cell recognition and the immune system
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
65 Terms
how does the immune system differentiate between self and non self cells
antigens present on all cell surfaces. Antigens could be proteins, glycoproteins or glycolipids. the combination on each cell surface is unique
name 4 types of foreign cells that can be identified using antibodies
pathogens
cells from other organisms of the name species eg organ transplants
toxins
abnormal body cells eg cancer cells
describe self vs non self antigens
Self-Antigens:
Present on normal body cells.
Recognised as harmless by the immune system.
Failure to recognise self-antigens correctly can result in autoimmune diseases (e.g., multiple sclerosis).
Non-Self Antigens:
Found on pathogens, transplanted cells, or abnormal cells (e.g., cancer cells).
Recognised as foreign, triggering an immune response.
They include bacterial surface proteins, viral coat proteins, and toxins.
define pathogen
microorganisms that cause communicable disease
define antigen
A molecule, usually a protein, that triggers an immune response.
through what process can pathogens change their surface antigens, and what does this cause
mutation- different antigens are formed due to changes in the genes of the pathogen, antigenic variability
what does the mutation of pathogen surface antigens mean? (ie what does this mean for immune responses, frequency of infection, precautions one may have to take to prevent infection)
Memory cells from a previous infection may no longer recognise the pathogen. - no secondary response. The primary response takes time to get rid of infection which is why you get ill again
Vaccines may need frequent updates, as seen with the flu vaccine. Also makes it difficult to develop new vaccines
Recurrent infections are common, e.g., the common cold and malaria.
what type of response do the antigens on the cell surface trigger
primary
when you are infected a second time by the same pathogen(same antigens on it’s surface) which response do they activate
secondary
describe how antigenic variation affects the production of vaccines to help protect people from catching influenza
the flu vaccine changes every year. This is because antigens on the surface change regularly due to mutations, forming new strains of the virus
memory cells produced from vaccination with one strain of the flu will not recognise other strains with different antigens . The strains are immunologically different
every year there are different strains of flu virus circulating in the population, so a different vaccine has to be made
new vaccines are developed and one is chosen eveyr year thats most effective towards the recent strain of circulating virus
Describe how the structure of an antigen enables it to be recognised by the immune system. (2 marks)
Antigens have a specific shape that is complementary to antibodies or T-cell receptors.
The immune system recognises non-self antigens as foreign, triggering an immune response.
describe the process of phagocytosis
the phagocye recognises the foreign/ non-self antigens on a pathogen. Chemicals released by the pathogen or damaged cells attract the phagocyte (chemotaxis)
this causes the pahgocyte to bind to the pathogen
the phagocyte engulfs the pathogen and is now contained in a phagocytic vacuole - ‘phagosome’
The lysosome, containing hydrolytic enzymes called lysozymes, fuses with the phagosome
the lysozymems released hydrolyse/digest and destroy the pathogen
the phagocyte then presents the pathogens antigens- it presents the antigens on it’s surface to activate other immune system cells
define phagocyte
Phagocyte: A white blood cell that engulfs and digests pathogens.
what cells do phagocytes activate
T-cells
what two defenses are enclosed in non-sepcific responses
physical and chemical defenses, phagocytosis
what two responses are enclosed in sepcific responses
cellular and humoral
name the two types of lymphocyte
T-lympocytes- migrate to the thymus gland for a period of maturation before migrating to the lymph nodes. Involved in the cellular response where they respond to antigens presented on body cells.
B-lymphocytes- B cells mature in the bone marrow. They are involved in the humoral response where they produce antibodies found in body fluids (or humors).
name the three types of T-cell/ lymphocyte
Helper T cells (TH cells)
These cells have receptors on their cell-surface that bind to complementary antigens on antigen-presenting cells. Release cytokines to activate other immune cells. - eg maturation of B cells and triggering production of antibodies. Also to activate phagocytes and cytotocxic T cells.
Cytotoxic T cells (TC cells)
These cells kill abnormal and foreign cells by producing a protein known as perforin. This protein makes holes in the cell-surface membrane, causing it to become freely permeable and causing cell death.
Memory T cells
These cells provide long-term immunity against specific pathogens. They provide a rapid response if the body is re-infected by the same pathogen.
describe the process of clonal selection in the cellular response, and what can the cloned T cells carry out
Phagocytes engulf pathogens and display their antigens on the cell-surface. They are now known as antigen-presenting cells.
Helper T cells with complementary receptors bind to these antigens.
On binding, the helper T cell is activated to divide by mitosis to form genetically identical clones.
The cloned T cells can carry out different functions:
Develop into memory cells - These circulate in the body to provide long-term immunity.
Stimulate phagocytosis - Cloned cells stimulate phagocytes to engulf pathogens.
Stimulate division of B cells - Cloned cells stimulate B cells to divide and produce antibodies.
Activate cytotoxic T cells - This allows TC cells to kill infected cells.
what cells do helper t cells activate
B cells, phagocytes, cytotoxic T cells
describe the cellular response
Stages Of The Cellular Response
Pathogen Invasion & Antigen Presentation
A phagocyte (e.g., macrophage) engulfs a pathogen and hydrolyses/ digests it.
It presents antigens from the pathogen on its surface, becoming an antigen-presenting cell (APC).
Activation of T-Lymphocytes
T-helper cells have different and specific T-cell receptors that bind to the antigen on the APC.
This activates the T-helper cell. We say the T-helper cell has undergone clonal selection.
Clonal Expansion & Differentiation
Activated T-helper cells divide by mitosis, this can be called clonal expansion.
They then differentiate forming:
More T-helper cells.
Memory T-cells which play a role in the secondary immune response for long-term immunity.
Cytotoxic T-cells (Killer T-cells) to directly kill infected cells.
Action of Cytotoxic T Cells (Killer T cells)
Cytotoxic T-cells release perforins, which create pores in the membrane of infected cells.
This causes cell lysis, killing the infected cell and preventing viral replication.
why is the cellular response important
targets viruses- which hide inside host cells- inaccessable to antibodies
essential for destroying cancer cells
long term immunity via memory T-cells
T-helper cells are needed to activate B-cells in the humoral response.
T-helper cells release cytokines (chemical signals) to stimulate further phagocytosis.
define the cellular response
The cellular (T-lymphocyte) response is part of the specific immune system.
The specific immune response is antigen-specific and provides long-term immunity.
T-lymphocytes respond to antigen presenting cells. These may be phagocytes, cancerous cells, transplanted cells or cells infected with a virus.
define humoral respnse
The humoral response involves B-cells and the production of antibodies by plasma cells.
It is part of the specific immune response, which is antigen-specific and provides long-term immunity.
Describe the role of T-lymphocytes in the immune response. (6 marks)
Phagocytes engulf pathogens and present antigens on their surface.
T-helper cells bind to the antigen on the antigen-presenting cell (APC) and become activated.
These activated T-helper cells divide by mitosis or undergo clonal expansion.
Some differentiate into cytotoxic T cells, which release perforins, creating pores in infected cell membranes and killing them.
Some differentiate into memory T cells, providing long-term immunity.
Some differentiate into T-helper cells which activate B-cells
How do cytotoxic T-cells kill infected cells?
Cytotoxic T-cells release perforins, which create pores in the infected cell’s membrane, causing lysis and cell death.
4 types of cells involved in the humoral response
Cells involved in the humoral response The humoral response involves the following types of cell: B cells
Plasma cells
Memory cells
Helper T cells
|
why is the humoral response calledthe humoral response - for unrelated memory only
The humoral response is so-called because it involves antibodies that are found in body fluids (or humors).
difference between clonal selection and expansion for B cells
Clonal selection - The B cell with the correct antibody is selected for cloning (by being activated by a T helper cell).
Clonal expansion - The division of specific B cells to produce genetically identical clones
describe the humoral response sequence
Stages of the Humoral Response
Activation of B-Cells (Clonal Selection)
B-cells have specific antibodies acting as receptors on their surface.
When a B-cell receptor binds to a complementary antigen, the B-cell engulf the antigen and presents it on its surface.
T-helper cells bind to the antigen-presenting B-cell and release cytokines, activating the B-cell.
Clonal Expansion (B-Cell Proliferation and Differentiation)
Activated B-cells undergo mitosis, producing many identical B-cells. This can also be called clonal expansion.
These differentiate into two types of cells:
Plasma Cells: Secrete large amounts of antibodies into the blood.
Memory B Cells: Provide long-term immunity by responding quickly if the same pathogen is encountered again.
Antibody Production and Action
Plasma cells secrete specific antibodies,- which bind to the pathogen’s antigen.
Antibodies act in the following ways:
Agglutination: Pathogens are clumped together, making it easier for phagocytes to engulf them.
Opsonisation: Antibodies coat the pathogen, marking it for destruction by phagocytes.
Neutralisation: Antibodies bind to and neutralise toxins. They also bind to viral proteins, stopping viruses from entering and infecting body cells.
Immunological Memory
Memory B-cells remain in the blood after infection.
If the same pathogen is encountered again, memory B-cells rapidly divide into plasma cells, producing antibodies much faster.
This is called the secondary immune response, which is faster and stronger than the primary response.

Exam Q- Describe how B-lymphocytes are activated and how they respond to a pathogen. (6 marks)
A B-cell with complementary receptors binds to the pathogen’s antigen.
The B-cell engulfs the pathogen and presents the antigen on its surface.
T-helper cells bind to the antigen-presenting B cell and release cytokines, activating the B cell (clonal selection).
The activated B-cell undergoes mitosis to form many identical B cells (clonal expansion).
These differentiate into plasma cells, which secrete antibodies
And memory B-cells, which provide long-term immunity.
define opsonisation, agglutination and neutralisation
Agglutination: Pathogens are clumped together, making it easier for phagocytes to engulf them.
Opsonisation: Antibodies coat the pathogen, marking it for destruction by phagocytes.
Neutralisation: Antibodies bind to and neutralise toxins. They also bind to viral proteins, stopping viruses from entering and infecting body cells
define antibody
Antibodies are specialized Y-shaped proteins produced by the immune system to identify and neutralize specific antigens, such as pathogens and toxins. They bind to antigens.
describe the structure of antibodies. Draw one. What type of protein, polyp chains, regions, bonds
Antibodies are globular proteins made up of four polypeptide chains: two heavy chains and two light chains.
They have variable regions forming two specific antigen-binding sites.
They have constant regions which consist of very similar amino acid sequences in all antibodies.
Disulfide bonds maintain the antibody’s stable quaternary structure by holding the 4 polypeptide chains together.
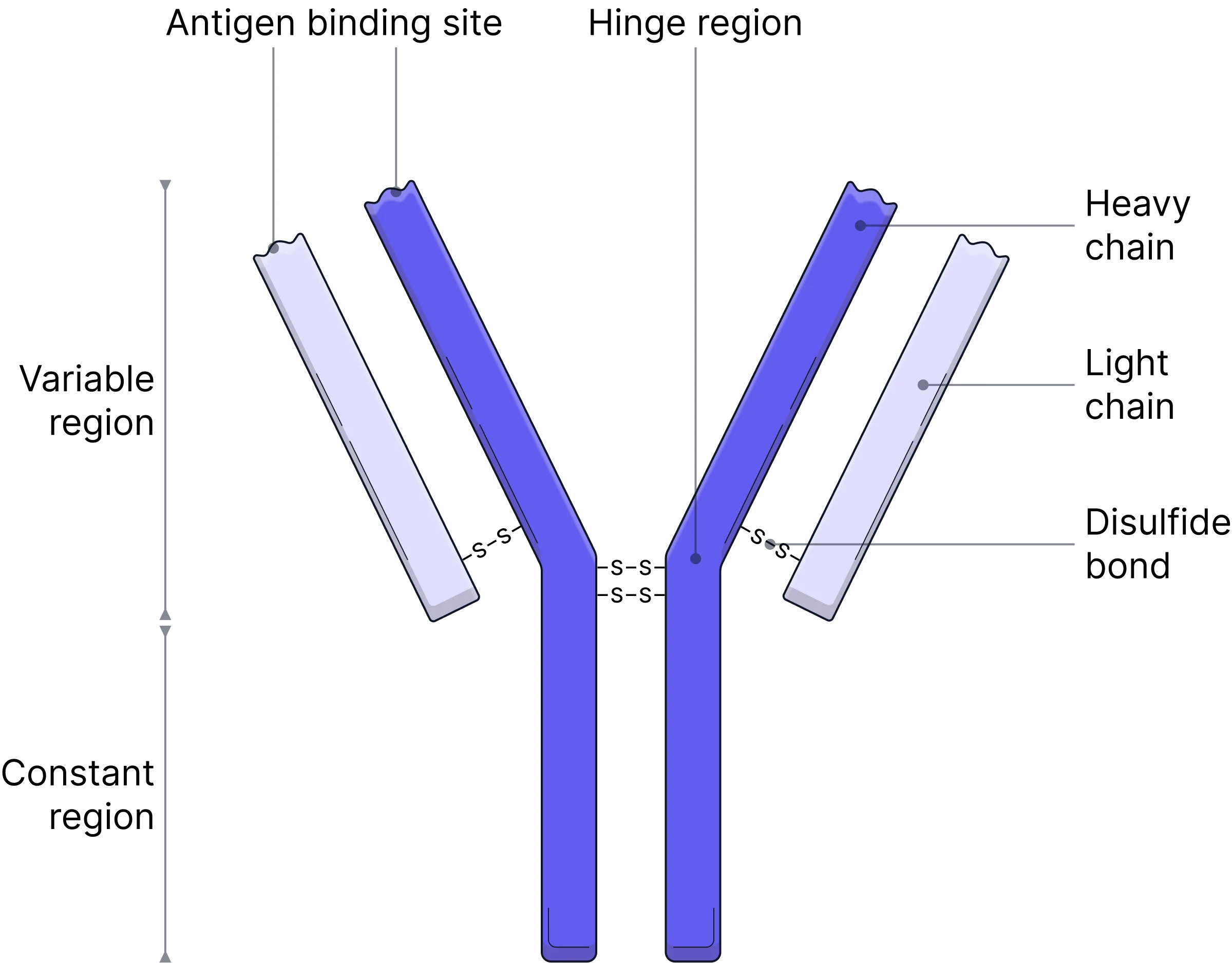
each antibody has a unique binding site - in the ‘-’ that fits onto a specific antigen. When an antibody binds it forms a what?
variable region.
antigen-antibody complex
how do antibodies contribute to pathogen destruction - 3 ways
Agglutination: Antibodies have two antigen binding sites (allowing them to bind to antigens on two different pathogens), clumping pathogens together to make them easier for phagocytes to engulf.
Neutralisation: Blocking toxins or preventing viruses from binding to host cells and replicating within them.
Opsonisation: Coating pathogens to mark them and enhance phagocytosis.
Describe the role of antibodies in agglutination and explain how this process helps the body fight infection. (3 marks)
Antibodies have two binding sites, allowing them to bind to antigens on two different pathogens.
This causes pathogens to clump together in a process called agglutination.
Agglutination makes it easier for phagocytes to engulf and destroy the pathogens by phagocytosis.
what are memory cells, T cells and B cells
T-cells are a type of white blood cell (lymphocyte) involved in the cellular response.
Types of T-cells include Helper T-cells, which activate B-cells, Cytotoxic T-cells (Killer T-cells), which kill infected or cancerous cells and Memory T-cells which provide long-term immunity.
B-cells are a type of white blood cell that is responsible for humoral immunity.
When activated, B-cells differentiate into plasma cells (which produce antibodies) and Memory B-cells (which provide long-term immunity).
Memory cells are long-lived immune cells that remain in the body after an infection has been cleared.
They allow for a faster and stronger secondary immune response if the same pathogen infects the body again.
Both Memory T-cells and Memory B-cells exist to provide long-term immunity.
what is the primary and secondary immune response
Occurs when the immune system encounters a pathogen for the first time.
Happens when the same pathogen, with the same antigen, infects the body again.
why is the primary response slow
The immune system must identify the antigen.
Specific B-cells must be activated and clone themselves (clonal selection and clonal expansion must take place). - there are few B cells that are specific to the pathogens antigens
Plasma cells produce antibodies, which take time to reach a high concentration.
describe the process of the primary and secondary response
Primary immune response:
|
Secondary immune response:
|
are the symptoms experienced in the secondary response? which cells are involved in each primary and secondary
no
primary- B cells (plasma)(antibodies) and T cells(respond to APC)
secondary- memory B + T cells(memory B differentiate to plasma, memory T activate cytotoxic T cells to destroy infected cells)
describe whythe secondary response is quicker
Memory B-cells quickly differentiate into plasma cells and produce antibodies.
Memory T-cells rapidly activate cytotoxic T-cells to destroy infected cells.
More antibodies are produced, and are produced more rapidly. They also remain in the bloodstream for longer.
Explain why the secondary immune response is faster and produces more antibodies than the primary response. (4 marks)
Memory B and T-cells remain in the body after the primary infection.
Upon re-exposure, memory B-cells differentiate rapidly into plasma cells.
Plasma cells produce antibodies more quickly and in higher concentrations.
The pathogen is destroyed before symptoms develop.
what is active and passive immunity and some differences
active- immunity developed after the immune response system makes it’s own antibodies. Artificial- antibodies made after a vaccination. Natural- eg zntibodies made after an infection
Takes a whule to become immune to the disease, but offers long term protection due to the produced memory cells
passive- immunity required by recieving antibodies from another organism. Natural- eg antibodies transmitted from mother to baby. Artificial- eg antibodies transfused or injecyed into individual immideate immunity to the disease, but it is short term protection because the antibodies are broken down and memory cells are not produced
describe how vaccinations lead to protection
Vaccines contain antigens from a pathogen, which stimulate the immune system to produce a primary immune response, this is an example of artificial, active immuntiy.
These antigens may be on a dead or weakened pathogen or may just be the isolated antigen.
Once injected with the antigen, an immune response is triggered.
B-lymphocytes produce plasma cells that secrete antibodies.- specific
Memory cells are produced, providing long-term immunity.
On secondary exposure, memory cells respond quickly and produce antibodies faster, preventing symptoms of disease.
how do vaccines prevent the spread of disease
When vaccinated individuals encounter the same pathogen, their immune system rapidly destroys it.
This reduces the chance of transmission of the pathogen to others.
Some pathogens require a large host population to survive, so reducing the number of susceptible individuals can eradicate diseases (e.g., smallpox).
describe herd immunity
When a large proportion of the population is vaccinated, non-vaccinated individuals are also protected.
The pathogen has fewer hosts, reducing its spread.
This is especially important for individuals who cannot be vaccinated, such as those with compromised immune systems.
Threshold for herd immunity varies between diseases (e.g., measles requires ~95% vaccination coverage).
contrast active and passive immunity (3 marks)
Active immunity occurs when the immune system produces its own antibodies after exposure to an antigen, while passive immunity involves receiving antibodies from an external source.
Active immunity forms memory cells, leading to long-term protection, whereas passive immunity does not produce memory cells and provides only short-term protection.
Active immunity takes time to develop, but passive immunity provides immediate protection.
what is a virus
non-living, acellular infectious particle that requires a host cell to replicate.
what is HIV
HIV (Human Immunodeficiency Virus) is a retrovirus that attacks the immune system, specifically T-helper cells.
Leads to AIDS (Acquired Immunodeficiency Syndrome), where the immune system is severely weakened, increasing susceptibility to infections.
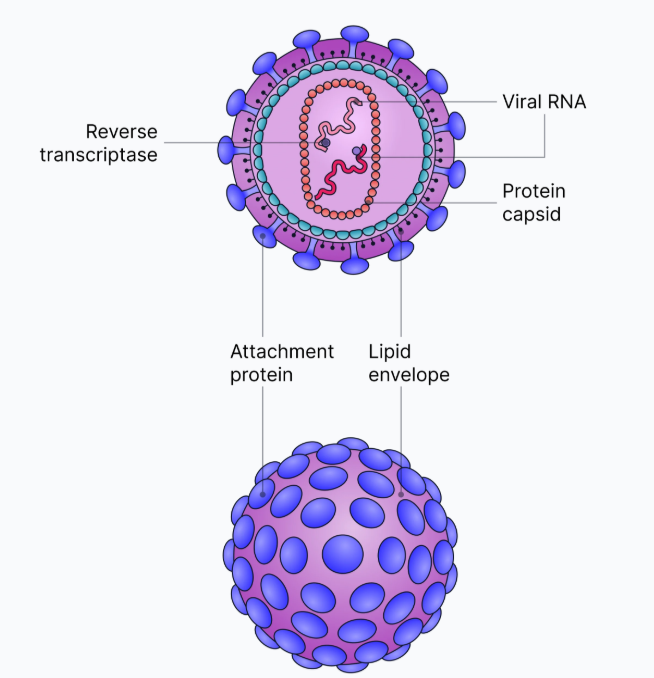
describe the sturcture of HIV
Lipid Envelope
Derived from the host cell membrane.
Contains attachment proteins that help the virus bind to T-helper cells.
Capsid
A protein coat that surrounds the genetic material.
Protects the viral RNA and enzymes inside.
Genetic Material (RNA)
HIV carries two single-stranded RNA molecules instead of DNA.
Contains genes for viral proteins.
Enzymes (Inside the Capsid)
Reverse Transcriptase: Converts viral RNA into DNA inside the host cell.
what is HIV effect on the immune system - how does it cause AIDS
HIV attacks T- helper cells- gradually reducing the number
Fewer T- helper cells= Bcells are not activated
Fewer B cells divide by mitosis/ undergo differentiation(or clonal expansion)-
fewer plasma cells- fewer antibodies produced
this comprimises the immune response- making the individual vunerable to infections
eventually AIDS develops, leading to life-threatening infections and cancers- only when the number of Helper T cells is critically low
define retrovirus ad reverse transcriptase
A virus that converts RNA into DNA using reverse transcriptase.
An enzyme that synthesises DNA from RNA.
Explain how HIV replicates inside a human cell. (6 marks)
HIV binds to the receptor on a T-helper cell using its attachment proteins.
The viral envelope fuses with the host cell membrane, and HIV RNA and enzymes enter the cell.- the viral capsid is uncoated and releases this
Insidethe cell, Reverse transcriptase converts viral RNA into a complementry strand of DNA.
Viral couble stranded DNA is incorporated/ inserted into the host cells chromosomes/ DNA
The host cell produces new HIV proteins from the viral DNA
The new viruses are assembled and bud off, destroying the T helper cell- weakening the immune system
describe why antibiotics don’t work against viruses
antibiotics kill bacteria by interfering with their metabolic reactions- they target the bacterial enzymes and ribosomes used in these reactions
bacterial enzymes and ribosomes are different from human enzymes and ribosomes. Antibiotics are designed to only target the bacterial ones so they don’t damage human cells
viruses don’t have their own enzymes and ribosomes- they use the ones in the host cells. Antibiotics therefore can’t inhibit viruses because they don’t targethuman processes
most antiviral drugs are designed to target the few virus-specific enzymes that exist. eg HIV uses reverse transcriptase to replicate- human cells don’t use this enzyme so drugs can be designed to inhibit it withoutaffecting the host cell. These drugs are called reverse transcriptase inhibitors.
describe how monoclonal antibodies can be used for monoclonal antibody therapy of cancer cells
different cells in the body have different surface antigens
monoclonal antibodies are produced that are specific to antigens on cancer cells (called tumour markers)- which arn’t found on normal cells
when the antibodies come into contact with the cancer cells they will bind to the tumour markers- so the drug will only accumulate in the body where the cancer cells are- side effects lower
you can also attach anti-cancer drugs to the antibodies
they attach to the surface of the cancer cells and block the chemical signals that stimulate their uncontrolled growth
describe how monoclonal antibodies can be used in medical diagnosis- pregnancy testing
the women would urinate on the end of the test strip. If she is pregnant, she will have HCG in her urine
as the urine diffuses up the test strip,it carries HCG to the reaction zone- where there are mobile antibodies
these mobile antibodies are specific for HCG- monoclonal, same tertiary structure, produced by B cells
HCG binds to the movile antibodies- which have a enzyme attached to them
mobile antibdies with HCG on their binding sites now move into test zone- which have a 2nd type of antibody that is complementry to HCG but are IMMOBILE
in the test zone, there is also the substrate for the enzyme, so if HCG was present and the mobile monoclonal antibodies bound to immobile antibodies in test zone, there is now a reastion whic gives a colour change- indicates pregnancy. OR dye beads carried by the reaction zone antibodies
control zone- shows if the test has worked. Third immobile antibody that will ind to any of the mobile antibodies that did not get fixed in the test zone(there is an excess). Again, could be enzyme - substarte colour reaction or dye beads carried
if not pregnant- no HCG, so can’t bind to test zone antibodies, but can bind to fixed antibodies in control window as those just bind to the mobile antibodies
define monoclonal antibody
Monoclonal antibody: identical antibodies, with the same tertiary structure, produced by clones of a single B lymphocyte.
whatis the ELISA test used for
a lab test to detect the presence of antigens or antibodies
describe some ethical issues associated with vaccines
all are testd on animals before humans-some disagree. Some animal based substances may also be used
testing on human- volunteers, unecessary risk- might not work
risk of side effects- but still protected by herd immunity
epidemic of new disease- who gets the vaccine first
describe some ethical issues withmonoclonal antibodies
animal rights issues- as animals produce the cells
what are the two types of ELISA test
The direct test - This uses only one antibody.
The indirect test - This uses two antibodies.
describe the ELISA test
Add the sample (containing the target protein) to a well plate where the target protein can attach to the well.
Add the antibody that is specific to the target protein. These antibodies will bind to the target proteins attached to the well.
Wash the well to remove any unbound antibodies.
Add a second antibody that will bind to the first antibody. These secondary antibodies are attached to an enzyme.
Wash the well again to remove any unbound secondary antibody.
Add a solution containing substrate to the well. The enzyme attached to the second antibody will act on the substrate to cause a colour change. The intensity of the colour indicates the quantity of protein present.
give two ways in qhich pathogens can cause disease
release toxins
kills cells/tissues