Cardiology
1/59
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
60 Terms
Criteria for a STEMI?
Symptoms consistent with ACS (generally >20mins) with persistent (>20 mins) ECG features in 2 or more contiguous leads of:
2.5mm ST elevation leads V2-3 men under 40 or 2mm ST elevation leads V2-3 men over 40
1.5mm ST elevation V2-3 in women
1mm ST elevation in other leads
New LBBB
Initial treatment of STEMI? Duration of anticoagulation?
Aspirin 300mg
PCI within 120 mins if presented within 12 hours of symptom onset or if after 12 hours but still ongoing evidence of ischaemia
Going for PCI and not already anticoagulated = prasugrel
Going for PCI and already anticoagulated = clopidogrel
No PCI = ticagrelor (clopidogrel if high bleeding risk)
Aspirin lifelong, 2nd agent for 12 months
Anticoagulation during PCI?
Radial access – Unfractionated heparin with bailout glycoprotein IIb/IIIa inhibitor
Femoral access – bivalirudin with bailout GPI
STEMI presented within 12 hours but no access to PCI within 120 mins - what treatment would be given? What needs to be given with this?
Fibrinolysis - if ST elevation not fixed 60-90 mins later, consider PCI
Give fondaparinux
Complications of MI? Signs of LV free wall rupture? Following MI, acute heart failure and pansystolic murmur? Following MI, persistent ST elevation with fatigue. Signs of papillary muscle rupture? Which MI can cause AV block?
DREAD - Death, Rupture of papillary muscles, heart failure, Arrhythmia, Aneurysm, Dressler’s syndrome
Anterior MI. 10 days later - low BP, raised JVP, muffled heart sounds, crackles, low O2
VSD
LV aneurysm
Dyspnoea, orthopnoea, hypotension, raised JVP, new pansystolic murmur
Inferior MI
Management of NSTEMI/unstable angina? Timelines for coronary angiography? What would you give if having PCI?
Aspirin 300mg
Fondaparinux if no immediate coronary angiography
If immediate coronary angiography or creatinine >265 - give unfractionated heparin
Coronary angiography (with follow-on PCI if necessary):
Immediate – clinically unstable
Within 72hrs if GRACE >3%
Consider if experience ischaemia subsequently after admission
If having PCI – give unfractionated heparin (regardless of fondaparinux)
Prior to PCI - further antiplatelet prasugrel or ticagrelor (clopidogrel if taking oral anticoagulant)
No PCI – ticagrelor or clopidogrel if high bleeding risk
ACS secondary prevention?
ACE inhibitor
Beta blocker
Statin - primary prevention 20mg, secondary prevention 80mg
Aspirin 75mg
STEMI/NSTEMI - anticoagulated for 12 months
ACE inhibitor - U&Es checked in 1-2 weeks, what rise is acceptable?
Rise in creatinine up to 30% from baseline acceptable
Rise in potassium up to 5.5 acceptable
Management of angina? How to reduce nitrate tolerance?
Aspirin and statin
Sublingual GTN
1st line - BB or CCB (verapamil or diltiazem)
If combo, then amlodipine, nifedipine
Poor response to initial treatment – increase to max dose before adding other stuff
On monotherapy and symptomatic and can’t tolerate the other = long-acting nitrate, ivabradine, nicorandil, ranolazine
BB and CCB – only add 3rd drug if awaiting PCI/CABG assessment
If taking standard release isosorbide mononitrate – asymmetric dosing interval to maintain 10-14 hours nitrate-free time – reduce chances of tolerance
What is persistent AF? When would you rhythm control first?
Persistent AF = greater than 7 days
Rate control unless coexistent heart failure, first onset AF (less than 48 hours), obvious reversible cause
How do you rate control in AF?
1st line - BB or diltiazem
If still uncontrolled, any 2 of:
Beta blocker, diltiazem, digoxin
AF - how do you rhythm control in less than 48 hours onset?
Give heparin
Electrical - DC cardioversion or
Pharmacological - flecainide or amiodarone if structural heart disease
No need for further anticoag
AF - how do you rhythm control in more than 48 hours onset?
Anticoagulate for at least 3 weeks first (or do TOE – if no left atrial appendage thrombus can give heparin and cardiovert immediately)
Electrical instead of pharmacological
High risk of cardioversion failure – 4 weeks amiodarone or sotalol first
Anticoagulated for 4 weeks following cardioversion. After this, consider individual risk.
Components of CHA2DS2-VASc? When would you anticoagulate? How would you assess bleeding risk?
Congestive heart failure - 1
HTN - 1
Age >75 - 2
Age 65-74 - 1
Diabetes - 1
Stroke/TIA - 2
Vascular disease - 1
Sex female - 1
0 = no treatment
1 = consider anticoagulation only in males
2 or more = consider anticoagulation
Assess bleeding risk with ORBIT
AF and which condition is an absolute indication for anticoagulation?
AF + valvular disease
Choices of anticoagulation after TIA/stroke? When would you start it?
Warfarin or direct thrombin inhibitor (dabigatran) or factor Xa inhibitor (apixaban, rivaroxaban)
After TIA - anticoagulated ASAP after excluding haemorrhage
After stroke – anticoagulated after 2 weeks (antiplatelet in meantime)
Heart failure - when would you refer for specialist assessment?
NT-proBNP – high = specialist assessment +TTE within 2 weeks.
Raised = specialist assessment +TTE within 6 weeks
Management of heart failure - 1st, 2nd, 3rd line?
1st line – ace inhibitor AND beta blocker – start one at a time (no effect on mortality in HF with pEF)
2nd line – aldosterone antagonist, SGLT2- inhibitor
3rd line – ivabradine (heart rate has to be 75), sacubitril-valsartan (for those symptomatic on ACEi/ARBs – start after washout period), hydralazine + nitrate, digoxin (strongly indicated if also have AF)
Heart failure vaccines? When would you give ICD?
Annual influenza and one-off pneumococcal (booster 5 years if asplenic, CKD)
Cardiac resynchronisation therapy – for those with HF (LVEF<35%) and wide QRS (>120) and persistent symptoms despite medical therapy - ICD
Pericarditis causes? ECG changes? Cause of elevated troponin? Management?
Causes – viral (coxsackie), TB, post-MI (early – fibrinous, late – autoimmune/Dressler’s), connective tissue disease, malignancy
PR depression, saddle-shaped ST elevation
Need to have TTE
May have elevated trop – myopericarditis
Athletes should avoid strenuous exercise for a least 3 months until symptoms resolved and investigations have normalised
Acute idiopathic or viral – NSAIDs and colchicine
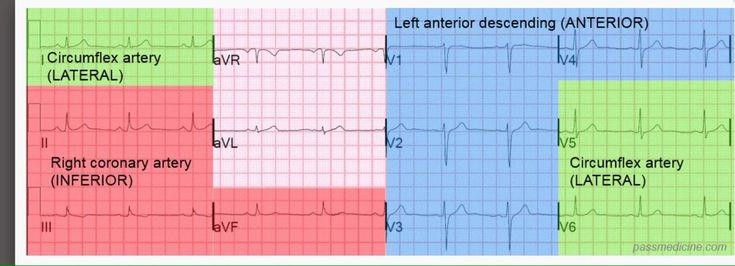
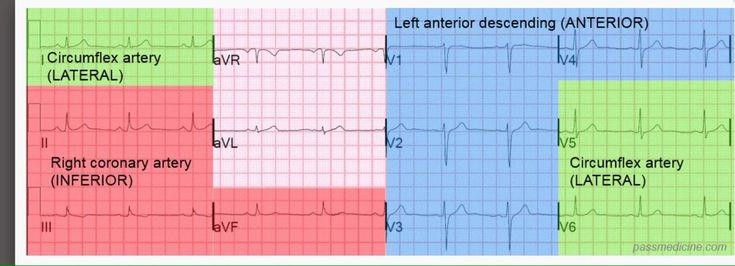
ECG territories?
ECG changes in 1) STEMI, 2) NSTEMI, 3) posterior MI, 4) pericarditis, 5) Dressler’s syndrome?
1) STEMI - ST elevation, Q waves
2) NSTEMI - ST depression, T wave inversion
3) Posterior MI - V1-3 horizontal ST depression, tall broad R waves, upright T waves, dominant R wave V2
4) Pericarditis - saddle-shaped widespread ST elevation, PR depression
5) Dressler’s syndrome - ST elevation and PR depression with reciprocal ST depression and PR elevation in aVR
ECG changes in 1) AF, 2) atrial flutter, 3) 1st degree block, 4) 2nd degree Mobitz I block (Wenkebach), 5) 2nd degree Mobitz II block, 6) 3rd degree block?
AF – irregularly irregular, absent P waves
Atrial flutter - >300bpm, regular, sawtooth waves
1st degree block – PR interval prolonged
2nd degree Mobitz I block (Wenkebach) – PR gets longer until QRS dropped
2nd degree Mobitz II block – steady PR but blocked QRS
3rd degree block– complete block
ECG changes in 1) LBBB, 2) RBBB, 3) pulmonary HTN, 4) normal axis deviation, 5) L axis deviation, 6) R axis deviation?
LBBB – WiLLiaM – deep S V1, broad R V6
RBBB – MaRRoW
Pulmonary HTN – Peaked P waves, R axis deviation, RVH, RBBB
Normal axis deviation – I positive, II most positive, III tiny bit positive
Left axis deviation – lead III negative (only significant if lead II negative)
Right axis deviation – lead I negative and lead III positive
ECG changes in 1) digoxin, 2) hypokalaemia, 3) hypothermia, 4) hypercalcaemia?
Digoxin – down-sloping ST depression
Hypokalaemia – U waves, small/absent T waves, ST depression, long QT, long PR
Hypothermia – J wave – small hump at end of QRS, bradycardia
Hypercalcaemia – short QT
ECG normal variants in athlete?
Sinus brady, junctional rhythm, 1st degree heart block, Mobitz I (wenkebach)
Aortic stenosis causes? Murmur/heart sounds? Signs?
Causes – degenerative calcification, BAV, William’s syndrome, post-rheumatic disease, HOCM
Ejection-systolic crescendo-decrescendo
Narrow pulse pressure
Soft/absent S2
S4 gallop due to LVH
Pulsus tardus – slow rising carotid
Pulsus parvus – decreased pulse amplitude
Aortic regurgitation causes? Murmur/heart sounds? Signs?
Causes – rheumatic fever, connective tissue disease, BAV, IE, aortic dissection
Early diastolic decrescendo
Wide pulse pressure
Collapsing water hammer pulse
Quincke’s sign – pulsation in nail beds
de Musset’s sign – head nodding with each beat
Pistol shot femoral – sharp bang on auscultation
Mitral stenosis causes? Murmur/heart sounds? Signs?
Causes – Mainly rheumatic fever
Can get haemoptysis
Late diastolic decrescendo crescendo
Loud S1
“a” wave in jugular venous pulsations – pulmonary HTN and RVH
Mitral regurgitation causes? Murmur/heart sounds? Signs?
Causes – post-MI, mitral valve prolapse, IE, rheumatic fever
Pansystolic
Soft S1, prominent S3 in CCF
Tricuspid regurg murmur? Pulmonary stenosis murmur? ASD murmur? PDA murmur?
TR - pansystolic, split S2
PS - ejection-systolic, widely split S2
ASD - fixed split S2
PDA - machinery murmur, bounding pulse
LBBB murmur? RBBB murmur? HCM murmur? RCM murmur?
LBBB - reverse split S2
RBBB - widely split S2
HCM - ejection systolic murmur LLSE, thrill at LLSE, S4
RCM - increased JVP, S3, S4
S1? S2? S3? S4?
S1 – closure of mitral and tricuspid. Soft in MR, loud in MS.
S2 – closure of aortic and pulmonary. Soft in AS.
S3 – normal in under 30. Heard in LVF, constrictive pericarditis, MR.
S4 – AS, HOCM, HTN.
Examples of narrow-complex tachys? WPW ECG changes? Type A vs type B? Management?
Sinus tachy
AF
Atrial flutter
SVT (p waves hidden) - AVNRT, AVRT, atrial tachycardia
AVRT - WPW - type A is L sided pathway (dominant R wave V1) and type B R sided pathway (no dominant R wave V1)
ECG WPW - short PR, wide QRS, delta wave
Management - sotalol (not in AF), amiodarone, flecainide
Definite - radiofrequency ablation
Management of narrow complex tachys? Half life of adenosine?
Shocked = synchronised DC cardioversion
Not shocked = Vagal manoeuvres → adenosine 6mg → adenosine 12mg → adenosine 18mg → verapamil/BB → DC cardioversion (avoid adenosine in asthmatics)
Adenosine half-life 8-10 seconds
Definitive treatment = radiofrequency ablation
Management of broad complex tachys?
Adverse effects = DC cardioversion
No adverse effects = amiodarone
Adult ALS? Half life of amiodarone?
Shockable = VF / pulseless VT
Non-shockable = asystole / PEA
Compressions to ventilation is 30:2
Defib = 1 shock then 2 mins CPR / monitored patients is 3 shocks
Drug delivery = IV to IO
Non-shockable
- Adrenaline 1mg ASAP
- Repeat every 3-5 minutes
Shockable
- After 3 shocks, 300mg amiodarone (half-life 20-100 days)
- 1 min after CPR restarted after shock 3 = adrenaline
- Further 150mg amiodarone after 5 shocks
- Alternative to amiodarone – lidocaine
PE suspected – thrombolytic drugs and continue CPR for extended period of 60-90mins
Management of bradycardia?
Atropine 500mcg IV – up to max 3mg → transcutaneous pacing → isoprenaline/adrenaline infusion → transvenous pacing
Cardiac tamponade triad? Signs?
Beck’s triad = raised JVP, low BP, muffled heart sounds
Kussmaul’s sign = raised JVP and neck vein distention on inspiration
Pulsus paradoxus = exaggeration in variation in pulse pressure in inspiration, causing drop in systolic BP
Infective endocarditis - valve most commonly affected? Most common causative organisms? Treatment?
In normal valves, mitral valve most commonly affected
S. aureus = IVDU, diabetes, surgery – tricuspid valve
S. epidermidis if <2months post-valve surgery
S. viridans = dental
Strep bovis = colorectal cancer
Abx – 4 weeks native valve, 6 weeks prosthetic valve
MRSA – IV vanc and rifampicin or IV vanc and rifampicin and gentamicin if prosthetic heart valve
Aortic dissection - classifications? Investigations and findings? Management? Complications of backward and forward tear?
Tear in tunica intima
Stanford classification:
Type A - ascending aorta - control BP (IV labetalol) + surgery
Type B - descending aorta - control BP (IV labetalol)
DeBakey classification:
Type I – originates in ascending can go distal, type II – originates and confined to ascending, type III – originates in descending, extends distal
Investigations:
CXR – widened mediastinum
CT angiography CAP – false lumen key finding
TOE if too unstable for CT
Complications backward tear – inferior MI, aortic incompetence/regurg
Complications forward tear – unequal arm pulses/BP, stroke, renal failure
Hypertrophic Obstructive Cardiomyopathy - inheritance pattern? ECHO findings? Management? What med would you avoid?
Leading cause sudden cardiac death young athletes
Autosomal dominant. Mutation in gene encoding Beta-myosin heavy chain protein
Echo findings – MR SAM ASH – mitral regurg, systolic anterior motion of anterior mitral valve leaflet, asymmetric hypertrophy
ABCDE – amiodarone, BBs/verapamil. Cardioverter defib, dual chamber pacemaker, endocarditis prophylaxis
Avoid ACEi
Arrhythmogenic right ventricular cardiomyopathy - inheritance pattern, ECG finding, management? What is Naxos disease?
2nd most common cause of sudden cardiac death in young after HCM
Autosomal dominant
Epsilon wave in 50% - terminal notch in QRS
Sotalol, catheter ablation to prevent VT, implantable cardioverter-defib
Naxos disease – autosomal recessive variant – ARVC, palmoplantar keratosis, woolly hair
What is dilated cardiomyopathy? What is restrictive cardiomyopathy? Acquired cardiomyopathies?
Dilated cardiomyopathy
Most common form of cardiomyopathy
Alcohol, coxsackie B
S3, systolic murmur, ‘balloon’ appearance of heart on CXR
Restrictive cardiomyopathy
Amyloidosis, post-radiotherapy
Acquired cardiomyopathies
Peripartum
Takotsubo - stress-induced
Warfarin and high INR management? INR targets?
INR 5-8, no bleeding – omit 1-2 doses, reduce subsequent dose
INR 5-8, minor bleeding – stop warfarin, IV vit K 1-3mg. Restart when <5
INR >8, no bleeding – stop warfarin, 1-5mg vit K oral. Rpt if high after 24hrs. Restart when <5.
INR >8, minor bleeding – stop warfarin, give IV vit K 1-3mg. Rpt if high after 24hrs. Restart when <5.
Major bleeding – stop warfarin, IV vit K 5mg and prothrombin complex concentrate – if not available then FFP.
INR targets:
Mechanical aortic valve – 3
Mechanical mitral valve – 3.5
VTE – 2.5 / Recurrent VTE – 3.5
AF – 2.5
Rheumatic fever organism? Criteria? Signs? Treatment?
S. pyogenes
Jones criteria
Erythema marginatum, polyarthritis, carditis (endo mainly), subcutaneous nodules
Treatment – pen V, NSAIDs, aspirin
What is non-pulsatile JVP a sign of? What is Kussmaul’s sign and when is it seen?
Non-pulsatile – SVC obstruction
Paradoxical rise in JVP during inspiration – Kussmaul’s sign – constrictive pericarditis
HTN in afro-Caribbean with T2DM - 1st line?
A2RB
Management of acquired QT?
IV isoprenaline (CI in congenital)
What is a capture beat?
Normal QRS complex in between VT complexes
Hypokalaemia precipitates ____ toxicity? Symptom?
Digoxin toxicity
Green/yellow tinge to vision
Brugada syndrome - inheritance pattern, ECG changes? Investigation?
Sudden cardiac death, autosomal dominant
Convex ST elevation in V1-3 followed by negative T wave, partial RBBB
ECG changes more apparent after giving flecainide or ajmaline – Ix of choice
Avoid drugs that can precipitate arrhythmias, implantable device
Buerger’s disease - what is it? Signs?
Small and medium vessel vasculitis, strongly associated with smoking
Extremity ischaemia, superficial thrombophlebitis, Raynaud’s
Takayasu’s arteritis - what is it? Signs/symptoms? Investigation? Management?
Large vessel vasculitis – occlusion of aorta
Systemic features vasculitis, unequal BP upper limbs, carotid bruit, absent/weak peripheral pulses, limb claudication on exertion, AR
MRA or CTA
Management – steroids
Management of Torsades de Pointes? What can cause this?
IV magnesium sulphate
Macrolides
Driving advice for 1) elective angioplasty, 2) CABG, 3) ACS, 4) angina, 5) Pacemaker insertion, 6) ICD for sustained arrhythmia, 7) ICD prophylactically, 8) AAA 6.5cm, 9) heart transplant?
Elective angioplasty – 1 week off
CABG – 4 weeks off
ACS – 4 weeks off (1 weeks if successfully treated by angioplasty)
Angina – no driving if symptoms occur at rest/wheel
Pacemaker insertion – 1 week off
ICD for sustained arrhythmia – off for 6 months
ICD prophylactically – off for 1 month
AAA of 6.5cm – no driving
Heart transplant – off for 6 weeks
Which electrolyte abnormalities can cause long QT syndrome? Which med would you avoid in long QT?
Hypokalaemia, hypocalcaemia, hypomagnesemia
Avoid macrolides
Adrenaline dose for cardiac arrest vs anaphylaxis?
Cardiac arrest = 1mg – 10ml 1:10,000 or 1ml 1:1,000
Anaphylaxis = 0.5mg – 0.5ml 1:1,000
What med is CI in people with renovascular disease?
ACE inhibitors
Difference in diastolic murmur in AR vs MS?
AR = early diastolic murmur
MS = Mid-diastolic murmur