Module 3: Cells and Lymphoid Organs of the Immune System
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
47 Terms
Hematopoietic stem cells (HSC)
Myeloid progenitor cells (MPC) and lymphoid progenitor cells (LPC)
HSCs differentiate into what 2 separate lineages
Red blood cells, platelets, neutrophils, monocytes, eosinophils, basophils, mast cells, and certain dendritic cells
Myeloid progenitor cells (MPC) further differentiate into
T and B lymphocytes and specific dencritic cells
Lymphoid progenitor cells (LPC) further differentiate into
Types of dendritic cells
Both MPCs and LPCs give rise to
Steady state level
A homeostatic condition thay is maintained under normal conditions (without infection or immune challenges) It is the number of cells that arise from division and differentiation and the number of cells removed by apoptosis
Levels and types of cytokines produced by bone marrow stromal cells
Cytokines produced by activated cells
Regulation of receptor expression by stem and progenitor cells
Apoptosis
Steady state is regulated by (x4)
3.7×10^11
Human body produces approximately how many white blood cells a day
Membrane-bound immunoglobulins (mIg)
B-lymphocytes possess
T-helper cells and cytotoxic-T cells
T-cells are divided into
CD4+
T-helper cells have what CD marker
CD8+
Cytotoxic T-cells have what CD marker
Natural killer cells (NK)
Lymphocytes part of the innate immune response that can kill host cells (e.g. virus infected cells) without making their own antigen-specific receptors (thus they lack T-cell receptors and mIg)
NKs and cytotoxic T-cells
What cells contain cytoplasmic granules with lytic enzymes
Lytic enzymes
Enzymes that kill virus-infected cells upon contact
Cancer and viral infection
Low NK cell count means an individual is more prone to
Cluster of differentiation markers (CD markers)
Specific type of molecules found on the surface of cells that help differentiate one immune cell type from another and also function in cell signaling and adhesion
Monocytes
Migrate to tissues and differentiate into various macrophages
Differentiated macrophages
Larger macrophages perform specific functions based on their location and have different receptors based on their tissue-specific location (contain more hydrolase enzymes, have increased phagocytic ability, and contain a variety of soluble factors)
Professional antigen-presenting cells (pAPC)
Regardless of differentiation all macrophages act as
Microglia
Brain tissue macrophages that function in neural circuit development (synaptic pruning)
Alveolar macrophage
Lung tissue macrophages that function to remove pollutants and microbes and clear surfactants
Kupffer cell
Liver tissue macrophages that function to scavenge RBCs and clear particles
Resident kidney macrophage
Kidney macrophages that function to regulate inflammatory responses to antigens filtered from blood
Langerhans cell
Skin macrophages that function in skin immunity and tolerance
Red-pulp macrophage
Spleen macrophage that function to scavenge RBCs and recycle iron
Peritoneal cavity macrophage
Peritoneal cavity macrophages that function to maintain IgA production by B1 B-cells
Lamina propria macrophage and intestinal muscularis macrophage
Intestinal macrophages that function to regulate peristalsis in gut immunity and tolerance
Bone marrow macrophage
Bone marrow macrophages that function to maintain niche for blood cell development and clear neutrophils
Subcapsular sinus macrophage
Lymph node macrophage that function to trap antigen particles
Cardiac macrophage
Heart macrophages that function to clear dying heart cells
Phagocytes ingest exogenous antigens
Macrophages are activated when
Opsonization
Process by which particulate antigens or microbes are rendered succeptable to phagocytosis
Opsonization process explained
Macrophages have receptors for antibodies (Fc receptor) and complement (CR1), then antigen coated with antibody binds to macrophages via recognition by specific T-helper cells and then the antigen undergoes phagocytosis; Makes it easier for macrophage to capture and antigen because of the receptor
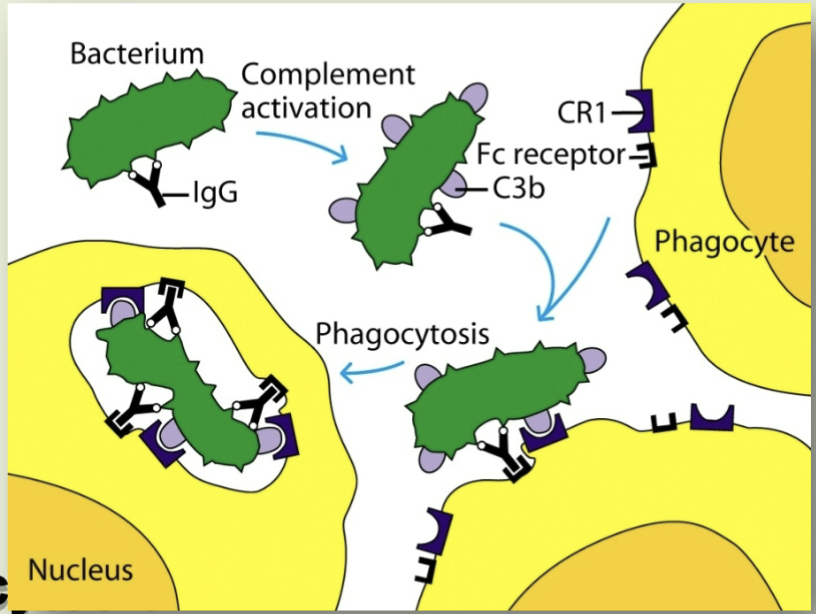
Opsonin
Molecule (either antibody or complement component C3b) that binds to antigens and macrophages thereby enhancing phagocytosis
Complement components (like C3b) and antibodies bind to microbes marking them for destruction
Enhanced phagocytosis occurs when
Neutrophils
First responders at inflammation site (make up 50-70% of circulating leukocytes) that function to kill microorganism
Hypochlorous acid that acts as an oxidizing agent
Neutrophils are the only type of cell that produce what to kill organisms?
Neutrophil structure
Multilobed nuclei that contain granules with microbial a
Neutrophilia
Infection that causes
Eosinophils
Play a crucial role in defending against