Lab 1 Homestasis, Feedback Mechanisms & Membrane Transport
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
40 Terms
Homeostasis
the ability to maintain internal stability
control mechanisms that allow the regulation of these variables consist of 3 components
1. receptor
2. Control centre
3. Effector
Control mechanism: Receptor
a receptor can be any type of sensor that monitors the environment. When a change in the environment (stimulus), is detected by the receptor , the receptor will send this information to the next component, the control centre
Control Mechanism: Control Centre (5 things)
5 Functions:
1. to establish a 'set point' for the variable- a level or range at which the variable must be miantained
2. to receive input from the receptors regarding stimuli that has been detected
3. to determine if the stimulus is strong enough to warrant a response.
4. to determine an appropriate response to the stimulus
5. to send information to the next component, the effector, about the response that is required.
Control Mechanism: Effector
the effector carries out the response as directed by the control centre. The response affects the stimulus is some way, either reducing it (- feedback) or enhancing (+ feedback)
2 mechanisms for maintaining homeostasis
positive and negative feedback mechanisms
steps of a homeostatic control mechanism
1. stimulus-produces change in variable
2. receptor- detects change
3. input-information sent along affect pathway to control center
4. output-information sent along efferent pathway to effector
5. response of effector feeds back to reduce the effect of stimulus and returns variable to homeostatic level
Negative feedback mechanisms
the course of action that us implemented in response to a stimulus acts to reverse the change in the environment. this causes the variable to change in a direction opposite to that of the original change that lead to a stimulus.
-main mechanisms used for maintaining homeostasis in the body
-usually control the functions that occur regularly and require great stability
three main example of negative feedback mechanisms
blood pressure
body temperature
hormonal secretion
negative feedback mechanisms- Blood Pressure
an increase in arterial blood pressure is sensed by receptors in the heart wall. These receptors send a message to the cardiac centre of the brainstem which, in turn, sends nervous signals back to the heart to decrease hart rate and, therefore, decrease blood pressure
High B.P-->Receptors-->Cardiac Centre-->Heart-->decreased heart rate--> decrease BP
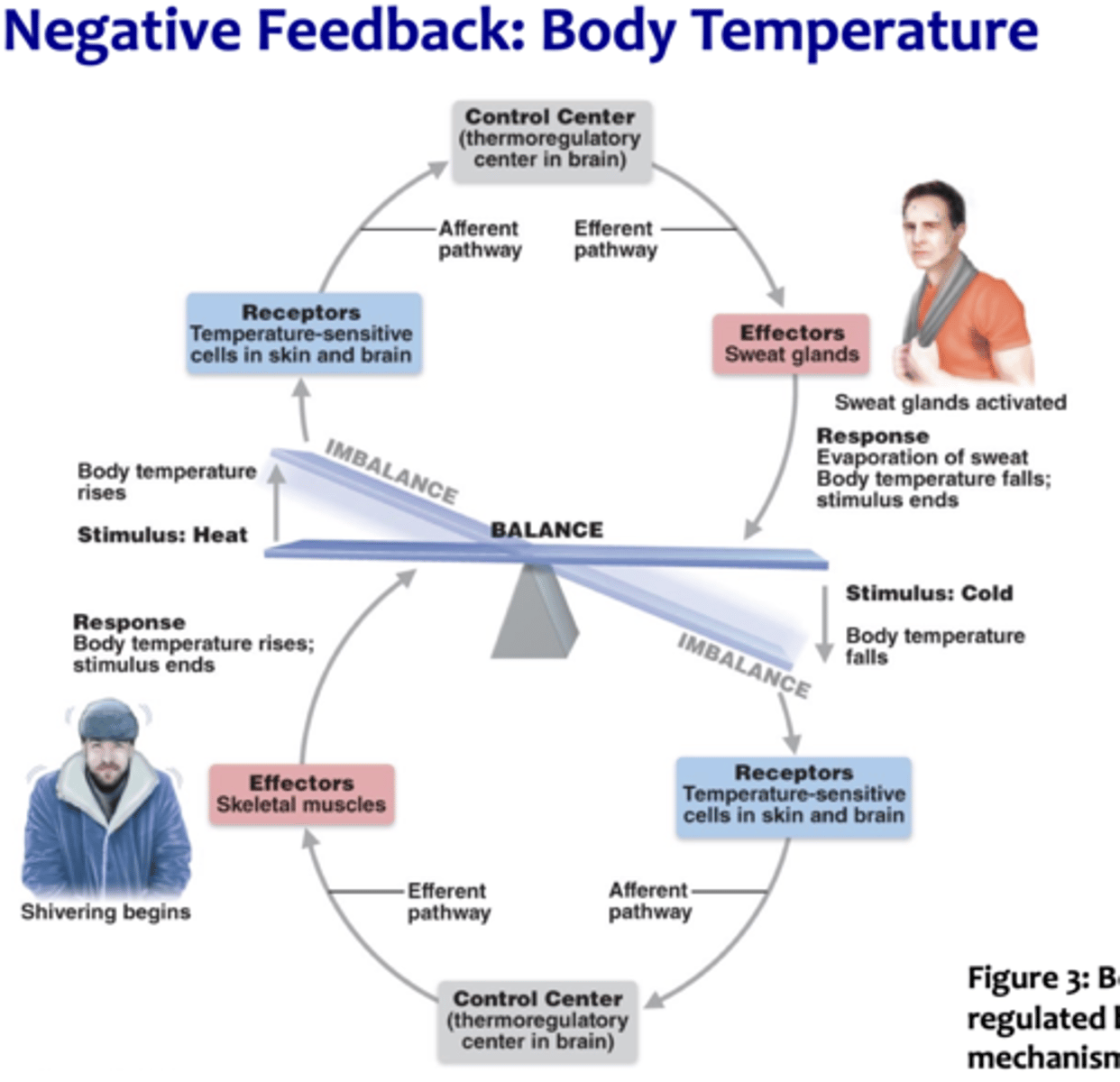
Negative Feedback Mechanisms- Body Temperature
your internal "thermostat" consists of a group of nerve cells at the base of the brain that monitors blood temperature. If you become overheated, this "thermostat" triggers mechanisms to lose heat, such as sweating and vasodilation (widening of the blood vessels_. If you become too cold, the thermostat triggers mechanisms to conserve heat, such as shivering and vasoconstriction (narrowing)
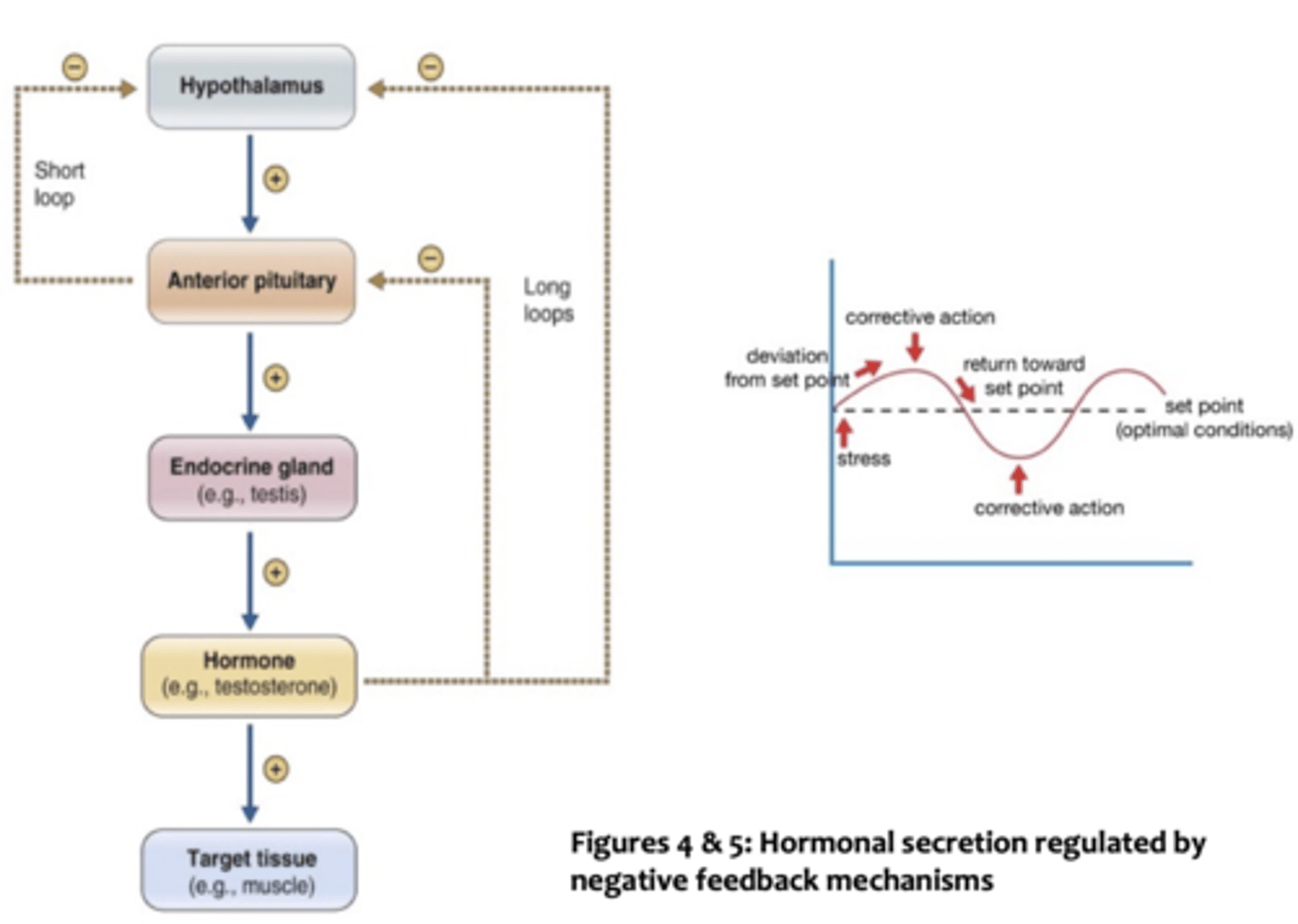
Negative Feedback Mechanisms- Hormonal Secretion:
the majority of hormones in our body produces are under negative feedback control. This allows an endocrine gland (and its control systems) to be sensitive to the levels of hormone released into circulation. if the level of hormone increases to a certain concentration, the endocrine gland in inhibited from releasing more hormones until levels decrease. if the concentration of hormone drops too low, inhibition ceases.
regulation of body temp via - feedback mechanism diagram
capillaries in the face and chest are close to the skin
** vasodilation of capillaries that are close to the skin and allows for radiation heat loss
**vasoconstriction of capillaries allows for blood cooling. conserve heat loss to environment
positive feedback mechanisms
in the case of positive feedback mechanisms, the body senses a change in homeostasis but activates mechanisms that lead to an even greater change in the same direction. this is completely contrary to the corrective effect of negative feedback.
-usually control functions that occur infrequently and rapidly,
examples of + feedback mechansims
release of oxytocin during childbirth
blood clotting
Positive feedback- Release of Oxytocin During childbirth
oxytocin is a hormone that stimulates contraction of the uterine muscles during childbirth. these contractions push an unborn child against the mother's cervix. nerve endings in the cervix send signals to the brain which, in turn, stimulates the pituitary gland to secrete more oxytocin
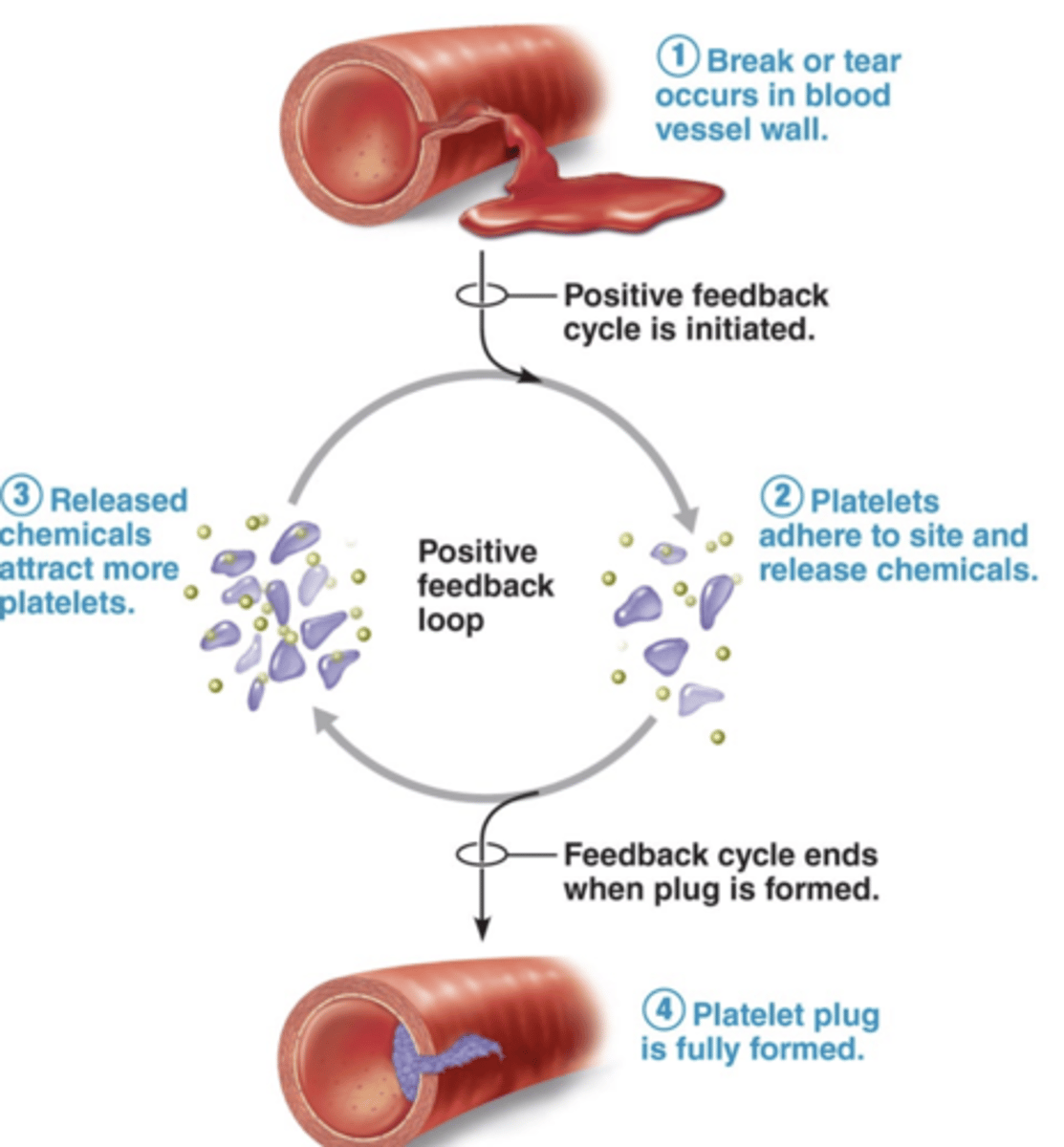
Positive feedback mechanisms- Blood Clotting
When there is a break in a blood vessel, elements in the blood called platelets stick to the injured site and release chemicals to attract even more platelets. The cycle ends when the break is sealed
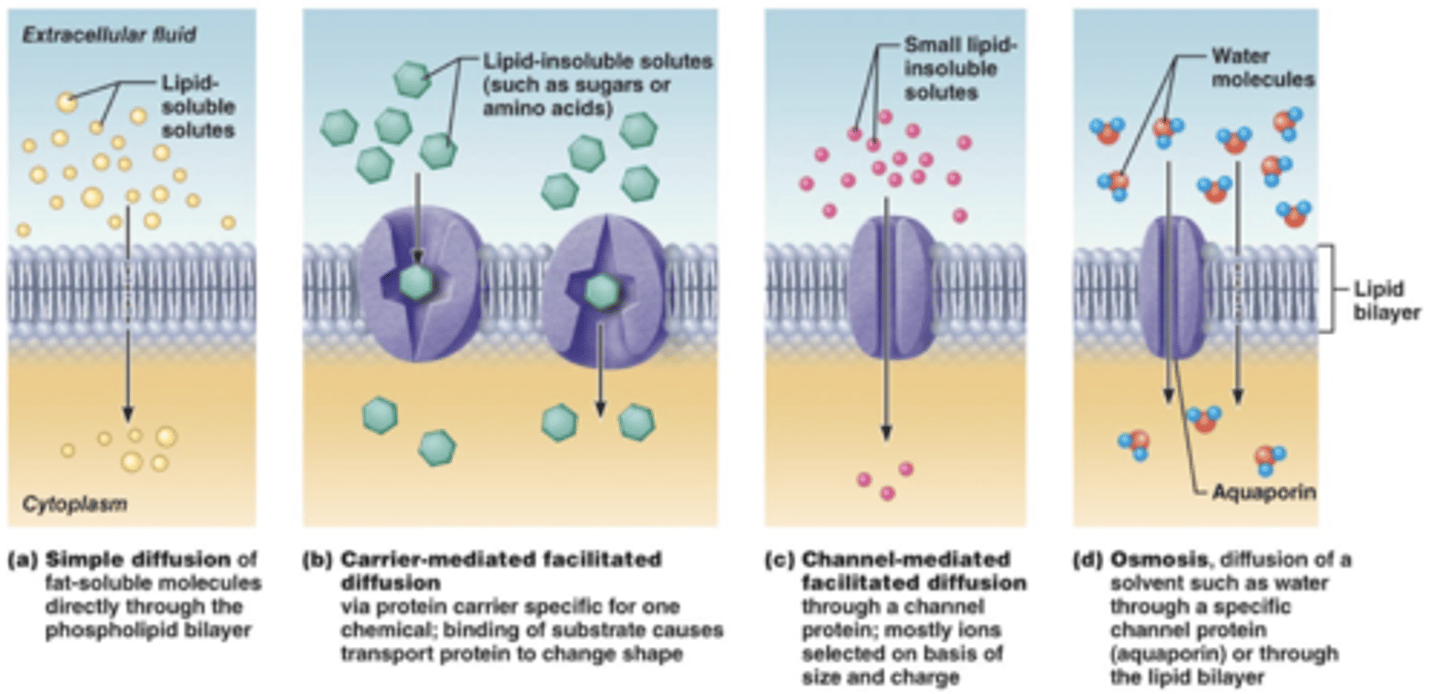
Passive processes
simple diffusion
facilitated diffusion
osmosis
simple diffusion
used by non-polar and lipid soluble molecules to diffuse through the lipid bilayer of our cells
Facilitated diffusion
molecules that are unable to diffuse through the lipid bilayer require assistance to be transported through the membrane
Carrier-mediated diffusion: the substance binds to a carrier protein that transports the molecules through the membrane
Channel-mediated diffusion: the substance crosses the membrane by moving through channels.
osmosis
movement of a solvent (such as water) through a selectively permeable membrane. Water can cross the lipid bilayer by either sliding through random gaps in the membrane lipids that form or by using specific protein channels called aquaporins
active transport
molecules being transported require carrier proteins to move solutes up the concentration gradient from an area where they are less concentrated to a region where they are becoming increasingly more concentrated. Active transporters are also called solute pumps
primary active transport
the energy to carry out this process comes directly from the hydrolysis of ATP. Phosphorylation (the addition of Pi) activates the transport protein allowing it to pump the solute across the membrane.
secondary active transport
An ATP powered pump (primary active transport) indirectly drives this process. As charged solutes are moved across the membrane against the concentration, the pump stores energy (ion gradient). The solute is able to "leak" back across the membrane, travelling down its concentration gradient, carrying other substance with it in the process.
Vesicular trasnport
fluids containing large particles and macromolecules are too large to be transported via channels and pumps. they must be packages inside membranous sacs called vesicles to be moves into (endocytosis) or out of (exocytosis) the cell. This method is also used to move substances from one area of a cell to another (transcytosis) or get a substance into, across, and out of a cell (vesicular trafficking)
Phagocytosis:
Large or solid materials are brought into the cell by engulfing it with cytoplasmic extensions (pseudopods) to form a phagosome
pinocytosis
small volumes of liquid are brought into the cell after it comes into contact with a protein-coated pit. contact triggers the infolding of the plasma membrane, which pinches off to form a small vesicle.
receptor-mediated endocytosis
this is a selective mechanism that utilizes plasma membrane proteins (receptors) for specific substances to be recognized, ingested, and concentrated within the cell.
could be dose dependant
Plasma Membrane-Generating a Membrane Potential pt 1
-charged particles on either side
-membrane potential (M.P) of -50 to -100 mV
-creates polarized state
-Mainly determined by K+. K+ is in high concentration inside the cell
-K+ diffuses out via leakage channels, loss of positive makes the inside of the cell negative
-Na+ is rich outside the cell so there is an influx of Na making the M.P = -70mV
-Membrane is also permeable to Cl- but they don't contribute to membrane potential because they are balanced
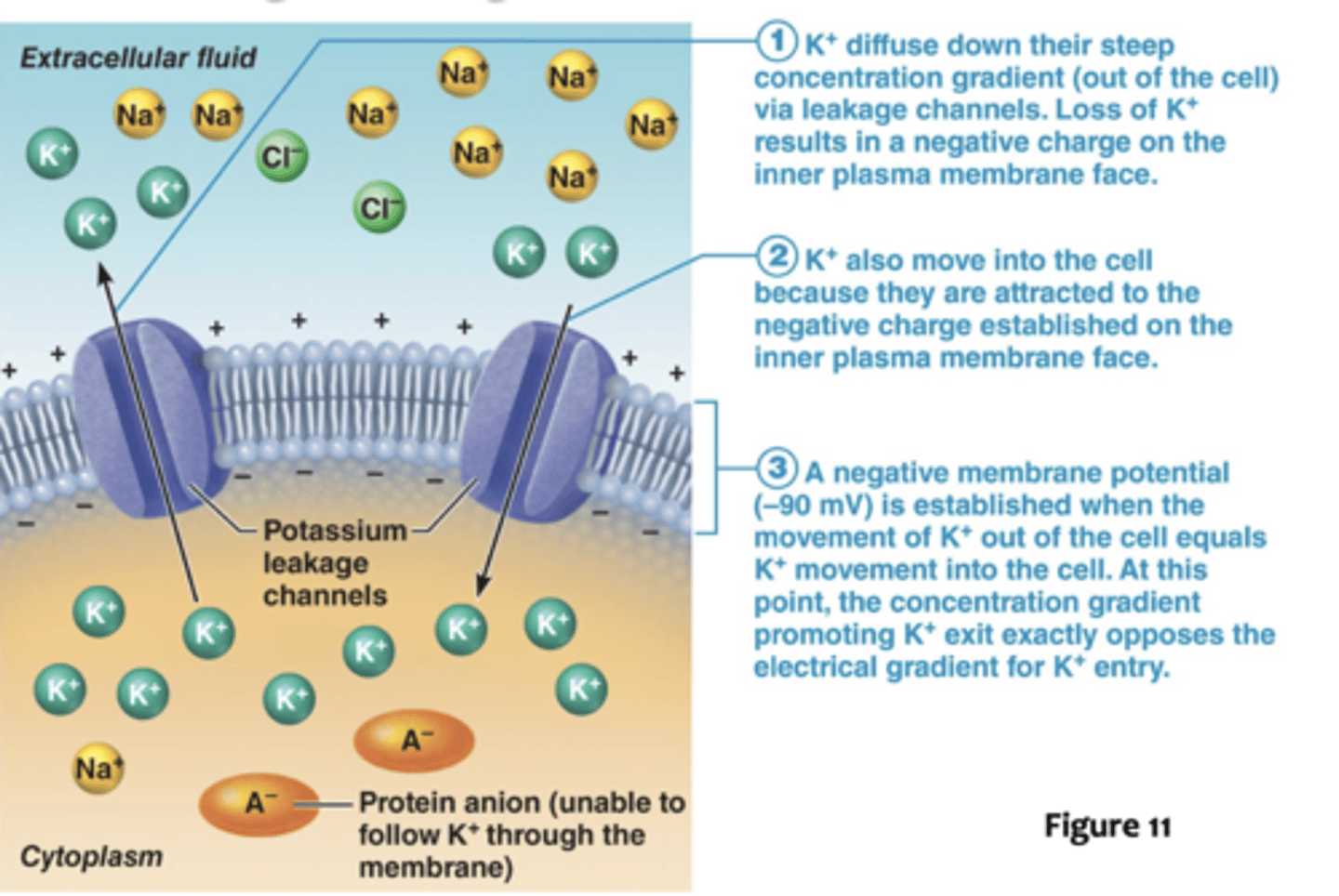
Plasma Membrane-Generating a Membrane Potential part 2
-the negative charge of the inner side of the plasma membrane prevents further loos of K+ past -90mV
-at this point M.P matches potassium conc. gradient therefore 1 K+ lost 1 K+ gained.
-the key to maintaining charge separation is to prevent the ion gradients from achieving equilibrium.
-Active Transport achieved by ATP dependent Na/K pumps is responsible for maintaining M.P
-the rate of active transport depends on how much Na+ has diffused into the cell. The exchange isn't 1:1.
-3 Na+ pumped out 2 K+ pumped in.
What would happen to our cells if Na+ was not continuously pumped out?
Water follows sodium ions, therefore all the excess water in the cell (which has followed the sodium ions) would cause the cell to lyse.
Why is less K+ pumped into the cell via the Na/K pumps compared to Na+
...
Identify the type of substance that can move across the plasma membrane using channel-mediated facilitated transport.
small lipid insoluble solutes (such as ions pass) through the plasma membrane using channel mediated facilitated transport.
Which is not a characteristic associated with the control centre in maintaining homeostasis in the human body?
a. Establish a normal range of activity for that suystem
b.Receiving incoming information from receptors that have detected a change in activity levels in a system
c.Determining what type of response is needed in response to changes in activity for a body function
d.Detecting a change in activity levels within a system
What body structure serves as the effector in the regulation of blood pressure.
heart muscle
What serves as the effector in the feedback mechanism involved in oxytocin release during childbirth
uterine muscle contractions
Which type of membrane transport does not require the use of energy or any form of stimulation for it's ability to permit ions to move from one side of the plasma membrane to the other?
leakage channels
What drives the activities associated with secondary transport?
primary transport-established concentration gradients
Which cells in our bodies possess Na+/K+ pumps on their plasma membrane?
all cells
What has the greatest influence in establishing the resting membrane potential of a cell?
POTASSIUM