/60
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
61 Terms
PRACTICE:
Which of the following is considered a part of the Muscularis Externa?
a. basement membrane
b. muscularis mucosal
c. serosa
d. longitudinal smooth muscle
d
PRACTICE:
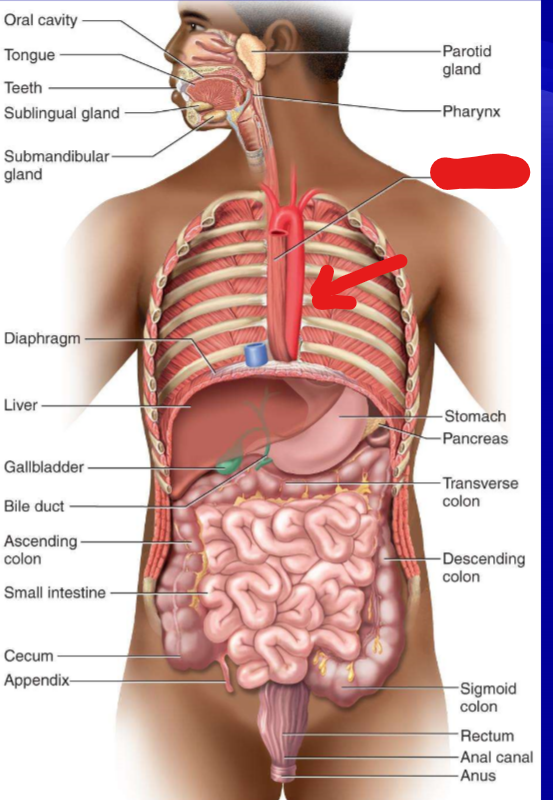
What part of the GI tract is the arrow pointing towards?
esophagus
What are the 2 main parts to circulation in the GI tract?
spleenic side—> blood comes FROM the heart to the organs
portal side—> blood comes FROM the organs to the liver than back to the heart
What organ receives all the blood from the portal vein and then sorts/stores blood before returning it to the heart?
a. spleen
b. stomach
c. small intestine
d. pancreas
e. liver
e. LIVER
What are the 4 layers to the GI wall?
Mucosal
Submucosal
Muscularis Externa
Serosa
What are the 4 parts of the mucosal layer of the GI wall?
epithelial cells
basement membrane
lamina propia
muscularis mucosal
What is the job of the muscularis mucosal?
move villi in/out to CONTROL SURFACE AREA
What layer of the GI wall is “space” and contains glands, ducts, etc.?
submucosa
What layer of the GI wall has the function of “holding things in place” and is like an outer protective layer?
Serosa
What 2 muscles make up the muscularis externa? Are they smooth or skeletal muscle?
Inner circular muscle
outer longitudinal muscle
both are SMOOTH muscle
For smooth muscle, what causes contraction? What causes relaxation?
contraction—> Ca++ (from SR, transporters, or Ach)
relaxation—> increase cGMP, inhibiting cAMP
What cells have a pacemaker ability in the GI tract?
ICC (Interstitial cells of Cajal)
What are slow waves? What are spike potentials?
slow waves- local depolarizing events generated by ICC, set BER
spike potentials- generated by increased slow wave potentials- lead to contractions
What are plexus? What are their names and where are they found in the GI wall?
plexus- nerve cell bodies
submucosal plexus—> found under the submucosa layer
myenteric plexus—> found between circular and longitudinal muscle
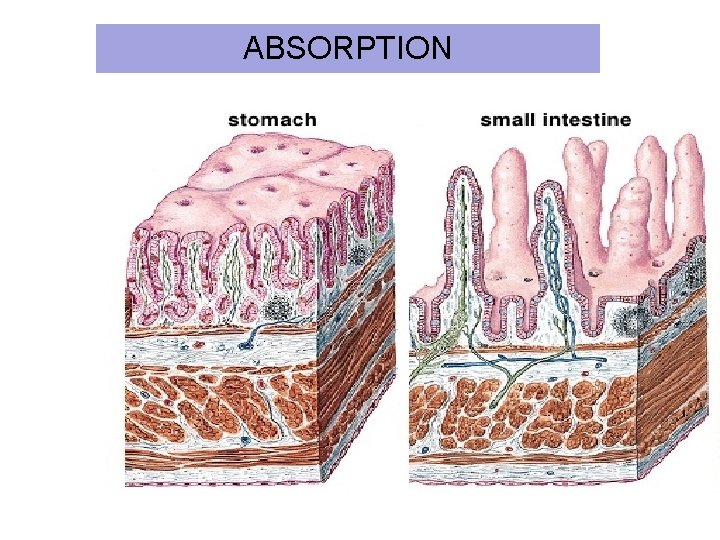
How does the wall of the stomach compare to the small intestine?
THE MUCOSA LAYER!!!!
in stomach—> invaginate and make pits
in small intestine—> have villi and crypts (small invaginations)
In the GI tract muscles move by segmentation or peristalsis…describe both.
segmentation- “mixing”, moves food back AND forth to break it up
PERISTALSIS- forward movement (HOW OUR FOOD GOES DOWN OUR INTESTINES)
basically we contract behind, and send inhibitory signals ahead to relax ahead. this propels food forward
What is the name of the neural control of the GI tract?
ENTERIC
Because we have plexxi in the GI tract, does that mean we don’t use our CNS or any outside innervation?
no—> enteric but can be controlled by ANS
Short reflexes only use the ____________ neural system. Long reflexes also use the _____.
a. central, enteric
b. vasovagel, enteric
c. enteric, central
d. enteric, somatic
c. enteric, CNS
Does the following example describe long or short reflexes:
internal stimuli—> chemoreceptor—> myenteric plexus—>smooth muscle—> contraction
short (does not involve the CNS)
What is a combination of mucous, electrolytes, lysozyme, IgA and is secreted by the parotid, submandibular, and sublingual glands?
saliva
What salivary gland is stimulated the most when eating?
parotid
What are the 2 cells of the salivary glands? What are their functions?
acinar cells- secretors (serous and mucous)
ductal cells- modifiers (absorption and secretion)
Does the parasympathetic or sympathetic system mainly control salivation?
Parasympathetic (doesn’t mean SNS has no effect)
SALIVA IS ALWAYS _____________________ to PLASMA.
a. isotonic
b. hypertonic
c. hypotonic
c
How does a fast and slow flow rate effect the tonicity of saliva?
fast—> less hypotonic
slow—> more hypotonic
In the ductile cells of the salivary glands, what electrolytes go out of the saliva and which come in?
out—> Na+, Cl-
in—> K+, HCO3-
Why is saliva hypotonic?
more NaCl is removed than K+, HCO3 is brought in
Answer the following about Sjogren syndrome:
Cause
Sym
Tx
Cause- autoimmune destruction of salivary gland
Sym- DRY MOUTH (xerostomia), DRY EYES (keratoconjunctivitis sicca), mouth ulcer
Tx- fluids, stimulants, steroids
Describe the voluntary phase of swallowing/deglutition:
chew and push food to back of throat
mechanoreceptors are activated—> begins involuntary phase
Describe the involuntary phase of swallowing/deglutition:
several muscle events occur:
upper esophageal sphincter opens
peristalsis
lower esophageal sphincter opens
receptive relaxation ( NO and VIP)
What is secondary peristalsis?
if food gets stuck in your throat, your enteric system activates a super strong push
The Upper esophageal area is covered in ___________ muscle. The lower esophageal area is covered in _________________ muscle.
skeletal, smooth
The _________ relaxes to allow food to enter the stomach because of NO and VIP.
LES (lower esophageal sphincter)
When does the LES relax?
AS SOON AS YOU SWALLOW (not when the food reaches it)
What is Achalasia?
loss of inhibitory neurons
causes LES to not be able to RELAX
Answer the following about GERD:
cause
symptom
tx
cause- LES issues, hernia, can’t empty stomach
symptom- esophagitis
tx- antacids, h2 blockers, PPIs, motility drugs, lifestyle changes
What are the functions of the stomach?
storage
mixing (break up food)
digestion
antibacterial secretions
What the 3 main regions of the stomach? (top to bottom)
fundus
body
pylorus
Does the mucosa in the stomach form pits, crypts, or villi?
pits
The ________ is a region in the fundus in the upper stomach.
cardia
What is the name of the sphincter between the esophagus and the stomach? What is the name of the sphincter between the stomach and intestine?
eso-stomach: lower esophageal sphincter
stomach-intestine: pyloric sphincter
When does the pyloric sphincter fully relax?
NEVER—> always contracted and is only slightly opened when food needs to exit
What are the 2 types of pits in the stomach? Where are they found? What cell types are found in each?
oxyntic pits (body)- mucous, parietal, ECL cells, and Chief cells
pyloric pits (pylorus)- Mucous, D cells, G cells
For each of the following cell types, describe the substance secreted by the cell and the substance’s function.
mucous neck cell, parietal cells, ECL cells, chief cells, D cells, G cells
Cell type | Substance secreted | Function |
Mucous neck cell | Mucous and Bicarb | Mucous- protects Bicarb- gets in mucus layer and helps neutralize acid |
Parietal cells | HCl and IF | HCl- digestive acid IF- B12 |
ECL cells | Histamine | Blocks parietal not ECL cells--> paracrine local signaling |
Chief Cells | Pepsinogen | Pepsinogen interacts w/ HCl to form pepsin which degrades proteins |
D cells | Somatostatin | Inhibits G-cells/ acid secretion in general |
G cells | Gastrin | HORMONE- stimulates acid secretion, promotes contraction (main idea--supports digestion of food) |
What 3 hormones regulate the release of HCl? (3 mediators)
gastrin
ACh
Histamine
Describe how we secreting acid:
what kind of pumps?
when were not digesting where are the pumps?
where are the pumps when were digesting?
Increasing what 2 things make the pump move intra to extra cellular?
What are those 3 stimulus?
What is the end result?
PROTON pumps
at rest= vesicles w/pumps are inside the cell
during digestion- at surface of parietal cell
increasing Ca++ or cAMP
3 stimuli- Ach, Gastrin, Histamine
end result- HCl secretion
How do we get the proton (H+) for HCl?
carbonic anhydrase takes water and carbon dioxide and forms H+ and bicarb
How do we get the Cl- for HCl?
on basolateral side we exchange bicarb for Cl-
What happens to H+ and bicarb after its formed?
H+ moves into lumen through H+/K+ ATPase
bicarb moves into the blood
Describe gastric motility/ the contractions and relaxation in the stomach:
receptive relaxation- when LES opens bc of VIP/NO also opens up the stomach
peristaltic contractions- once food is in stomach we contract down the stomach… contractions get stronger as you move down
pylorus contractions intensify and cause retropulsion- when it hits bottom of stomach it doesn’t just all go into intestine it goes back up stomach and contracts down again
slow emptying
Can slow waves in the stomach cause contraction?
YES!!!!!!
A diet that consists of proteins and lipids will empty _______ than an all liquid diet.
slower
What stimulates the release of ACh, gastrin, and histamine?
ACh- parasympathetic post ganglion
Histamine- Ach and Gastrin activate ECL cell
Gastrin- distention of stomach or enteric nervous system releases GRP
What inhibits the release of somatostatin from D cells?
Ach
What activates the release of somatostatin from D cells?
low pH (H+)
entero gastric reflex—> CCK and secretin are intestinal hormones that turn on D cells
GIP and VIP
Describe the cephalic phase of gastric secretion
Think: before eating
we want to prepare stomach for food
mainly stimulate stomach to secrete acid thru vagus nerves
stimulate Mucous cells, chief cells, parietal cells, g cells all to prepare for the food incoming
20% of acid secretion
Describe the gastric phase of gastric secretion:
Think: eating phase
STRETCH STOMACH—> mechanoreceptors detect stretch tell enteric neural system to secrete acid
our enteric system stimulates mucous cells, chief cells, parietal cells, and g cells all to help break down our food
70% of acid secretion
Describe the intestinal phase of gastric secretion:
Stimulatory effect: g cells in intestine= increase acid secretion
10% of acid secretion
Inhibitory effect: entero-gastric reflex and intestinal hormones
Describe how gastric secretion is inhibited:
ENTERO-GASTRIC REFLEX
turns off the stomach
Hormones: CCK, secretin, VIP, GIP
How is an ulcer formed? What are some not-natural things that can damage the mucosal defenses?
ulcer is formed when acid breaks thru epi layer and degrades
some things that can damage- H. pylori, NSAIDs, aspirin, cigs, alcohol, i