Eye Clinical Skills + Workshop
1/13
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
14 Terms
Steps for basic examination of the eye
Wash hands
Explain what you are about to do
“I am now going to do a basic examination of your eye. I will gently pull down your lower and upper lid to look for any abnormalities. ”
Gain patient consent
General observation of patient’s eyes/eyelids » redness, inflammation, discharge
To view the conjunctiva
Gently pull down the lower lid and ask patient to look upwards, left and right
Gently lift upper lid and ask patient to look down, left and right
Note any redness, blood vessels etc
Ask patient to feel for any tenderness over the sinus bones
“Do you feel any tenderness or soreness when you press over your cheekbones or forehead?”
Steps for using ophthalmoscope to view the conjunctiva
Wash hands
Explain procedure
“I will now use an ophthalmoscope, which is an instrument that lets me look at the back of your eye, including the retina and the blood vessels. It helps us check eye health and allows me to spot any issues. I’ll gently pull down your lower and upper lid and shine a light into your eye for a few seconds while you look straight ahead.”
Gain patient consent
Ophthalmoscope
Use middle sized light and focussing wheel on 0
Hold ophthalmoscope like a microphone and put index finger on dial
If examining right eye of patient, hold with right hand and check with right eye and vice versa when examining the left eye
‘Look directly into the light’
‘Look back at me’ » to check reaction of pupils to the light
‘Cover your unaffected eye with your palm and read the information printed on this card’ » note any difficult reading
When to REFER patients based on eye examination
General eye examination
Suspected foreign body in the eye
Any swelling around eye or face
Photophobia » ‘do bright lights make your eyes hurt or feel uncomfortable?’
Severe pain in the eye
Vision affected
Copious green/yellow smelly discharge which re-accumulates when wiped away
Ophthalmoscope
Pupil an unusual shape or doesn’t react to light
Cornea looks cloudy
Restricted eye movement
Steps for eye drop administration
Wash hands thoroughly with soap and water
Avoid touching the dropper tip against the eye or anything else
Tilt head back to look at the ceiling
Pull down lower eye lid with index finger to form a pocket
Hold dropper tip down with other hand as close to the eye as possible without touching it
While looking up, gently squeeze the bottle, so that a single drop falls into the pocket made by the lower eyelid
Blink the drops in
Place finger on tear duct and apply gentle pressure
Wipe any excess liquid from closed eyelid/face with tissue
If more than one drop is to be administered to the same eye, wait at least 5 mins before instilling the next top
Replace and tighten cap on dropper bottle
Wash hands to remove any medication
Other supports
PILs
Administration charts
Check patients who have glaucoma and drive have informed the DVLA

Case Study 1
It is Saturday afternoon and Matthew Hall has asked the pharmacy assistant if he could have some eye drops as they have discharge from both eyes now for four days and is not getting better.
The pharmacy assistant has referred this request to you, as the community pharmacist.
Your system shows only a single prescription 2 years ago for mebeverine 135mg tablets: 1 tablet 3 times a day
You have asked Matthew to come to the pharmacy consultation room. You note their eyes are generally red and that there is some sticky discharge in both corners
Redness in both eyes
Sticky discharge
Duration: 4 days and not improving
No mention of allergy, itchiness, or watery discharge » which would suggest viral or allergic
Diagnosis:
Bacterial conjunctivitis
Treatment:
Chloramphenicol eye drops 0.5%
1 drop every 2 hours for 48 hours
Then reduce to every 4 hours
For 5 days total
Case Study 2
Yesterday Alan Peterson came to the pharmacy to hand in a prescription for latanoprost 50 microgram / mL eye drops, one drop in each eye once a day.
You noted when you reviewed the pharmacy MR that Alan had not received these eye drops before and asked himif it was a new prescription. You note that Alan is also prescribed Clenil 100 inhaler and a salbutamol inhaler for treatment of their asthma.
Alan explained that they have recently started on their eye drops after being referred by their optometrist and their GP to the hospital eye clinic following their annual eye appointment. The ophthalmologist confirmed the optometrist's diagnosis of chronic open angle glaucoma.
Alan Peterson has now come to collect their prescription for latanoprost 50 microgram / mL eye drops and has agreed to see you in the pharmacy consultation room to discuss their understanding of glaucoma and to check their administration technique.
What is glaucoma and what does latanaprost do?
How should the patient administer the eye drops?
Side effects?
Adherence information?
Asthma note
What is glaucoma and what does latanoprost do?
Glaucoma damages the optic nerve due to raised pressure in the eye.
Latanoprost helps by increasing fluid drainage from the eye, lowering pressure.
It does not fix existing damage, but it prevents further vision loss.
Stopping drops can lead to permanent vision impairment, even if the eyes feel “fine.”
How to use eye drops:
One drop in each eye once daily — preferably at night.
Tilt head back, pull lower lid down to create a pocket.
Avoid touching eye or lashes with bottle tip.
After instilling, press gently on the inner corner of the eye (punctal occlusion) for 1–2 minutes — reduces systemic absorption and side effects.
If using more than one type of drop, wait 5 minutes between drops.
Remove contact lenses before use; wait at least 15 minutes before reinserting.
Side effects
Mild redness or irritation
Increased pigmentation of the iris over time (eye colour darkening — often permanent)
Adherence & importance of continuation
This is a lifelong condition.
Drops must be used every day, even when the eyes feel normal.
Missing doses can allow pressure to build and cause nerve damage.
Asthma note (important!)
Latanoprost generally does not affect asthma.
No major interaction with Clenil or salbutamol.
Case Study 3
Mrs X attends a GP appointment following advice from her local optician. The GP measures her intraocular pressure (IOP) that reads 25 mmHg and informs Mrs X that she has developed glaucoma. Mrs X's medical notes state that she Has a history of asthma which she also confirms to the GP. The GP prescribes her with Latanoprost eye drops.
What is the normal intraocular pressure of the eye and what is used to measure this?
10–21 mmHg (millimetres of mercury).
IOP is measured using an instrument called a tonometer.
So Mrs X’s IOP is higher than normal
Case Study 3
Mrs X attends a GP appointment following advice from her local optician. The GP measures her intraocular pressure (IOP) that reads 25 mmHg and informs Mrs X that she has developed glaucoma. Mrs X's medical notes state that she Has a history of asthma which she also confirms to the GP. The GP prescribes her with Latanoprost eye drops.
IOP lowering medication for glaucoma
1st line: Prostaglandin analogues
Relax muscles in the interior structure = increase aqueous humour outflow = reduce IOP
Side effects: increase melanin so can brown the iris
E.g. Latanoprost, Travoprost
2nd line: Beta blockers
Decrease production of aqueous humour
Contraindications: asthma, bronchospasm, bradycardia, hypotension
Side effects: can get red eye at the start » if this doesn’t resolve, switch to another BB, then try a preservative free formulation or different class
E.g. Betaxolol, Timolol
3rd line: Cholinergics / Miotics
Mimics action of parasympathetic NS
Increases aqueous humour outflow = reduces IOP
Side effects: can cause ciliary spasm affecting night vision
E.g. Pilocarpine
3rd line: Alpha-adrenergic agonist
Mimics action of NA on sympathetic NS
Side effects: palpitations, headaches
E.g. Apraclonidine, Birmonidine
Case Study 3
Mrs X attends a GP appointment following advice from her local optician. The GP measures her intraocular pressure (IOP) that reads 25 mmHg and informs Mrs X that she has developed glaucoma. Mrs X's medical notes state that she Has a history of asthma which she also confirms to the GP. The GP prescribes her with Latanoprost eye drops.
Explain why Mrs X’s asthma is an important consideration, although these are eye drops
Beta-blocker drops like timolol are absorbed into the bloodstream through the nasal mucosa, and can affect the lungs
They block β₂ receptors in the bronchial smooth muscle → airway constriction
In an asthmatic, this can cause wheezing, shortness of breath, or an asthma attack.
Case Study 3
Mrs X attends a GP appointment following advice from her local optician. The GP measures her intraocular pressure (IOP) that reads 25 mmHg and informs Mrs X that she has developed glaucoma. Mrs X's medical notes state that she Has a history of asthma which she also confirms to the GP. The GP prescribes her with Latanoprost eye drops.
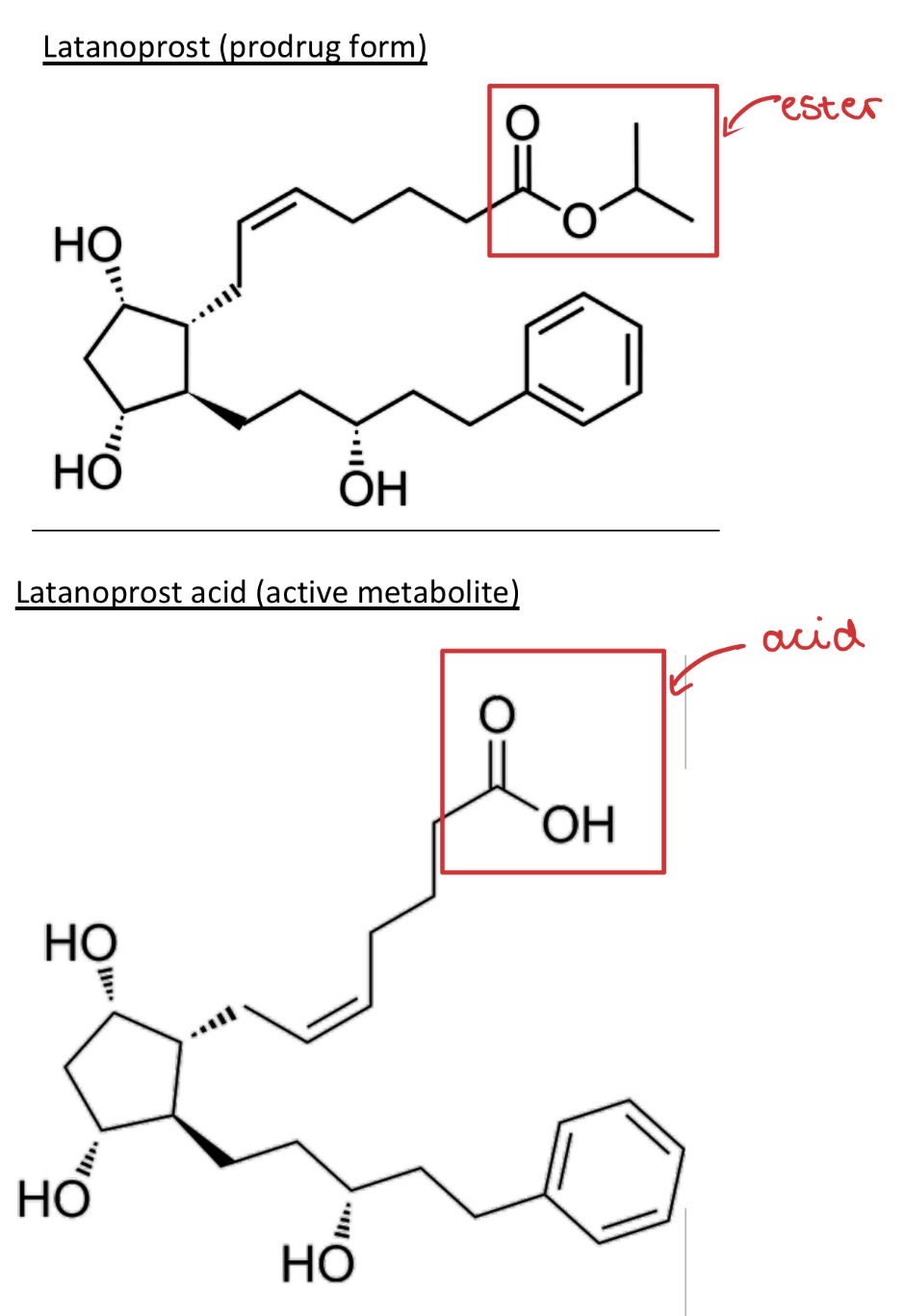
Latanoprost is a prodrug. Draw the structure of latanoprost and its active metabolite?
Case Study 3
Mrs X attends a GP appointment following advice from her local optician. The GP measures her intraocular pressure (IOP) that reads 25 mmHg and informs Mrs X that she has developed glaucoma. Mrs X's medical notes state that she Has a history of asthma which she also confirms to the GP. The GP prescribes her with Latanoprost eye drops.
Which naturally occurring prostaglandin does the active metabolite mimic?
Prostaglandins F2α
PGF2α acts on FP receptors in the ciliary muscle of the eye
This increases uveoscleral outflow of aqueous humour = reduces intraocular pressure
Latanoprost acid is a synthetic analogue of PGF2α with longer duration and better receptor selectivity
Case Study 3
Mrs X attends a GP appointment following advice from her local optician. The GP measures her intraocular pressure (IOP) that reads 25 mmHg and informs Mrs X that she has developed glaucoma. Mrs X's medical notes state that she Has a history of asthma which she also confirms to the GP. The GP prescribes her with Latanoprost eye drops.
What is the purpose of administering latanoprost as a prodrug?
Prodrug ester form is highly lipophilic so able to more easily cross the lipid-rich cornea into the eye = better corneal absorption
Converted in the eye to its active acid form, allowing effective intraocular action with reduced systemic absorption
Case Study 3
Mrs X attends a GP appointment following advice from her local optician. The GP measures her intraocular pressure (IOP) that reads 25 mmHg and informs Mrs X that she has developed glaucoma. Mrs X's medical notes state that she Has a history of asthma which she also confirms to the GP. The GP prescribes her with Latanoprost eye drops.
Why should unopened bottles of latanoprost be stored in the fridge?
Latanoprost is sensitive to temperature in its pro-drug form:
Storing in the fridge prevents ester hydrolysis = preserves shelf life