oral modified release drug delivery systems
1/45
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
46 Terms
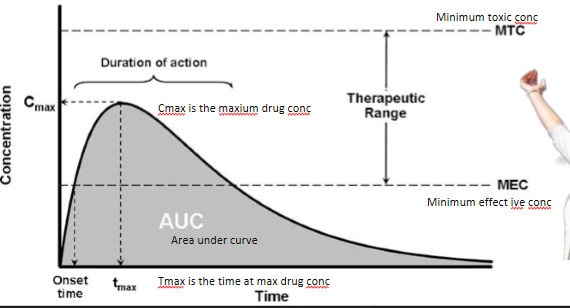
define the limits of therapeutic range
above the minimum effective concentration
below the minimum toxic concentration
what happens if the drug concentration exceeds minimum toxic concentration
side effects will be experienced
what is the main function of the intestine
to extract nutrients and absorb them
what is the difference between immediate release (IR) or modified release (MR)
IR is when the drug is released faster so quicker onset
MR is when the drug is released slower and delayed so drug is released further down GIT
official definition of modified release systems
where formulations are prepared using substances or procedures (which separately or together) are designed to control the rate or place at which active ingredients are released in GI tract
name the 2 types of oral modified release systems
delayed release DR
extended release ER
true or false: delated release systems are also known as gastro-resistant or enteric systems
true
how do delayed release systems work
thin coating is applied to tablet/capsule/pellet surface
coating delays the release of drug to small or large intestine
what factor determines when the drug is released from tablet
pH of the delayed release coatings
at what pH would the drug be if target is:
small intestine
stomach
large intestine
small intestine = pH > 5-6
stomach = pH 1.5
large intestine = pH > 7
if you want to deliver drug to [first/end] part of small intestine, then use coating which dissolves at pH 5.6-6
if you want to deliver drug to [first/end] part of small intestine, then use coating which dissolves at pH 7.4
if you want to deliver drug to [first/
end]part of small intestine, then use coating which dissolves at pH 5.6-6if you want to deliver drug to
[first/end] part of small intestine, then use coating which dissolves at pH 7.4
what functional group do all pH sensitive polymers have
carboxylic acid
what happens to the carboxylic acid group of polymers at:
low pH in the stomach
higher pH in the intestine
low pH in the stomach - COOH remains unionised so does not dissolve
higher pH in the intestine - ionises and becomes COO- so dissolves
examples of pH sensitive polymers
polyvinyl derivatives
polymethacrylates
how do enteric coated systems for delayed release targetting the colon work
the drug and tablet remain intact until the start of the large intestine where enteric coating dissolves and drug enters and is carried throughout large intestine
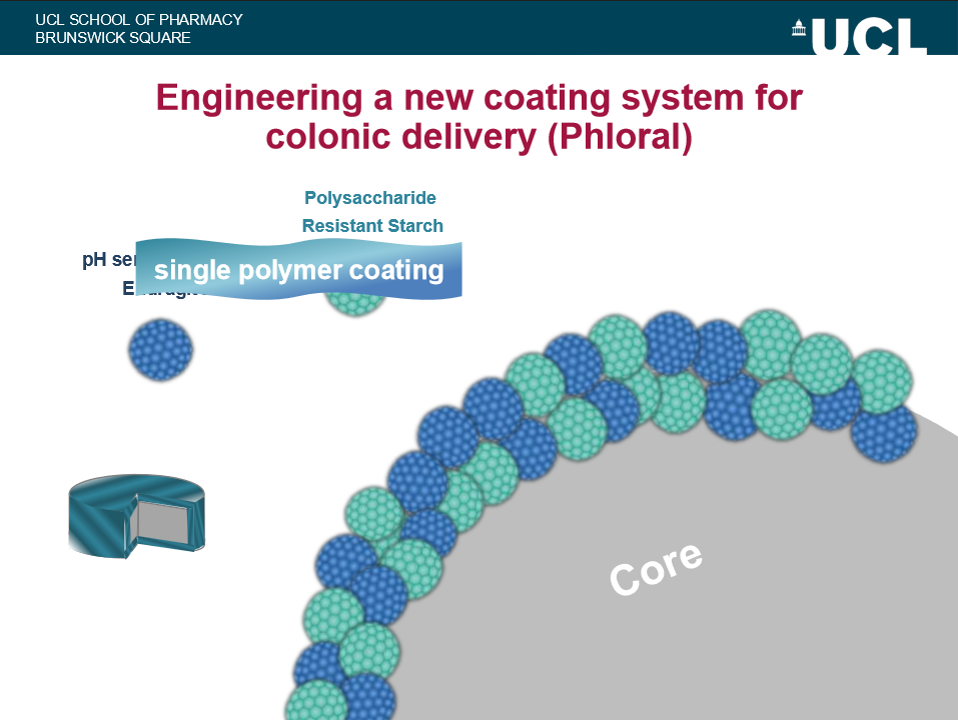
what is Phloral colonic coating
dual trigger coating system designed to deliver drugs to colon specifically by combining pH sensitive release (responds to intestinal pH) and microbiota triggered release (responds to colonic bacteria)
what are the 2 components that make up the Phloral outer coating
pH-sensitive polymer (e.g. Eudragit)
insoluble in stomach and small intestine
dissolves at pH < 7
acts as the first trigger
polysaccharide (e.g. resistant starch)
not digested in upper GI tract
specifically broken down by colonic bacteria
acts as second trigger
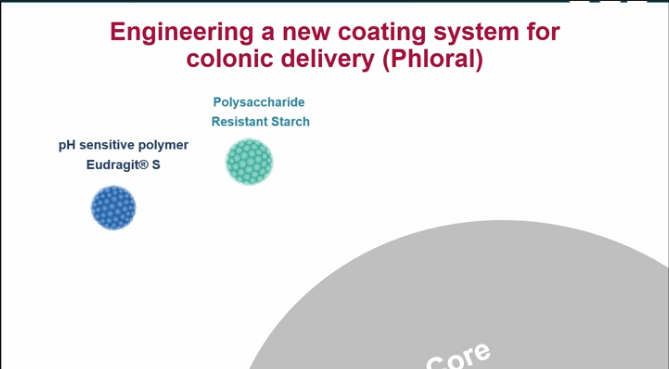
true or false: the 2 polymers in Phloral outing coating are mixed together into a single coating layer
true - not 2 separate coats
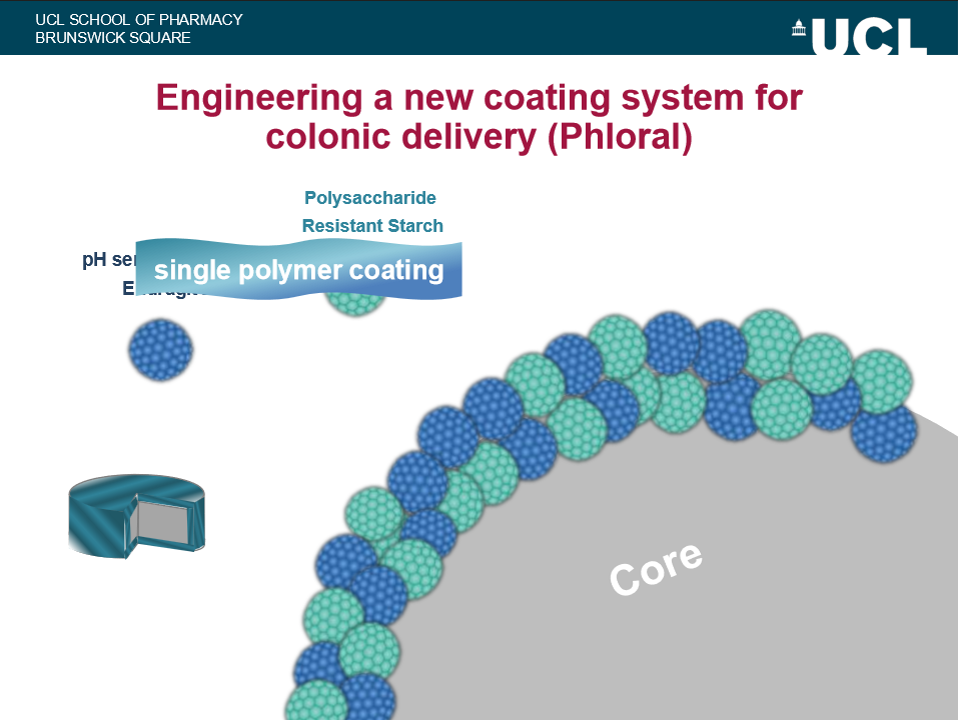
advantages of Phloral outer coating vs normal coating
two independent triggers so more reliable targetting
reduces premature drug release due to variable gut pH
ideal for GI disorders lower in GIT e.g. ulcerative colitis, Crohn’s colitis
what is the purpose of extended release systems
to reduce frequency of dosing
advantages of extended release systems
maintenance of therapeutic plasma levels
improved patient compliance
economics
what are some synonymous names of extended release
controlled release
sustained release
prolonged release
slow release
what does the conc-time graph for extended release drug systems look like
define half life
rate of elimination of drug from the body
how quickly drug is metabolised by liver
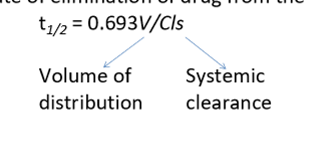
what is the ideal half life range for drug
4-6hrs
why is it difficult to formulate drugs into MR system if drugs have half life < 2hrs
because large doses would be necessary
why does a half life of 8hrs mean its unnecessary to modify drug into MR system
because it already naturally takes a long time to be metabolised
what are the disadvantages of extended release systems
drugs with absorption windows
drugs with short half lives
variable conditions/transit time through GIT
size of formulation
dose-dumping
expensive
what is an absorption window
some drugs are only absorbed efficiently in specific region of GIT like stomach or duodenum - this region is called absorption window
why are absorption windows a limitation for ER systems
ER systems are designed to release drug slowly along whole GIT
once drug moves past absorption window, any drug later is poorly/not absorbed
reduces bioavailability and increases variability between patients
why are short half life drugs a limitation for ER systems
because ER releases drug slowly so the drugs with short half lives are eliminated faster than released and plasma levels may not reach therapeutic levels
how can transit time affect drug release
rapid transit
slow transit
pH variation
Rapid transit → incomplete drug release
Slow transit → risk of over-release
pH variation → coating dissolves too early or too late
why are ER tablets/capsules larger in size
because ER systems require:
large amounts of polymer
multi layers
this means difficulty swallowing and not suitable for elderly or paediatric patients
what is dose dumping
unintended rapid release of entire drug dose form ER system
why does dose-dumping occur
due to:
coating failure
alcohol interaction
mechanical damage (chewing or crushing)
manufacturing defects
why is dose-dumping dangerous
increased risk of:
toxicity
side effects
overdose
why are ER systems more expensive
Specialized polymers
Complex manufacturing
More stringent quality control
Stability testing requirements
difference between single unit and multi-unit systems
single unit - tablets and capsules
dose of drug within single unit
multi-unit - pellets, mini-tablets and granules
dose of drug distributed among several units
advantages of multi-unit systems
drug is distributed along various units smaller in size
spread easily throughout GIT
more expensive to make than single unit
what are the 3 main mechanisms of extending drug release
dissolution controlled release
diffusion controlled release
osmosis
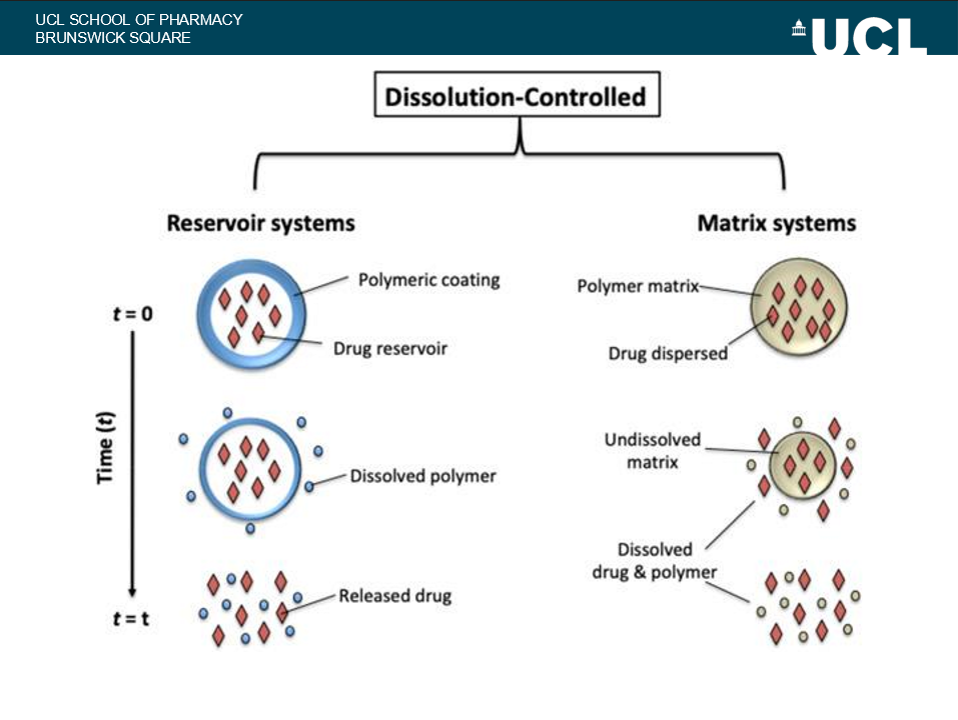
describe the dissolution controlled release mechanism
polymeric coating takes time to dissolve
this means drug also takes time to come out
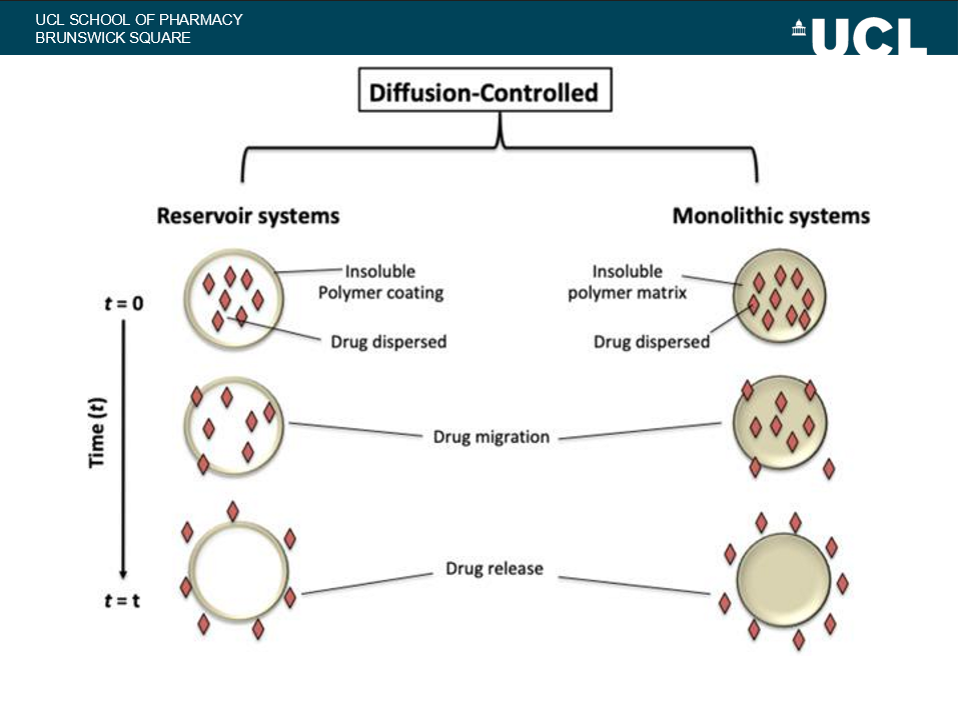
describe diffusion controlled mechanism
coating does not dissolve
GI fluid goes into system
drug is dissolved
drug moves out of system and is released
examples of coatings or reservoirs
difference between dissolution and diffusion systems
Dissolution systems = coatings will dissolve
dissolution system takes a long time to dissolve so takes a while for drug to come out
Vs
Diffusion systems = coating does not dissolve
Diffusion system remains intact but it’s a physical barrier through which the drug has to diffuse which takes a long time
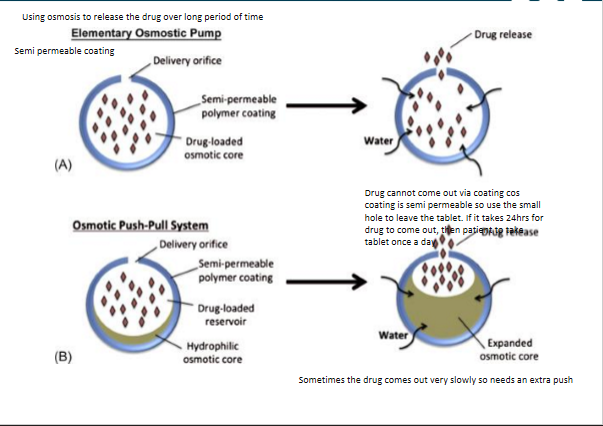
how does the osmotic system release drug
semi permeable polymer coating
fluid can enter
drug cannot leave
GI fluid enters system through semi permeable coating
fluid dissolves drug and osmotic agent
KCl builds up osmotic pressure
to reduce pressure, drug is released out of tablet over long time through the osmotic delivery orifice (hole in coating)
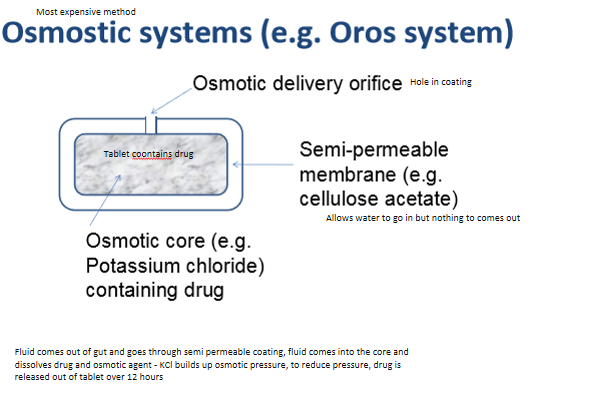
summary of osmotic system