excretion final
1/74
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
75 Terms
What is excretion?
The removal of metabolic waste from the body that may build up and become toxic
What are the main excretory products?
CO2, urea, ammonia, bile pigments
Why do we get rid of metabolic waste products?
They can alter the pH interfering with cell processes so the normal metabolism is affected, they may also inhibit enzymes
Why is excess CO2 a problem?
It is mostly transported as hydrogen carbonate ions the formation of which releases H ions that affect the pH of the cytoplasm of RBC's changing the bonds and shape of haemoglobin reducing its affinity for oxygen
Why must we excrete nitrogenous compounds?
Amino acids can't be stored because they contain a toxic amino group that needs removing absorbed by cells and decreases their water potential and they burst. uric acid may crystallise in joints
Through which vessels does blood flow into the liver?
The hepatic artery (oxygenated blood from the heart) and the hepatic portal vein (deoxygenated blood from the digestive system)
What is the bile duct?
Duct that carries the bile secreted in the liver from the liver to the gall bladder
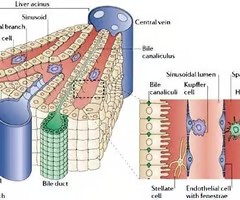
liver diagram
How is the liver further divided from lobes?
Lobes are divided into lobules
In what vessel does blood from the vein and arteries mix?
A sinusoid
What is the purpose of blood passing through sinusoids?
They put the blood in close contact with liver cells that alter the concentrations of substances in it
What do kupfer cells in sinusoids do ?
They recycle and break down RBC's producing bilirubin as well
What vessel drains blood from the liver?
The hepatic vein
What are the metabolic functions of hepatocytes?
Protein synthesis, transformation and storage of carbohydrates, synthesis of cholesterol and detoxification
How do hepatocytes store glycogen ?
In granules in the cytoplasm
How might hepatocytes detoxify substances?
They may oxidise, reduce or combine them with another molecule
How is alcohol broken down by detoxification?
Ethanol is broken down by ethanol dehydrogenase to ethanal which is dehydrogenated by ethanal dehydrogenase to ethanoate which combines with coenzyme A to form acetyl coenzyme A. NAD forms reduced NAD from hydrogen ions
Why does alcohol make fat build up?
Because NAD is used to detoxify it and if it is used up doing this it cannot break down fatty acids
Which part of amino acids makes them toxic ?
The amino group
What is deamination ?
amine group and hydrogen is removed from amino acid to form ammonia and a keto acid which may be respired or converted to glucose or fat.
What is the ornithine cycle?
ammonia is toxic so is converted to urea. ammonia and co2 combined to urea and water
urea diffuses through the phospholipid bilayer of the hepatocytes and into the kidney
What is the role of the kidney?
To remove waste products from the blood and produce urine
Where is each bowmans capsule ?
In the cortex
Which vessel enters the kidney ?
Renal Artery
What is the glomerulus ?
A bunch of capillaries that are the result of the renal artery splitting into afferent arterioles
what is ultrafiltration?
when fluid from the blood is pushed into the Bowmans capsule
which three layers act as the filter for ultrafiltration?
The endothelium of the capillary, the basement membrane and the epithelial cells of the Bowmans capsule (podocytes)
what substances are filtered out of the glomerulus?
water, amino acids, glucose, urea and mineral ions
what substances are not filtered out of the glomerulus and why?
blood cells and proteins because they are too large
What is the basement membrane composed of?
- meshwork of collagen and glycoprotein fibers
- water and small molecules can pass through
- proteins are too large and are repelled by negative charges on fibers

outline the Endothelium of blood capillary in the bowman's capsule
- very thin
- perforated with thousands of pores of about 10 nm diameter (occupy ~30% of capillary wall)
- provides a barrier to cells but not plasma proteins
outline the Epithelium of renal capsule in the bowman's capsule
- made of cells which are modified for filtration (podocytes)
Describe podocytes
- each cell has many foot-like extensions projecting from its surface
- the extensions wrap around the capillaries of the glomerulus and interlink with extensions from neighboring cells
- these extensions fit together loosely leaving filtration slits about 25 nm wide
- the filtered fluid passes through the filtration slits

why is it important that these substances are/are not filtered out ?
So the blood is left with a low water potential that makes reabsorption of water back into the blood possible later
what happens in the PCT?
reabsorption; of most sugars, mineral ions and some water
how is a salt gradient established in the loop of Henle
The descending limb is permeable to water but not salts but the ascending limb is permeable to salts but not water. This means that as the loop descends into the medulla, the interstitial fluid becomes more salty and hypertonic as water leaves the tubule by osmosis
outline the countercurrent mechanism in the vasa recta as a way of establishing a salt gradient
the vasa recta blood network surrounds the loop of Henle flows in the opposite direction (counter-current). This means that salts released from the ascending limb are drawn down into the medulla, further establishing a salt gradient
what happens in the thin Ascending Loop of Henle
As the fluid in the tubule ascends back up towards the cortex, the water potential becomes higher (less negative) but cant leave as the wall of the ascending limb is impermeable to water. Due to counter current from vasa recta, salts are drawn down into the medulla, firmly establishing a salt gradient.
what happens in the thick ascending loop of Henle
-contains large epithelial cells w specialized transport
proteins
1) The Na+/K+-ATPase pump in the membrane pumps 3Na+ out of, and 2K+ into, the cell
2) low intracellular Na+ conc drives the electroneutral Na-K-2Cl co-transporter (NKCC2) at the apical membrane.
3) K+ is recycled back into the lumen through K+
channels in the apical membrane = continued NaCl uptake. Cl- leaves through chloride channels in the basolateral membrane. The inward movement of K+ and Cl- occurs against their electrochemical gradients and is powered by the inward movement of Na into the cell.
what happens in the distal convoluted tubule
active transport finely tunes the concentration of various salts in the tubule
what happens in the collecting duct
When the fluid reaches the collecting duct it has a high water potential (less negative). The collecting duct carries fluid back into the medulla, which contains a lot of salts (low/very negative water potential). Therefore, as the fluid passes through, water moves by osmosis, from the tubule fluid into the surrounding tissue. It then enters the blood capillaries by osmosis and is carried away.
how is osmoregulation activated/ detected
Osmoreceptors in hypothalamus monitor the water potential of the blood. If the osmoreceptors detect a decrease in the water potential of the blood…… ADH causes the kidneys to reabsorb more water, which reduces the loss of water in the urine
whats the effect of ADH (Are DeHydrated) on the kidneys
ADH causes the luminal membranes (i.e. those facing the lumen of the nephron) of the collecting duct cells to become more permeable to water by causing an increase in the number of aquaporins (water
how does ADH work
ADH molecules bind to receptors what activates a signaling cascade = phosphorylation of the aquaporin molecules. Phosphorylated aquaporins, drive fusion of vesicles with the luminal membranes of the collecting duct cells. Water molecules move from the collecting duct (high water potential), through the aquaporins, and into the tissue fluid and blood plasma in the medulla (low water potential)
what is the counter current multiplier mechanism
It is divided into three segments: the descending, thin ascending and thick ascending loop of Henle. the countercurrent multiplier system increases the concentration of solute and ions within the interstitium of the medulla. This allows the nephron to reabsorb more water in the same time frame using as little energy as possible.
summarize osmoregulation
- The loop of Henle establishes a salt gradient (hypertonicity) in the medulla.
- Anti-diuretic hormone (ADH) regulate the level of water reabsorption in the collecting duct
describe the mechanism of reabsorbtion in the PCT
Sodium ions are pumped out of the cells lining the tubule, creating a concentration gradient of sodium ions towards the cell cytoplasm. Sodium ions therefor diffuse into the cell via cotransport proteins carrying glucose or an amino acid with them. The glucose and amino acids diffuse into the blood on the other side of the PCT. A water potential gradient is created in the process so that water moves into the cell by osmosis.
Describe the changes in glucose concentration throughout the tubule
in the PCT glucose is selectively reabsorbed so the concentration of it present is removed.
Describe the changes in Na+ and K+ ions concentration throughout the tubule
Na+ ions diffuse into the descending limb of the loop of Henle (concentration rises) in the d. limb they are pumped out (concentration drops). K+ ions are actively transported into the tubule (concentration increase) and when water is removed from the tubule their concentration also increases.
Describe the changes in urea concentration throughout the tubule
as water is withdrawn from the tubule the concentration rises. It is also actively moved into the tubule
what is osmoregulation?
controlling the water potential throughout the body
how do kidneys alter the volume of urine produced?
they alter the permeability of the collecting duct
What is filtered out of the blood into the nephron during Ultrafiltration?
Water
Amino acids
Glucose
Urea
Inorganic ions (sodium, chloride, potassium)
what are the stages of selective reabsorption
1) Sodium-potassium pumps pump Na out of the cells lining the PCT, into the blood. This requires ATP and a conc gradient is created
2) This drives the entry of Na through a co-transporter protein (symport) -this carries glucose or an amino acid at the same time, against their concentration gradient.
3) this reduces the water potential inside the cells lining the PCT, water also moves in to the cells by Osmosis.
4) the concentration of glucose + amino acids has increased inside the cells lining the PCT, they diffuse down their concentration gradient out into the blood
5) This in turn causes the water potential of the blood to be lower than the cells, causing water to follow by osmosis.
what are the role of the kidney
- As an osmoregulatory organ - they regulate the water content of the blood (vital for maintaining blood pressure)
- As an excretory organ - they excrete the toxic waste products of metabolism (such as urea) and substances in excess of requirements (such as salts)
kidney diagram
Each kidney is supplied with oxygenated blood through a renal artery (branches off from Aorta). A renal vein returns deoxygenated blood to the vena cava. It is made up of an outer cortex and an inner paler medulla. A whitish area called the pelvis lies in the centre of one edge. This leads to the ureter.
what is the nephron
- functional unit of the kidney - the nephrons are responsible for the formation of urine and the balance of ions

what is the ornithine cycle
Ammonia is very soluble and very toxic so it cannot remain in the body.
in the Liver, carbon dioxide + ammonia = citruline
plus more ammonia = arginine
When urea is removed, arginine is reconverted into ornithine to start the process again
what nitrogenous waste products are left other than urea and how are they broken down
Uric acid (made from excess purine bases)
Creatine (synthesised from creatine phosphate)
how are the walls of the PCT is specialized for Selective Reabsorption
- Microvilli = a large surface area
- Co-transporter proteins in the membrane
transport glucose and amino acids with
sodium ions (by facilitated diffusion)
- The opposite membrane (close to blood
capillaries) is folded to increase surface
area. It contains sodium-potassium
pumps that pump sodium out and
potassium in.
- Cell cytoplasm has many mitochondria
indicating that energy is required as ATP
when less water is needed…..
the walls are less permeable so less water is reabsorbed and more urine is produced
when more water is needed…..
the walls are more permeable so more water is reabsorbed and less urine is produced
how is the permeability of the walls of the collecting duct altered?
the walls have receptors to ADH and when it binds to them a series of enzyme controlled reactions result in vesicles containing aquaporins fusing with the membrane that act as water channels
what is the result of an increased level of ADH?
the walls are made more permeable and less urine is produced
what is the result of a decreased level of ADH?
the walls are made less permeable and more urine is produced
where in the body is water potential detected?
osmoreceptors in the hypothalmus
How does the hypothalamus respond to low water potential?
Osmorecpetors shrink which stimulates neurosecretory cells in the hypothalmus. These cells produce ADH which moves down the axon to the terminal bulb in the posterior pituatory gland. ADH enters capillaries and is transported in the blood to collecting ducts
what is the glomerula filtration rate?
rate at which the fluid enters the nephrons
Detoxification of alcohol
1) Alcohol Dehydrogenase is used to convert ethanol to acetaldehyde (ethanal) and creates NADH.
2) Acetaldehyde dehydrogenase converts acetaldehyde(ethanal) to acetic acid.
this produces a lot of app which means hepatocytes don't metabolise causing fatty live
kidney failure causes
-diabetes
-chronic, uncontrolled high blood pressure
-chronic glomerulonephritis
-rea, water, salts and various toxins are retained and not excreted
Less blood is filtered by the glomerulus, causing the glomerular filtration rate (GFR) to decrease
This leads to a build-up of toxins in the blood
In addition, the electrolyte balance in the blood is disrupted (the concentrations of ions and charged compounds are not maintained)
kidney failure treatment
dialysis, kidney transplant
Types of dialysis
hemodialysis and peritoneal dialysis
disadvantage of dialysis
Both forms of dialysis impose heavy restrictions on the lives of patients that rely on them, as they have to make regular trips to the hospital to receive the treatment, which takes at least 3 hours each time. In addition, patients have to carefully control their diet to minimise their urea production and their salt intake
strength of a kidney transplant
The patient has much more freedom
less restrictive diet
The use of dialysis machines is very expensive and so this cost is removed
A kidney transplant is a long term solution whereas dialysis will only work for a limited time
disadvantage of kidney transplant
risk of rejection
patient must take immunosuppressants therefore susceptible to other infections
may only last 10years
not enough donors