Liver , pancreas histology + pathology
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
33 Terms
How is the pancreas divided?
Into exocrine and endocrine portions.
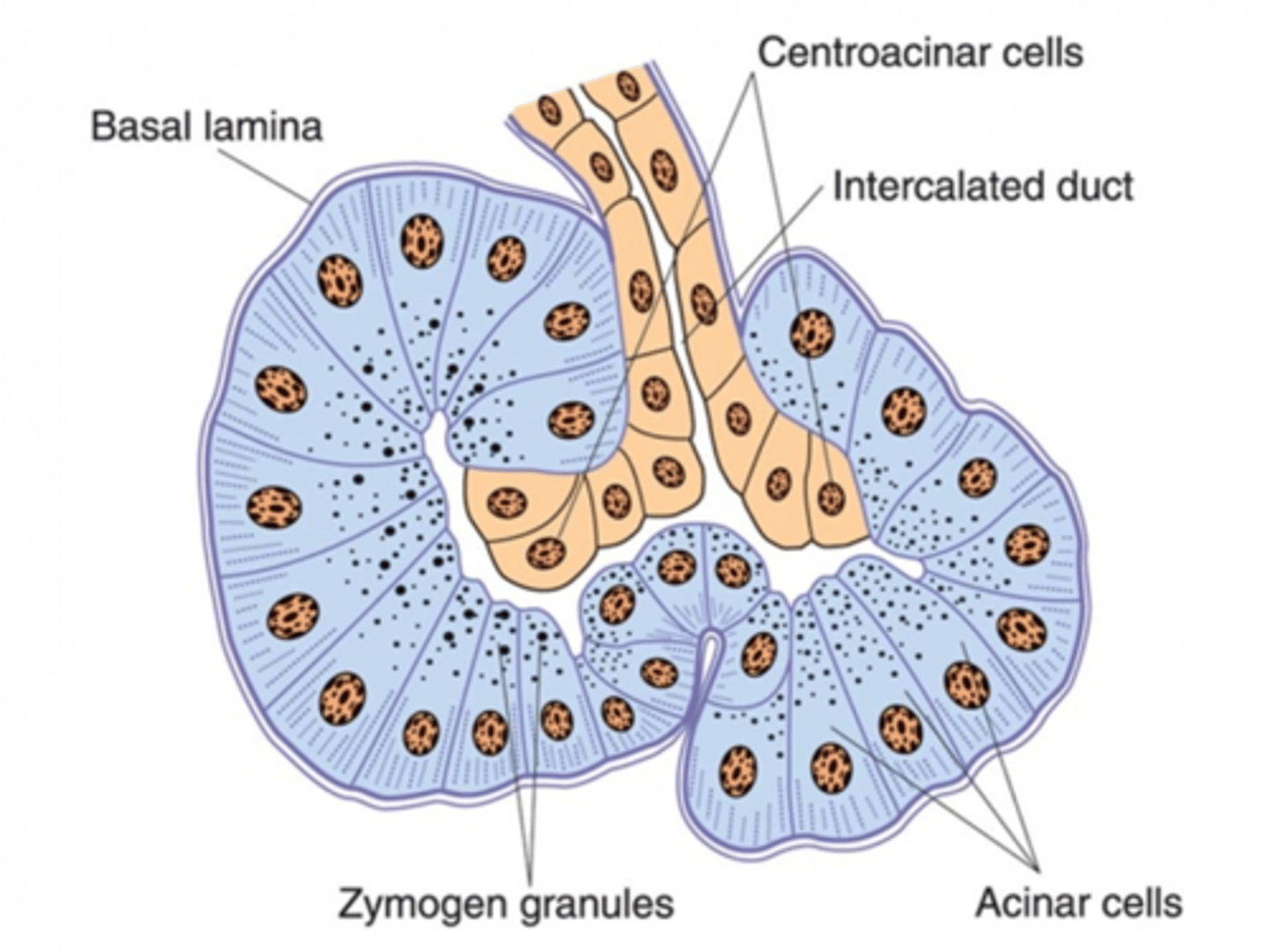
What are acini?
Clusters of columnar secretory cells that surround cuboidal ducts.
What do acinar cells contain in the pancreas? (2)
1. Rough ER and zymogen granules.
2. Digestive enzymes - pancreatic proteases (eg. trypsin and chymotrypsin), pancreatic amylases and lipases.
How is autodigestion in acinar cells prevented?
Secretions are:
1. packaged
2. inactive.
What is the function of duct epithelial cells in pancreatic acini? (2)
1. Secrete HCO3- to control pH in relation to HCl.
2. Produce water.
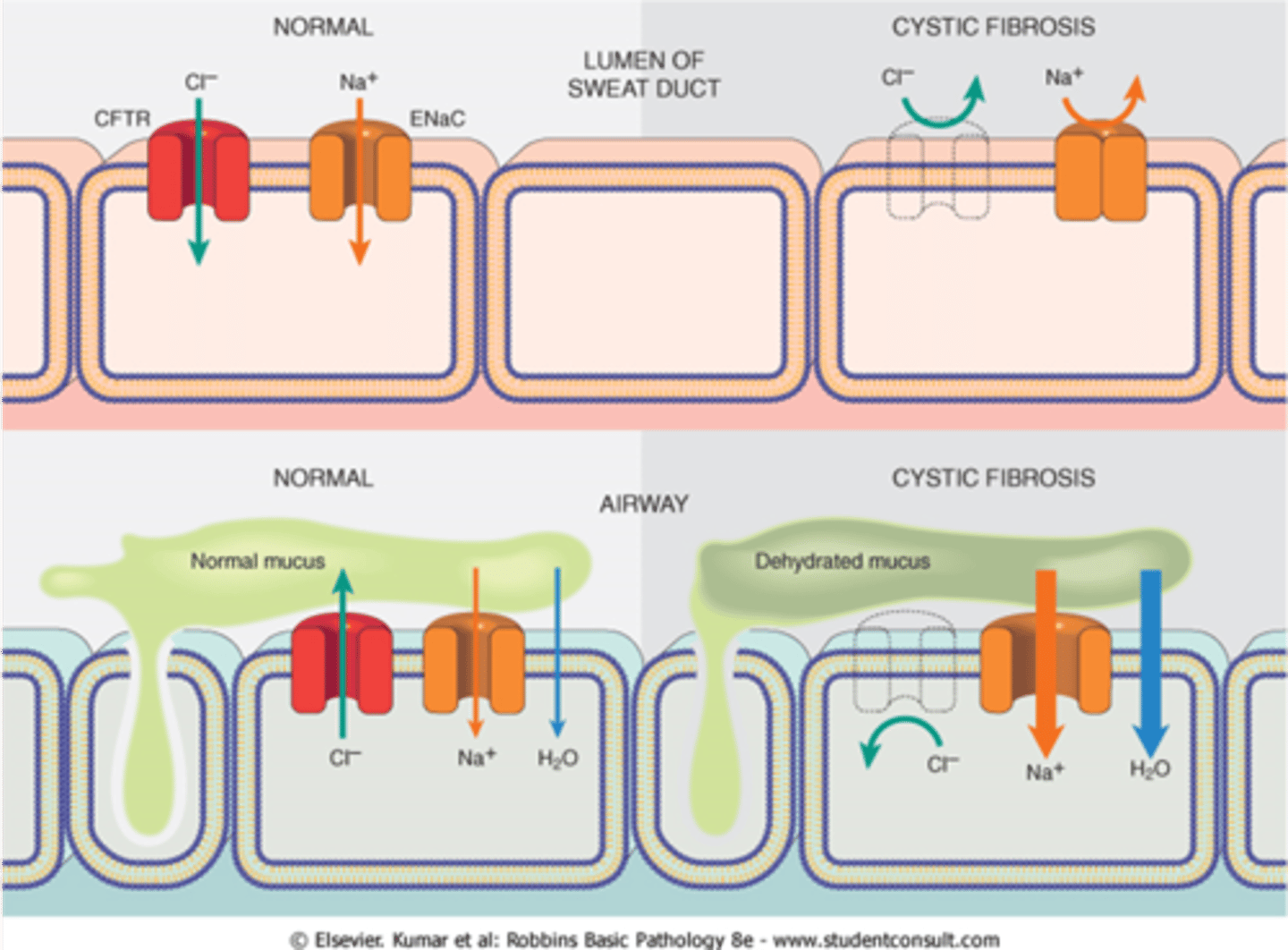
What is cystic fibrosis? What and where does it affect? (4)
1. Autosomal recessive disease, mutation of CFTR gene on chromosome 7, a chloride channel - defective Cl- transport.
2. Affects secretion of exocrine glands.
3. Manifests differently across body (sweat is different in GI and resp systems).
4. Mostly affects respiratory and alimentary, causing abnormally viscoid mucus.
How does abnormal mucus from CF affect different areas of body? (4)
1. Lungs: mucociliary elevator; infection and bronchiecstasis
2. Pancreas: clogs ducts and glands, insufficiency causes fibrosis and protein and fat malabsorption > fat-soluble vitamin deficiency.
3. Liver: clogs bile canaliculi > cirrhosis.
4. Reproductive tract.
What is the mechanism of CF in a) sweat glands and b) respiratory/pancreatic epithelium?
Sweat glands: Na + Cl secreted but no reabsorption of Cl- due to CFTR mutation, salty sweat.
Resp/pancreatic epithelium: less active transport of Cl- due to CFTR mutation and more Na into cell. Water follows > dehydrated mucus.
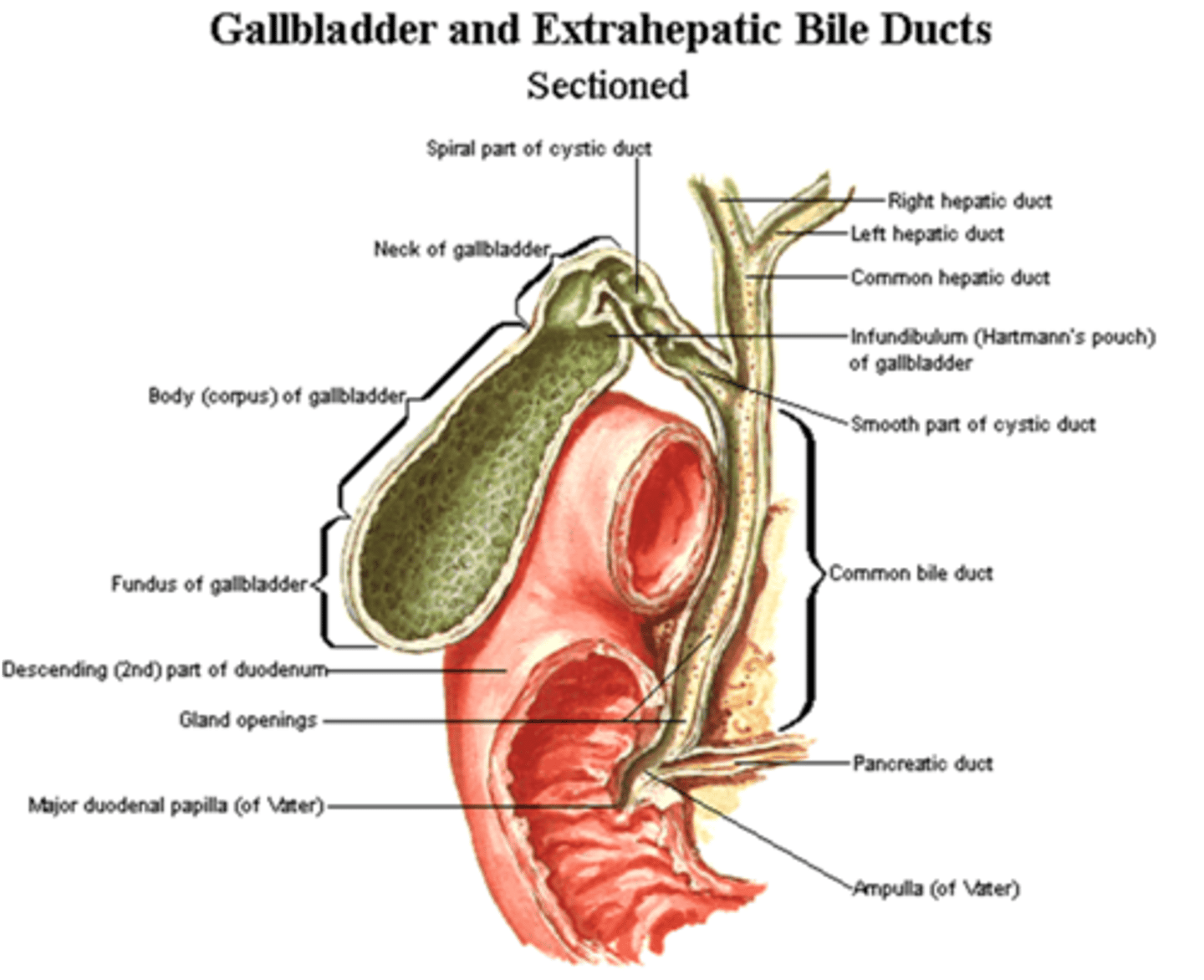
What does the biliary system consist of? (2)
Ducts from liver to duodenum and gallbladder. CCK release in duodenum stimulates gallbladder contraction and relaxes Sphincter of Oddi.
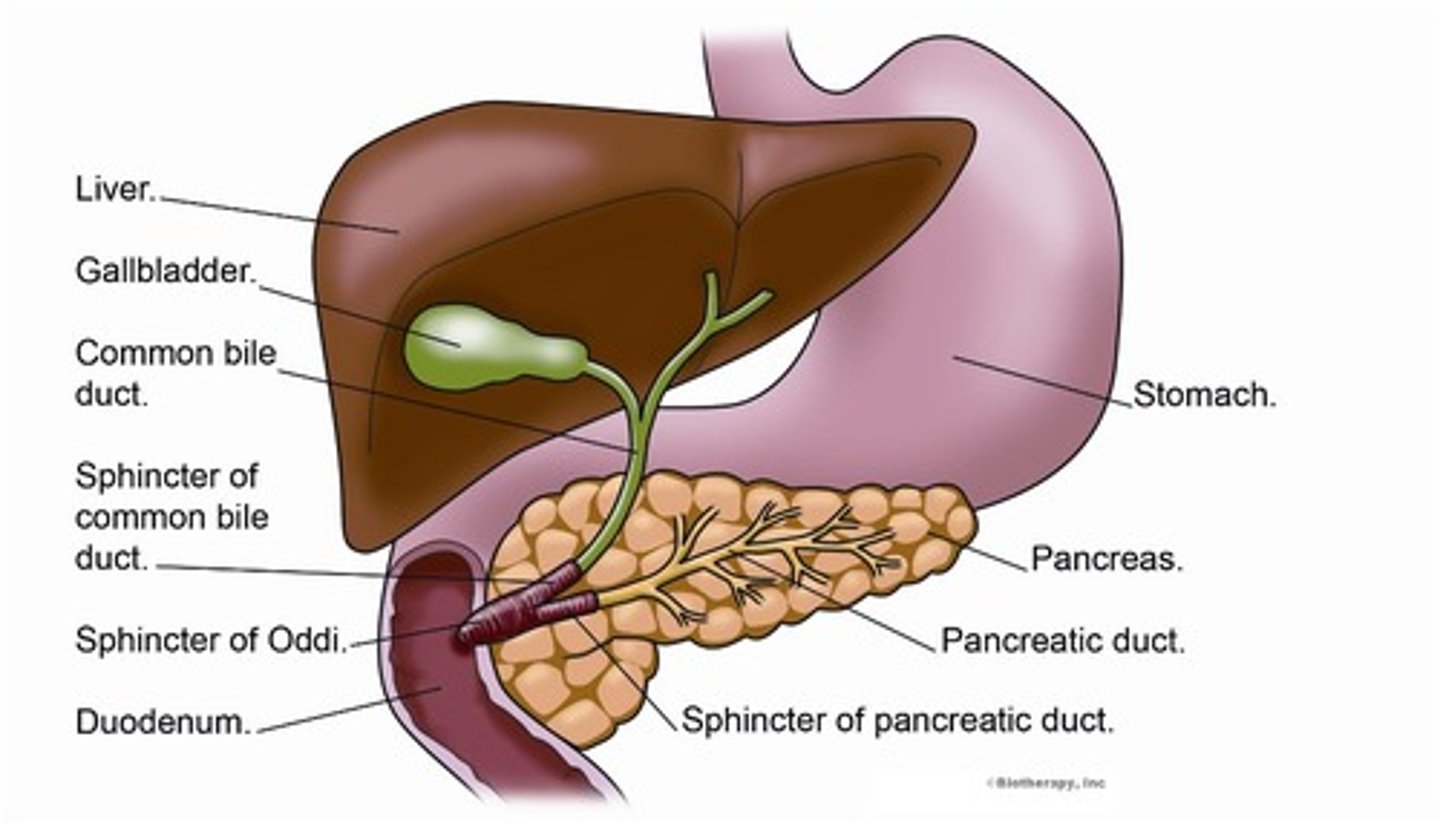
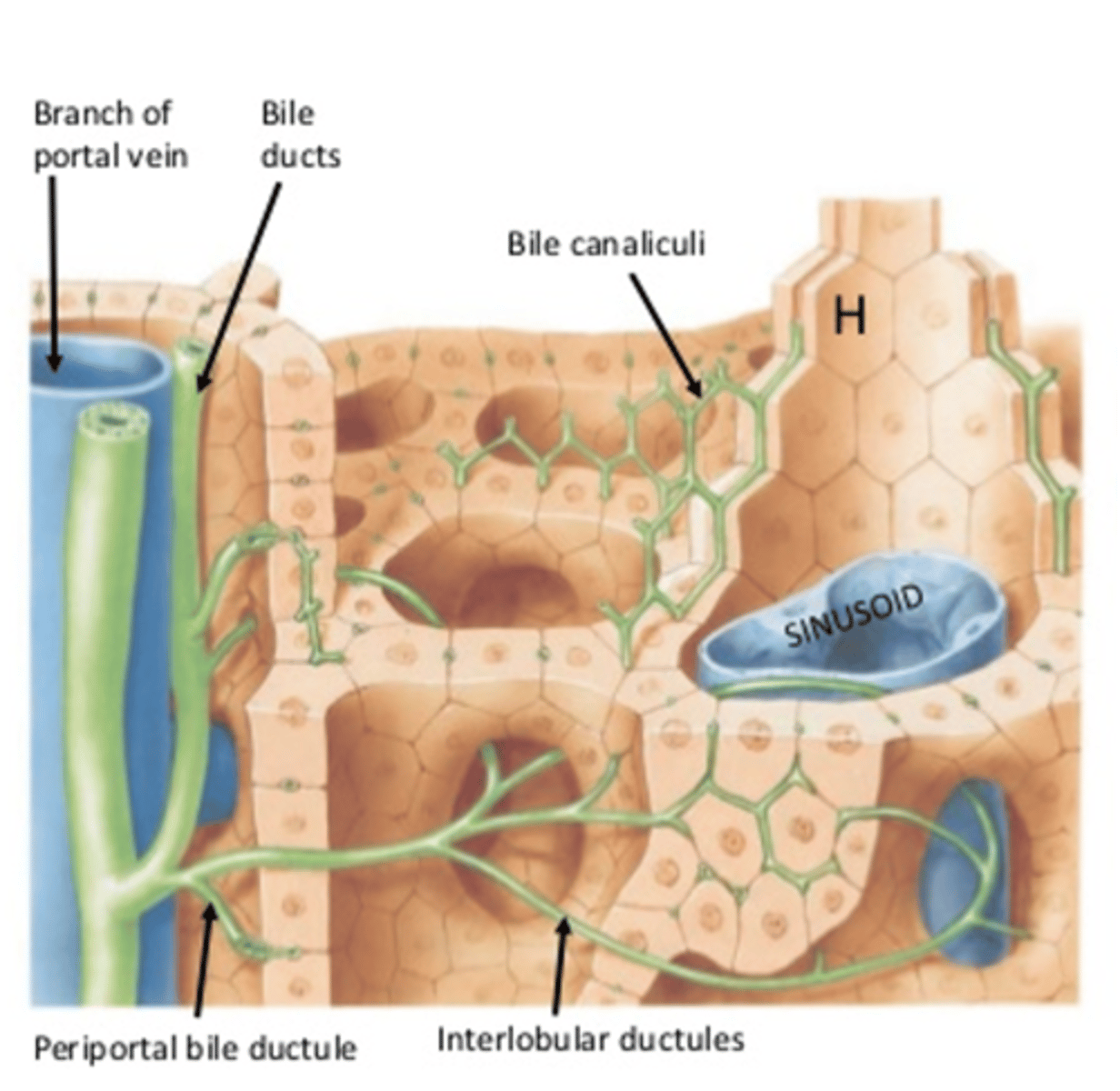
What is the route of bile from the liver?
Bile from hepatocytes is secreted into canaliculi > combine to form bile ductules > portal tracts > common hepatic duct.
What is bile? What does it contain and where is it released? (3)
1. Needed for emulsification of fats and fat absorption.
2. Contains water, bile salts (Na, Cl, K, HCO3-), bilirubin and cholesterol.
3. Released into duodenum via common bile duct to be absorbed and recycled.
What is bilirubin?
From senescent RBCs (breakdown product of haeme),
What happens to bilirubin in jaundice?
Binds to elastic tissue and causes them to appear yellow (skin, sclera).
What does it mean by the gallbladder concentrate bile?
Hepatocytes make 1L/day of bile
Gall bladder stores 50ml of concentrated bile. Concentrates bile by absorbing water, making the store bile more potent for aiding in fat digestion
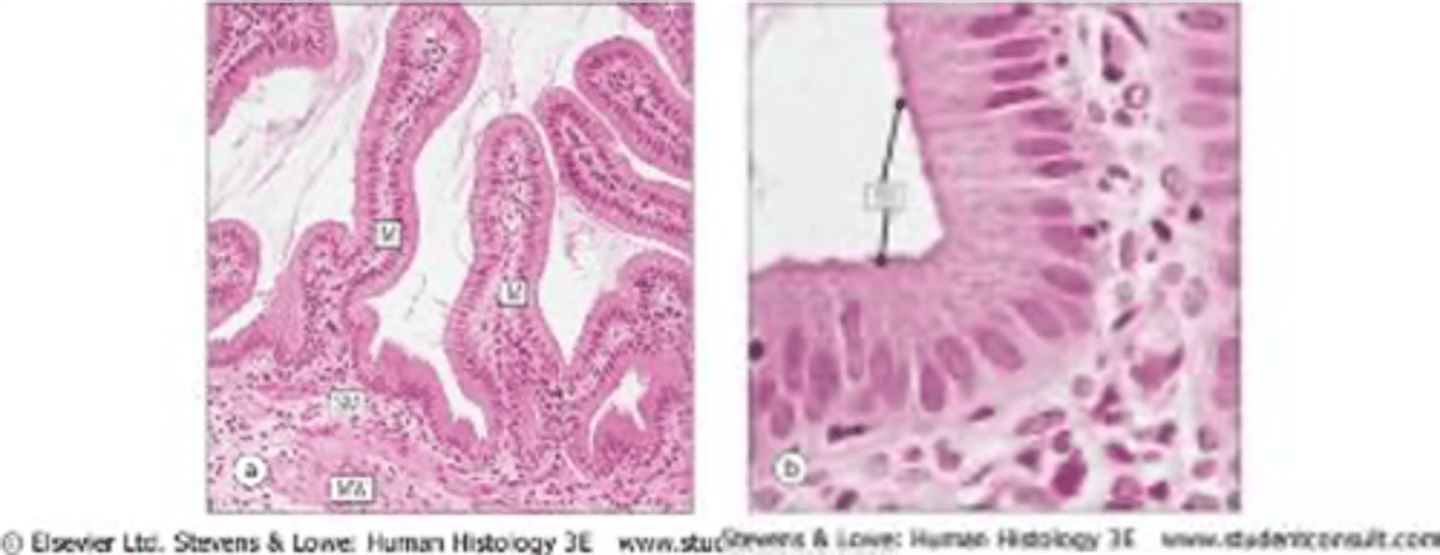
How is the gallbladder adapted to function? (3)
1. Muscular walled sac.
2. Epithelium - highly folded w/ microvilli, adapted for salt + water absorption.
3. Proton pumps pump out Na/Cl and osmotic gradient draws water into cells and enters capillary net.
How does cholestasis result?
Reduced bile flow (eg. stone obstruction) or synthesis (eg. hepatocellular damage) causing bile to accumulate in canaliculi > rupture > damage to hepatocytes > accumulate in blood > jaundice.
Where is the liver located?
right hypochondriac and extends across epigastrium into left hypochondrium
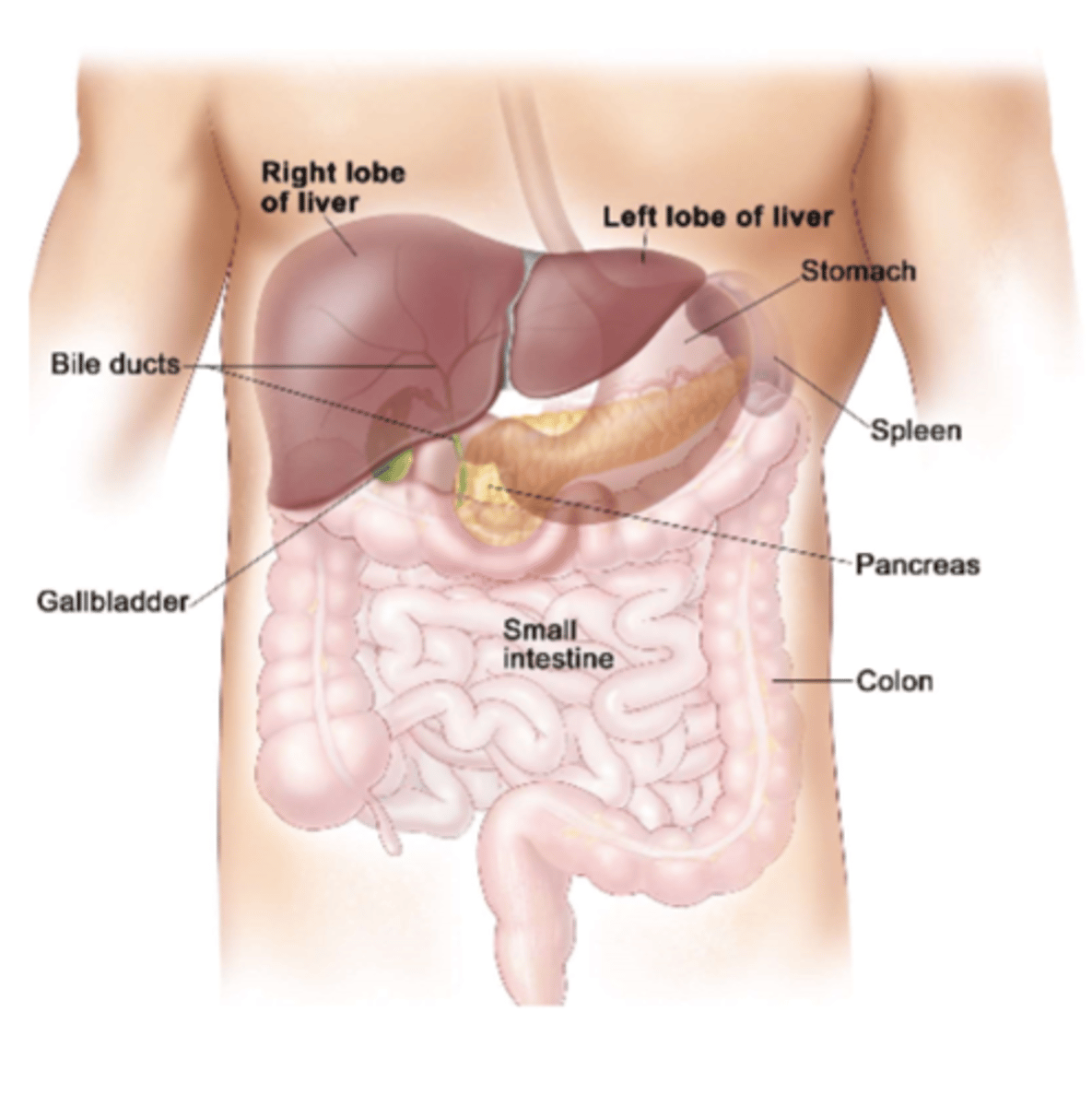
What is the function of the liver?
Bile synthesis and secretion for digestion of fat
Excretion of bilkirubin (breakdown product of haeme)
Metabolism: protein, carbohydrates, lipid, storage of vitamins, glycogen, copper and ion
Detoxification: conjugation and elimination of metabolites and toxins
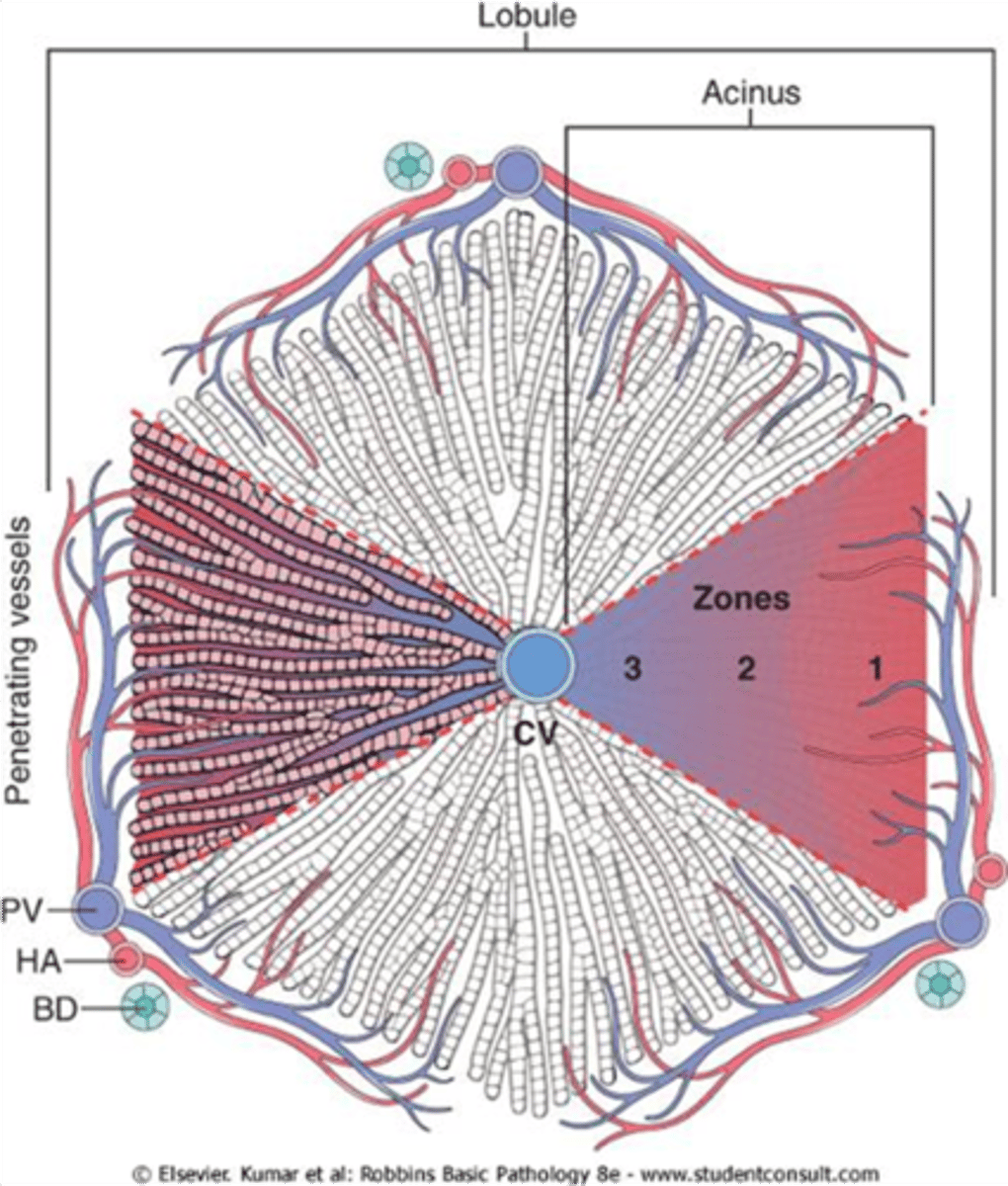
How is the liver structured?
Hepatocytes interact with blood in the sinusoidal capillaries, producing bile. Contain lobule and portal triad on apex.
What is the hepatic portal circulation- alimentary venous and fresh arterial blood supply the liver?
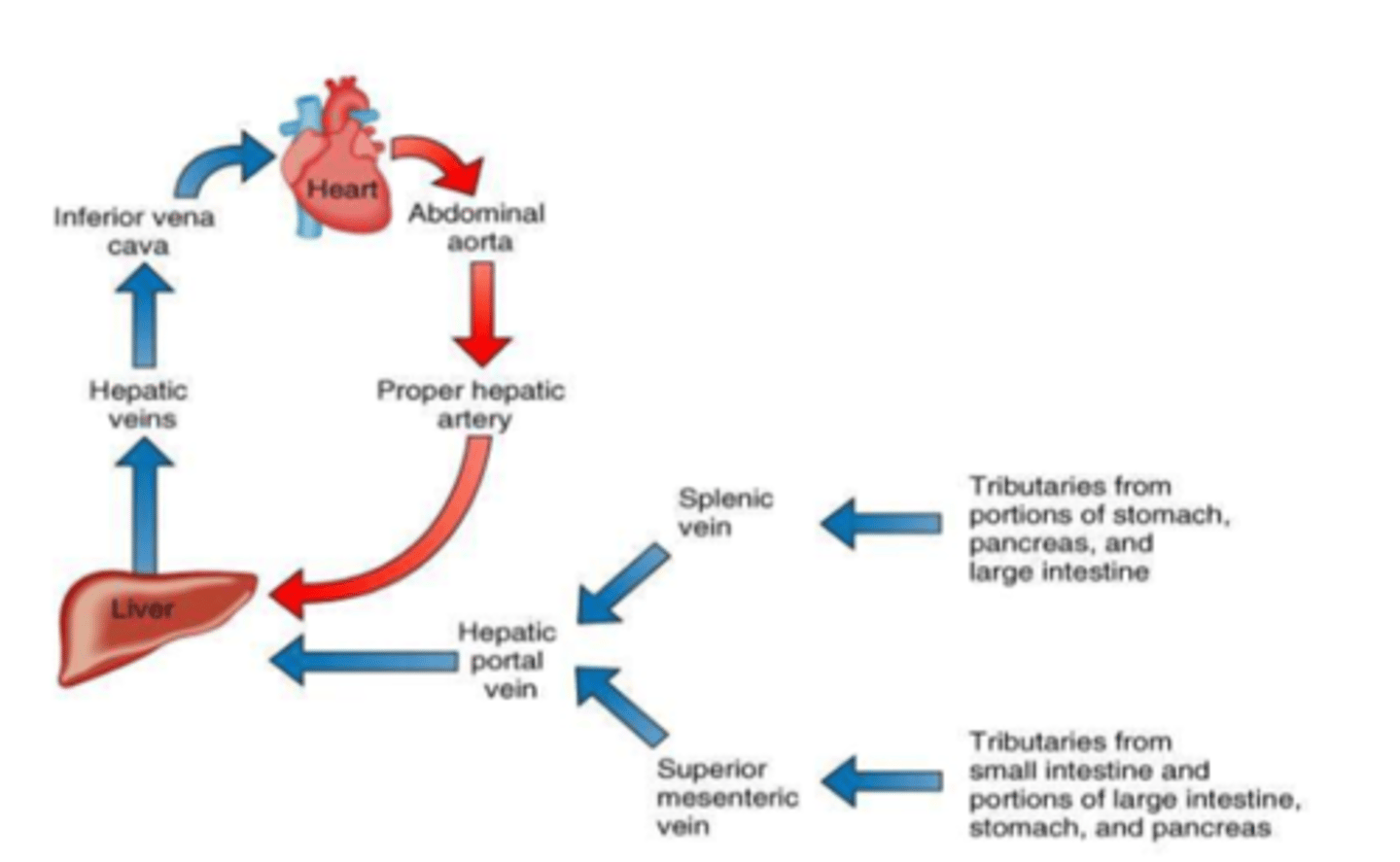
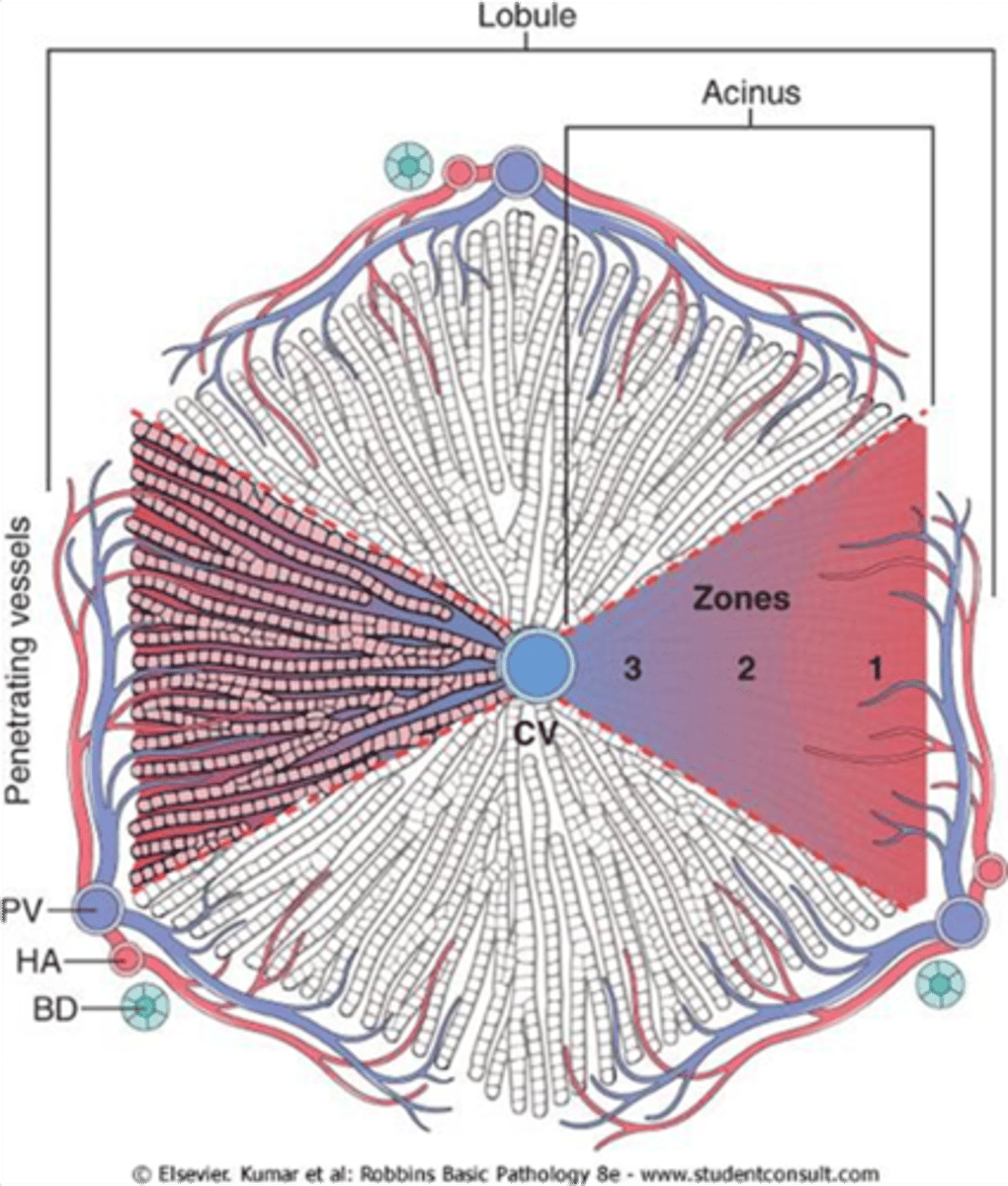
Where does the blood flow in liver?
Along portal/sinusoidal tracts into a central venule.
Which zone is initially expoed to circulating drugs eg. toxins?
Zone 1 - closest to edge.
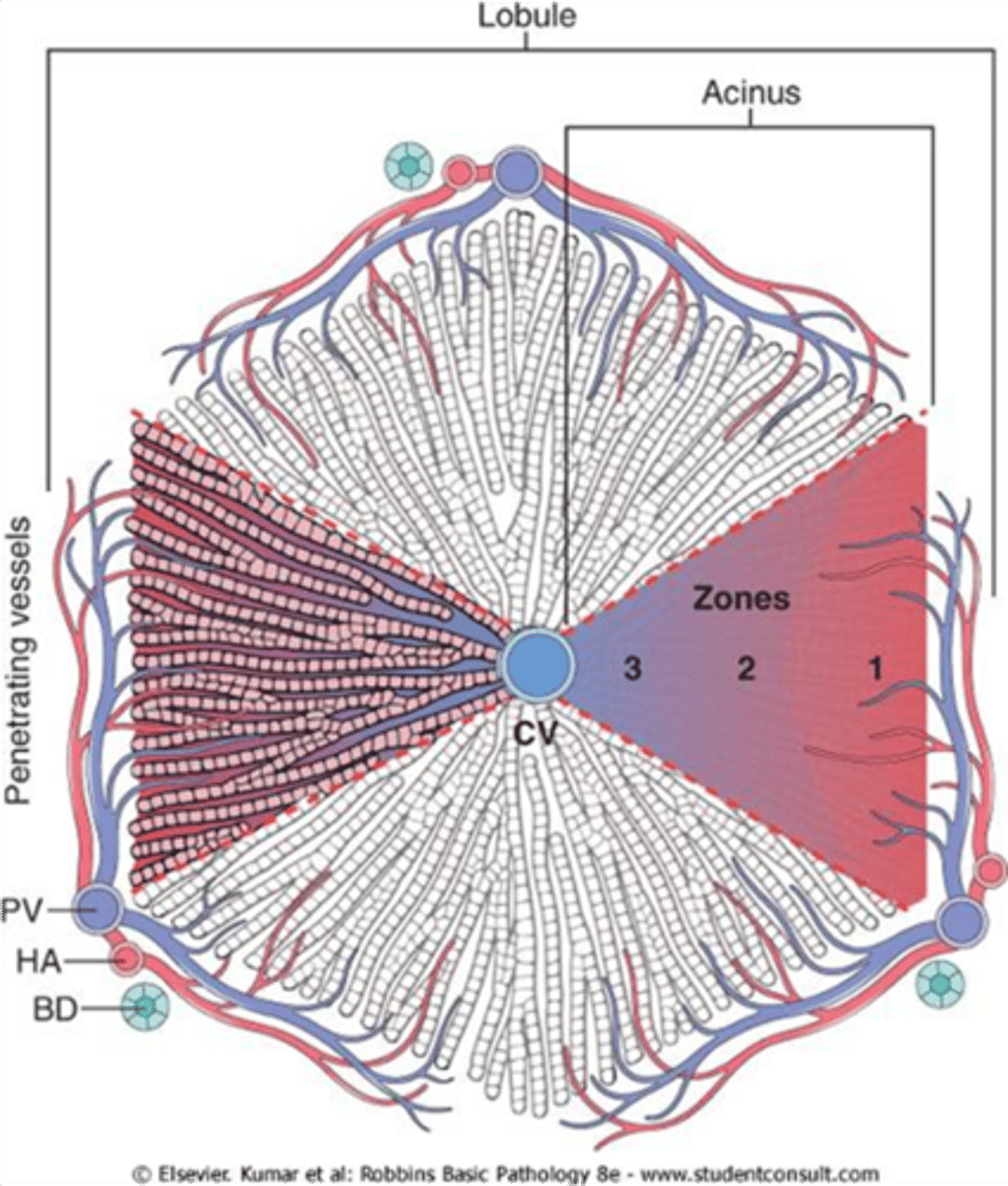
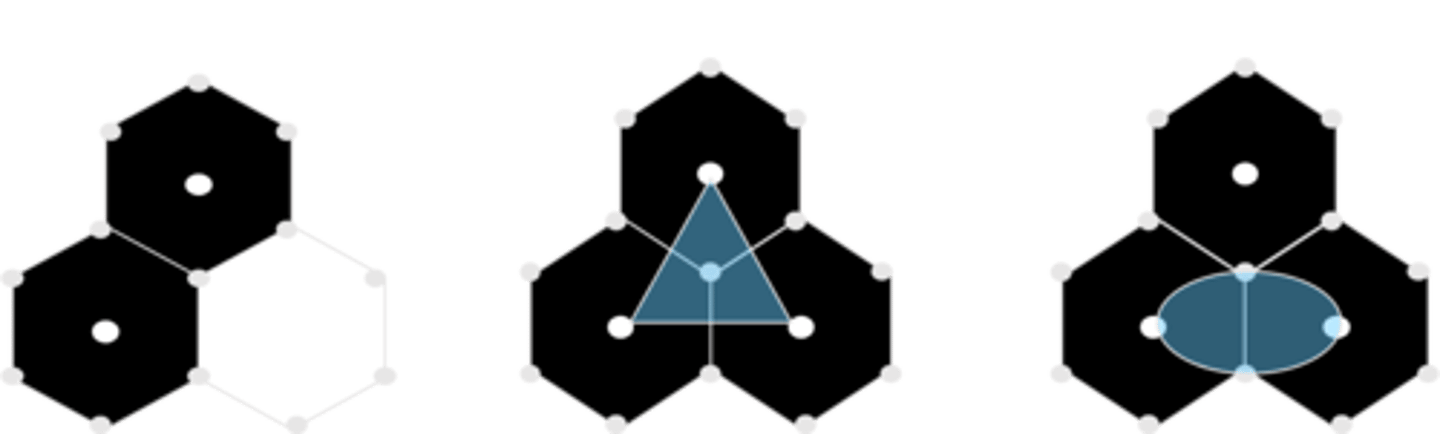
What 2 things can a liver be organised into?
1. Lobule (classic, 6 sides)
2. Liver acinus (last picture).
Which zone has highest conc of oxygenated blood?
Zone 1.
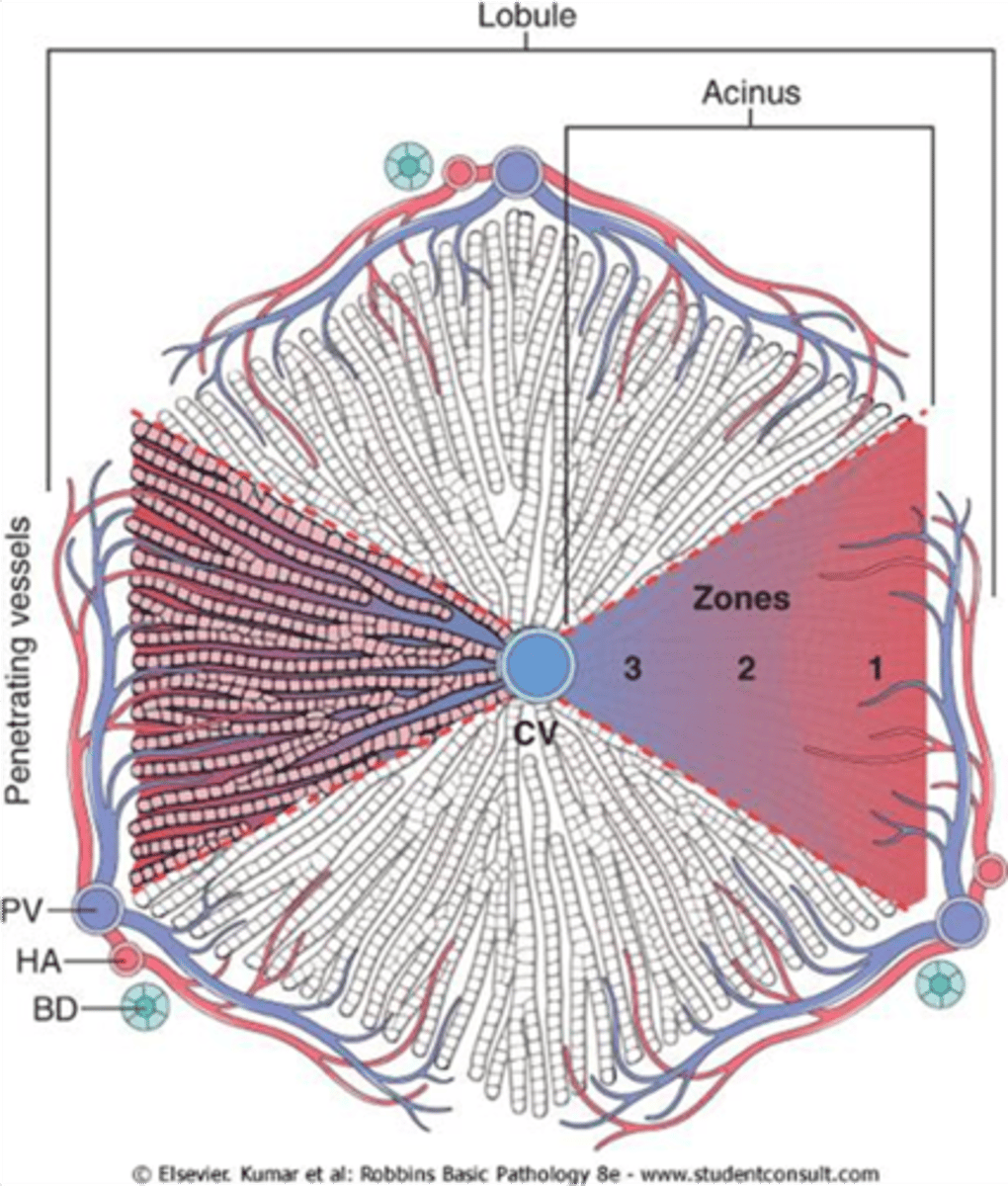
If O2 is withdrawn which cells will die first?
Zone 3 is affected first - not brilliantly oxygenated so most vulnerable to ischaemia. Cells dying at zone 1 suggest toxicity.
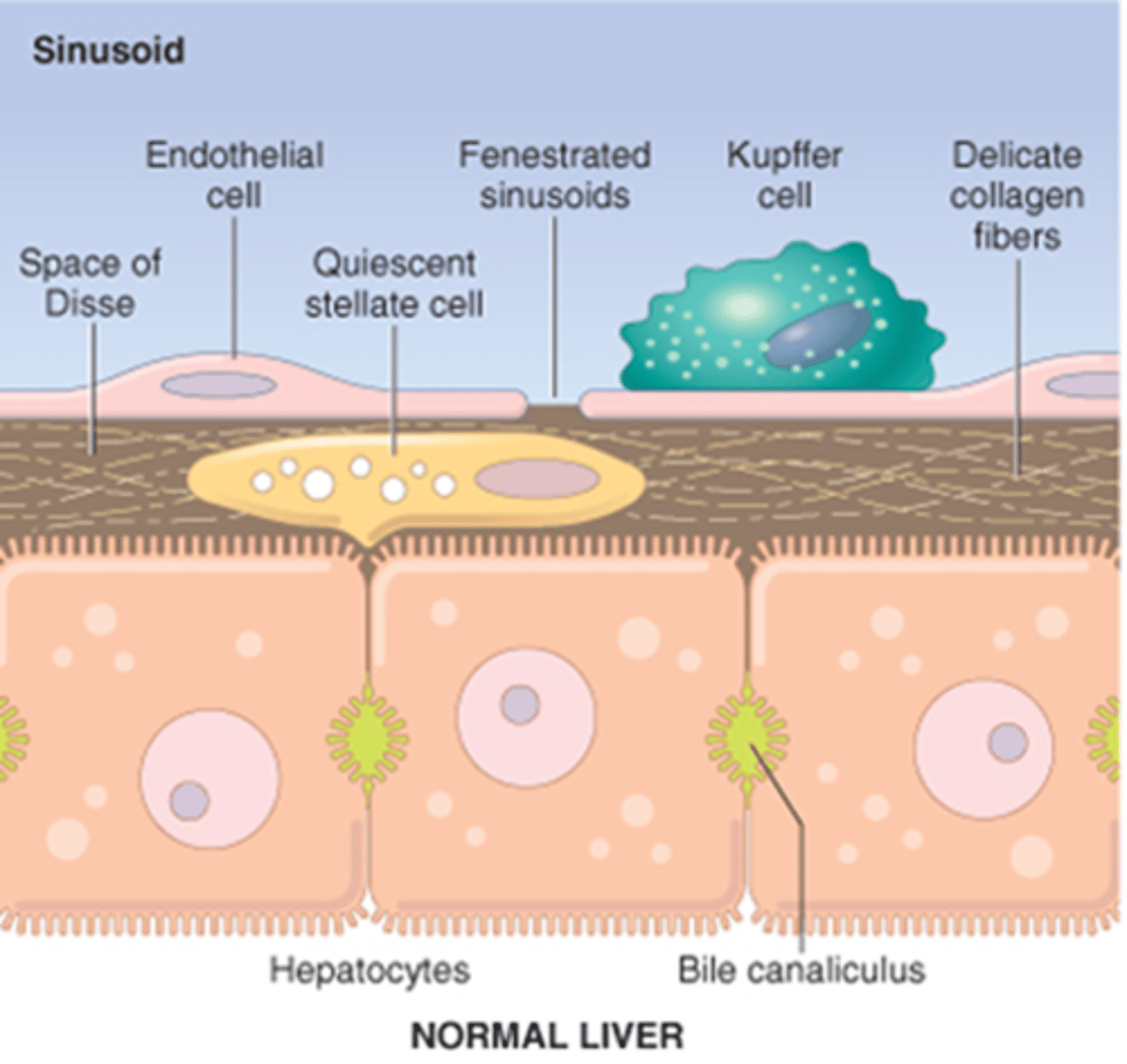
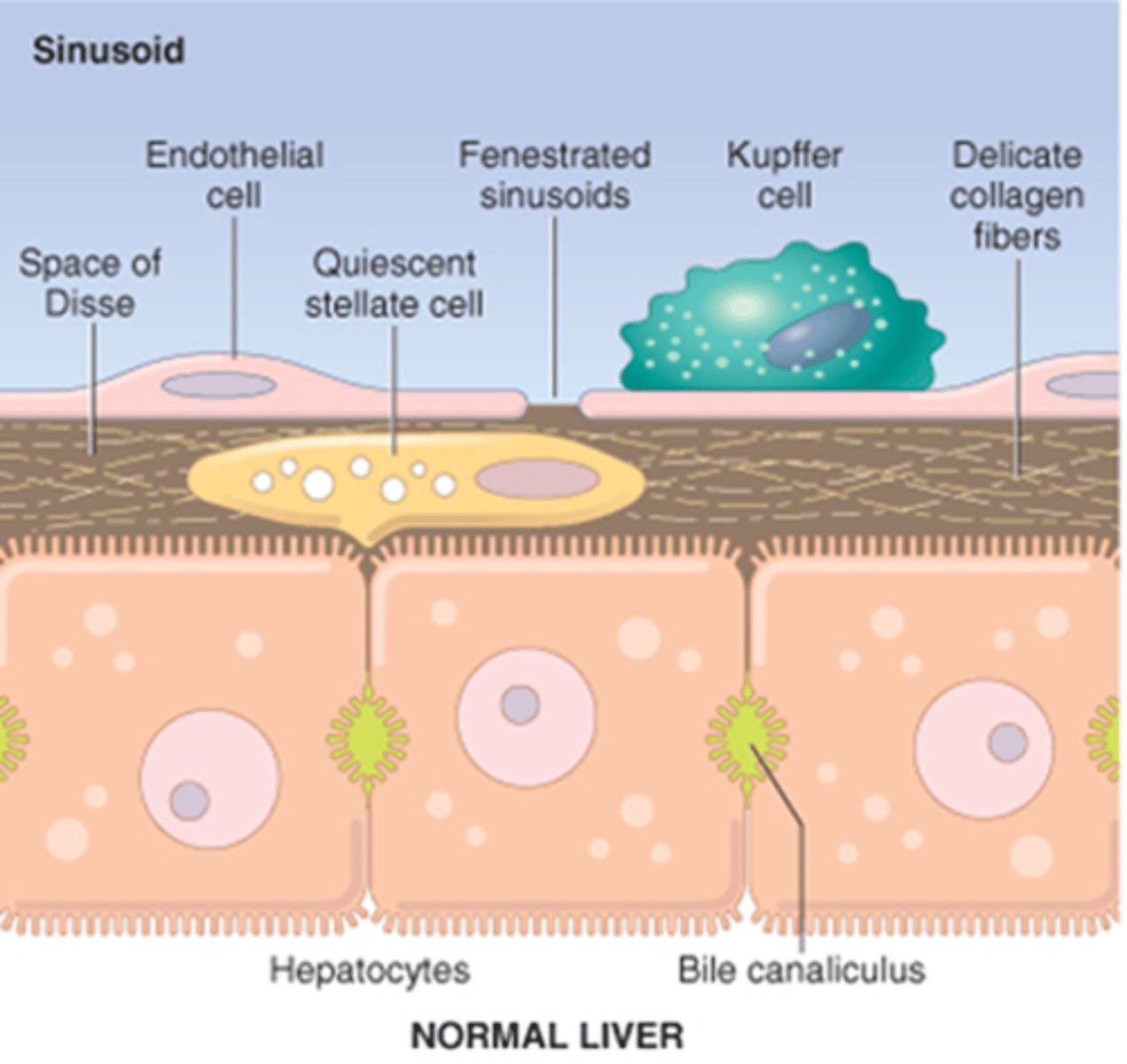
Outline the cells in the liver. (4)
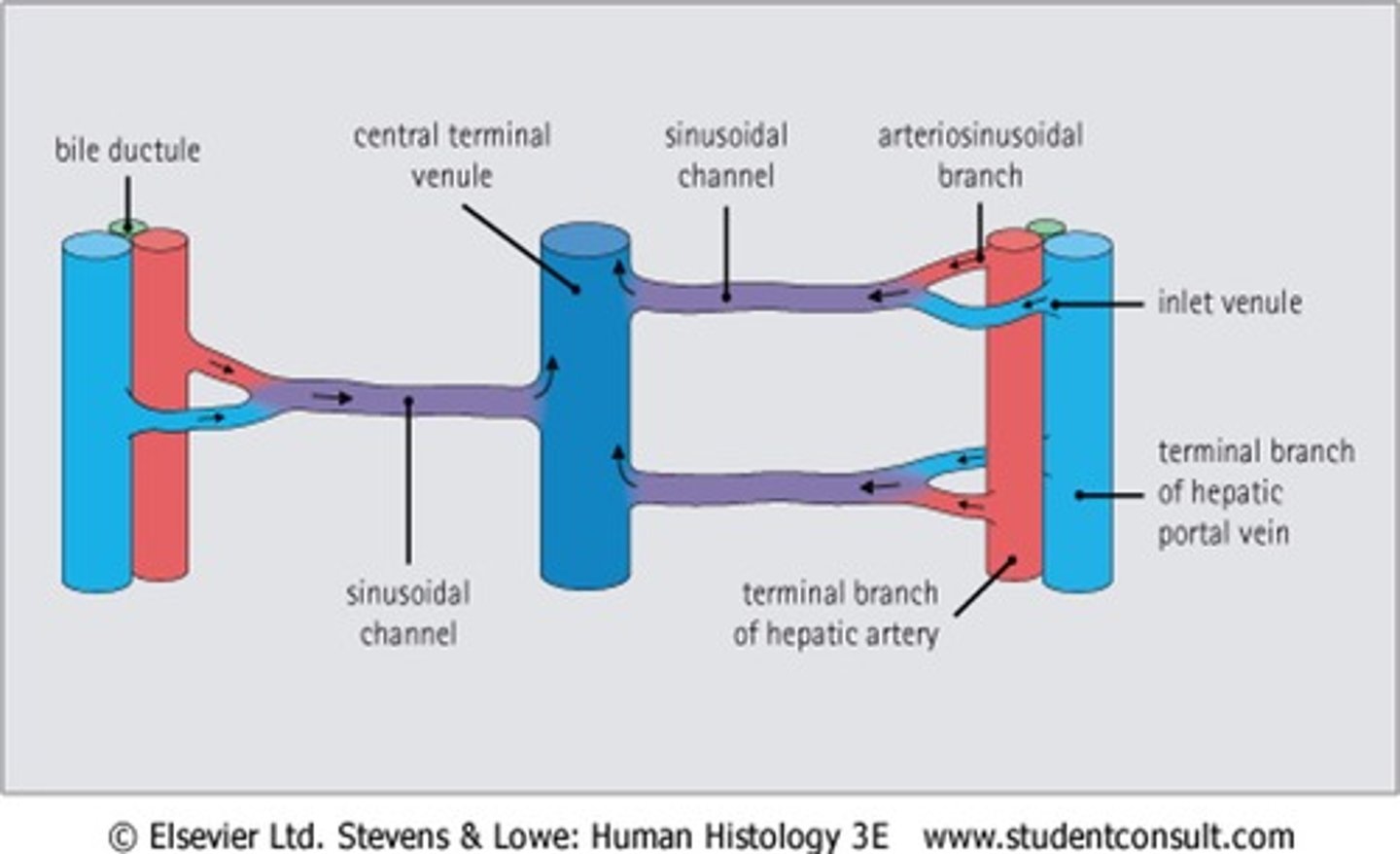
1. Hepatocytes: cords of cells separated by sinusoids, have microvili on apical and basal surfaces (sinusoidal facing) and bile canaliculi between adj. cells.
2. Sinusoids: leaky capillaries lined by endothelial cells and Kupffer cells.
3. Kupffer: phagocytic (bacteria and old/damaged blood cells).
4. Ito cells: stellate cells storing vit A in lipid droplets in cytoplasm. Are myofibroblasts and do fibrosis and are APCs.
What is the pathology in liver cirrhosis? (4)
1. Alcohol absorbed from stomach > acetaldehyde, toxic to liver cells.
2. Slowly progressive > chronic liver failure.
3. Hepatocytes die > scarring > damage between cells and bile system. Cells still function but reduced and eventually demand takes over supply > liver failure.
4. Ends in hepatic coma or complications of portal hypertension.
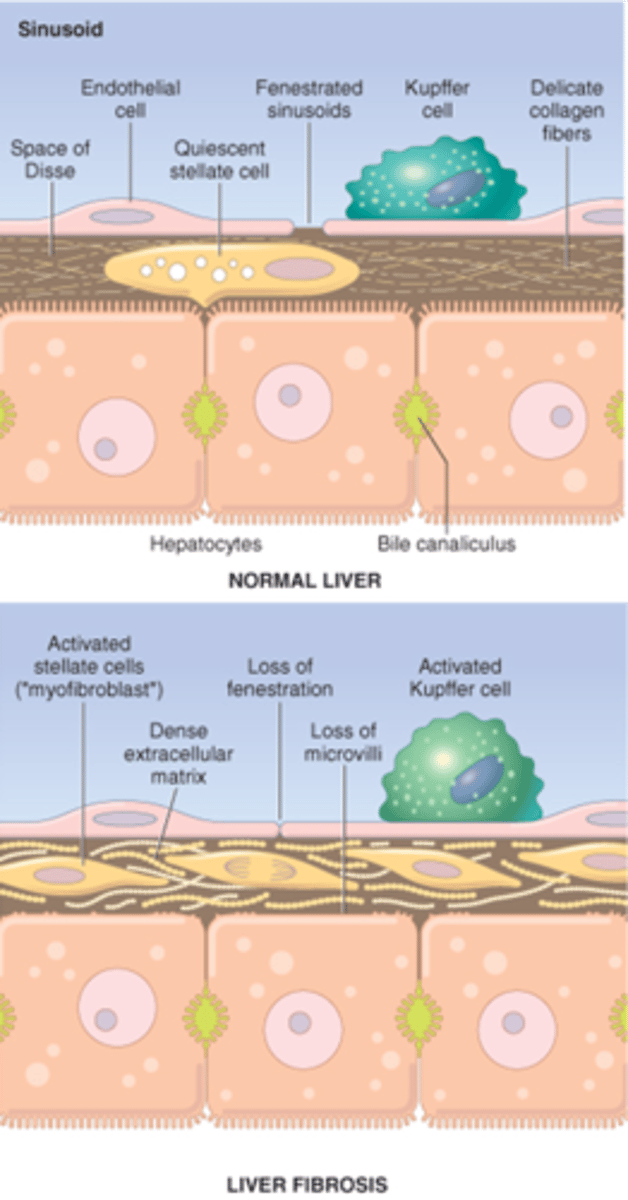
What is the Space of Disse?
Contains collagen fibres - collagen 3. Between hepatocytes and blood vessels. If scarring occurs, blocks comms between bile and capillaries.
List different types of liver diseases? (8)
1. Hepatitis
2. Hepatocellular carcinoma
3. Alcoholic liver diease
4. Cirrhosis
5. Vascular disease
6. Portal hypertension
7. Liver failure
8. Cholestasis.
What is portal hypertension? (3)
1. Sinusoid destruction so portal vv blood can't escape > increased Pa.
2. Only escape is via anastamoses with systemic venous system, which open under high Pa > distention > varices.
3. Happening at lower end of oesophagus can bulge into lumen and be eroded by gastric acid > torrential haemorrhage (fatal).
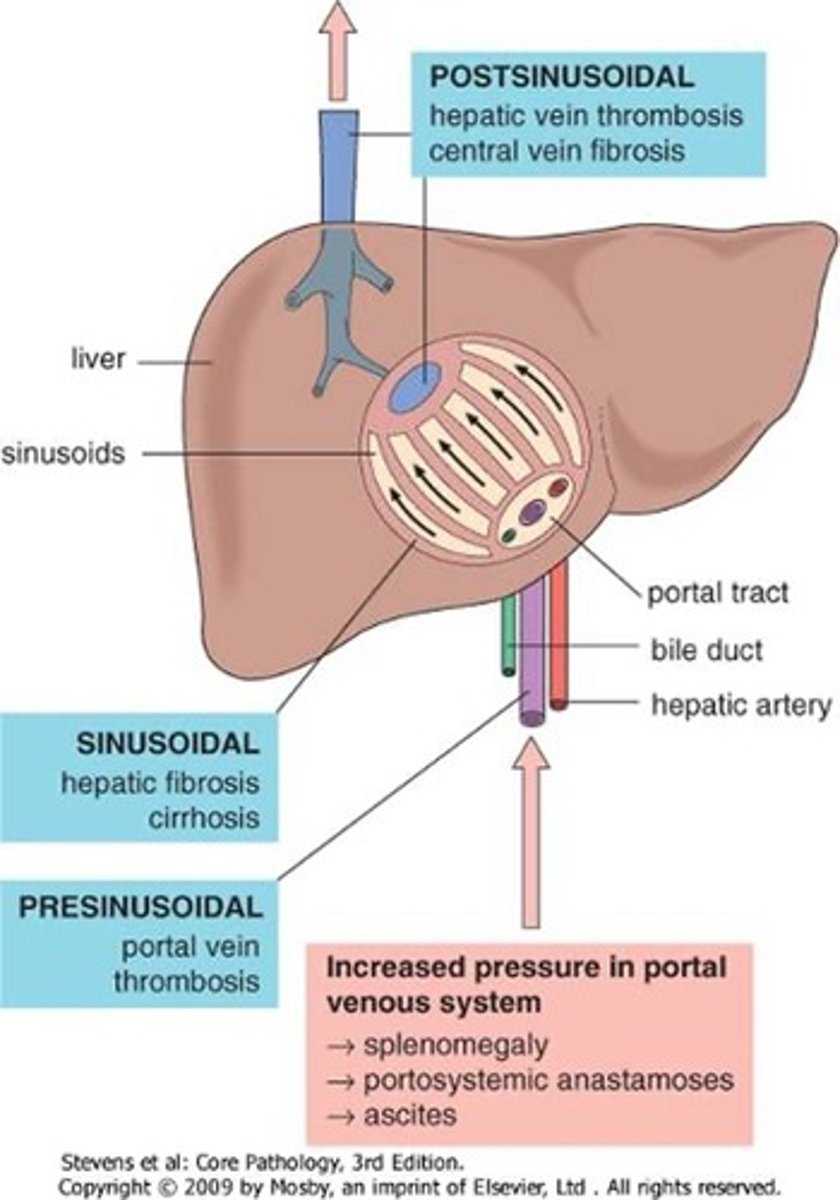
Why can cirrhosis and portal hypertension occur? (4)
Persistent hepatocyte destruction due to:
1. Alcohol toxicity
2. Viral infection (hep B and C)
3. Autoimmune liver disease
4. XS iron/copper
What are the consequences of liver failure? (4)
1. Synthesis failure > albumin (oedema and ascites) and clotting factors (spontaneous bleeding).
2. Detoxification failure > neuropsychiatric symptoms.
3. Failure to secrete bile > jaundice.
4. Acute/chronic > chronic due to cirrhosis, acute can lead to severe + sudden death of hepatocytes due to viral infection or Paracetamol toxicity.
How can hepatocellular tumours occur? (3)
1. Primary tumours aren't common - hepatocellular carcinomas can arise due to cirrhosis.
2. Metastatic tumours are common - from GI system via portal system and via blood (lung and breast).
3. Biliary tree tumours are rare - adenocarcinoma.