Spinal cord injury
1/84
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
85 Terms
Learning Objectives
Review spinal cord neuroanatomy
Understand spinal cord injury (SCI) epidemiology and pathophysiology
Describe the common secondary complications following SCI
Spinal Cord Neuroanatomy Review
Grey matter vs white matter?
grey-cell bodies
white-tracts that carry info
grey matter
-neurons
-glial cells
astrocytes
microglia
oligo
schwann
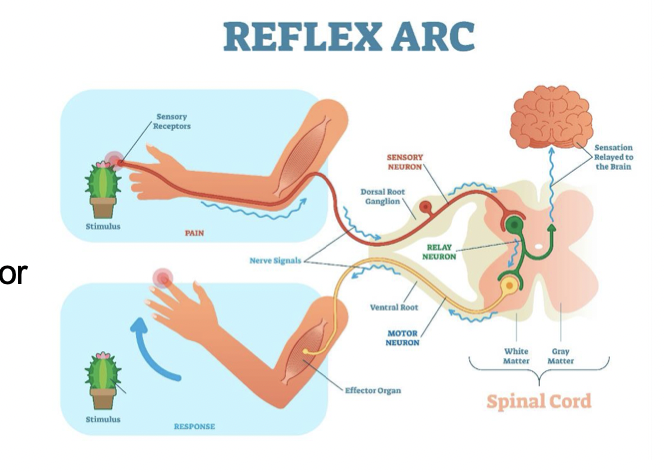
Spinal tracts
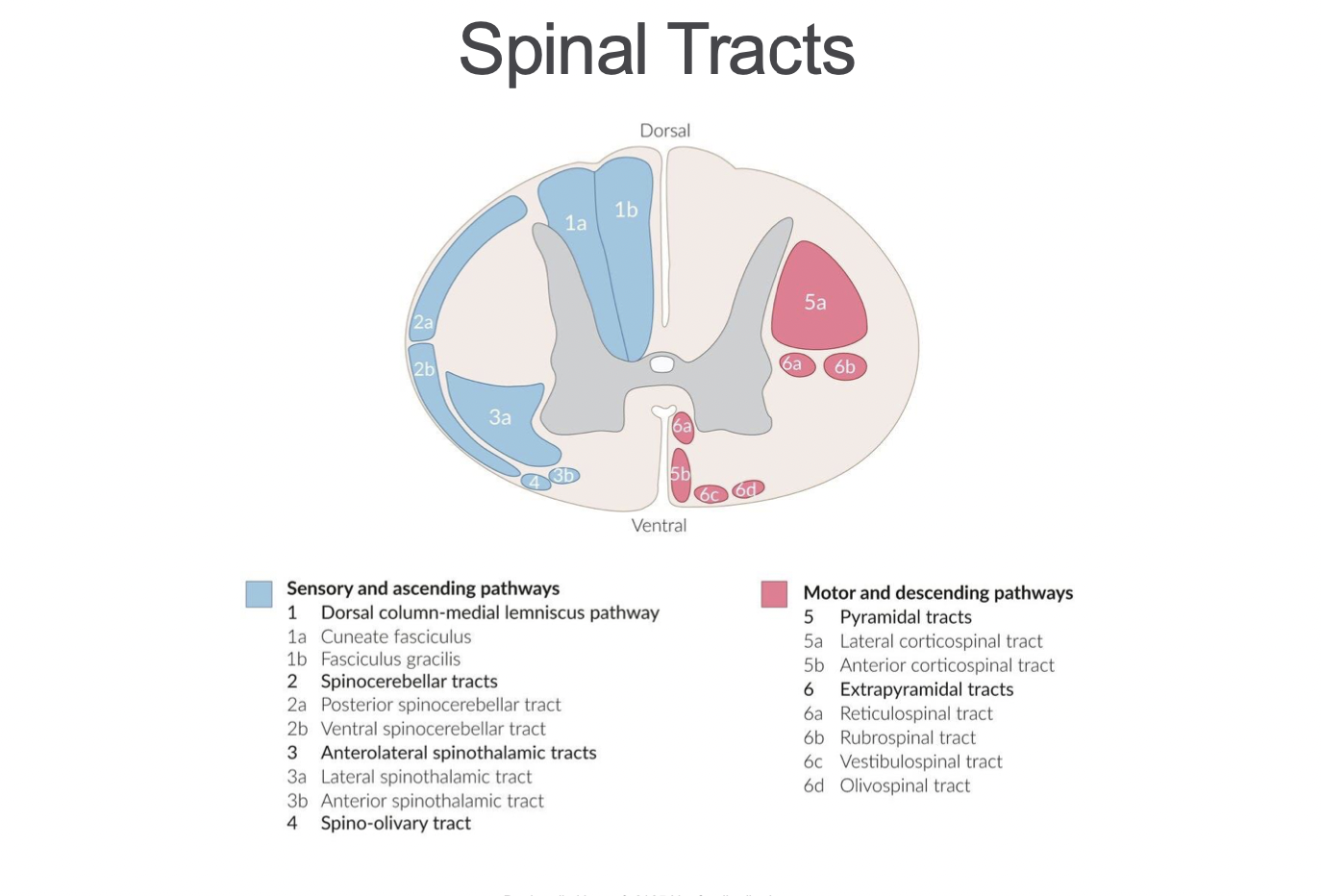
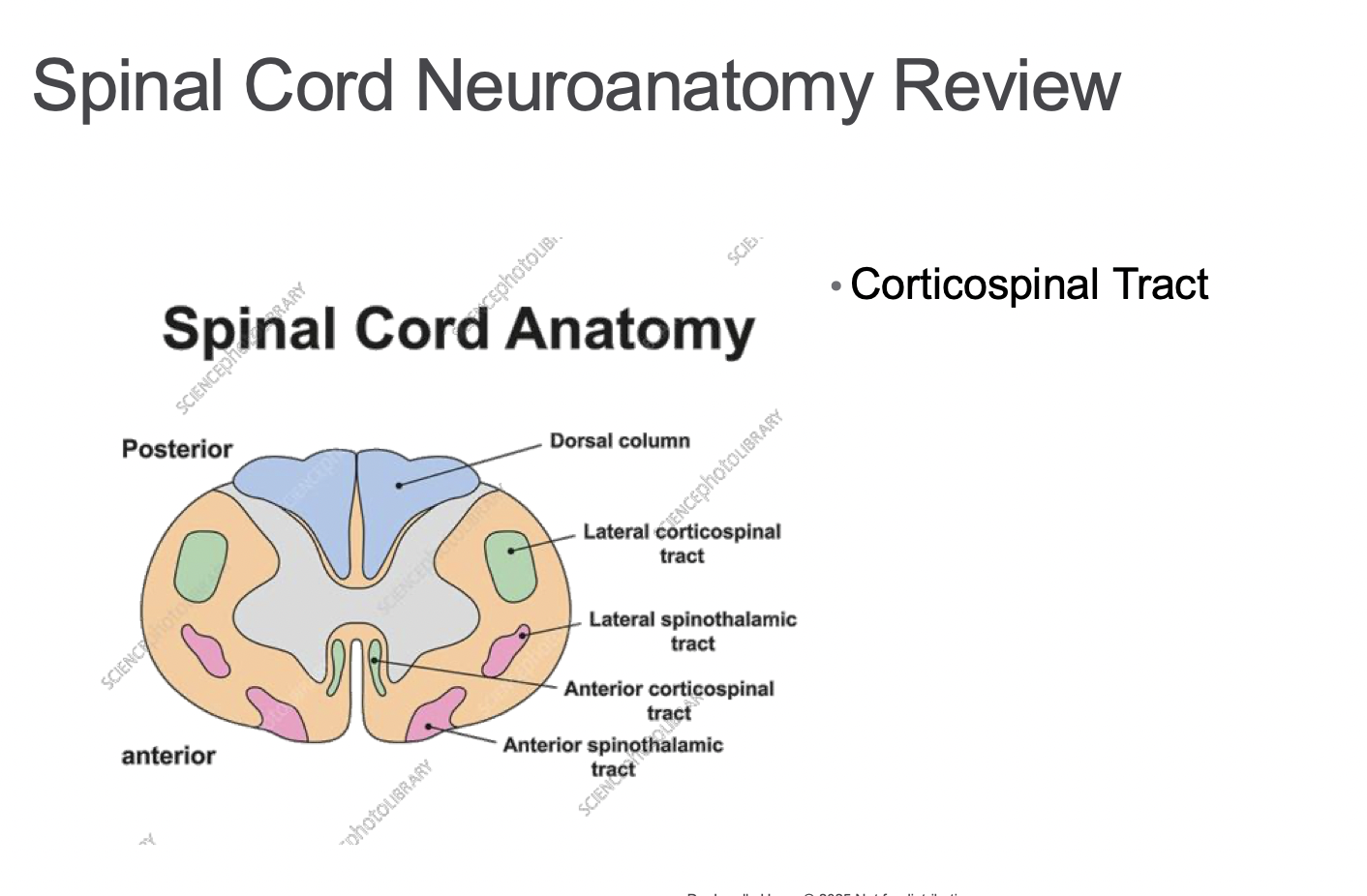
Spinal cord neuroanatomy review: Corticospinal tracts
-originates in motor cortex
Lateral- voluntary mvmt
-decussates in the medulla
Anterior- postural stability
-decussates at the level of termination -crosses over right before it exits the SC
Cervical → sacral (medial → lateral)
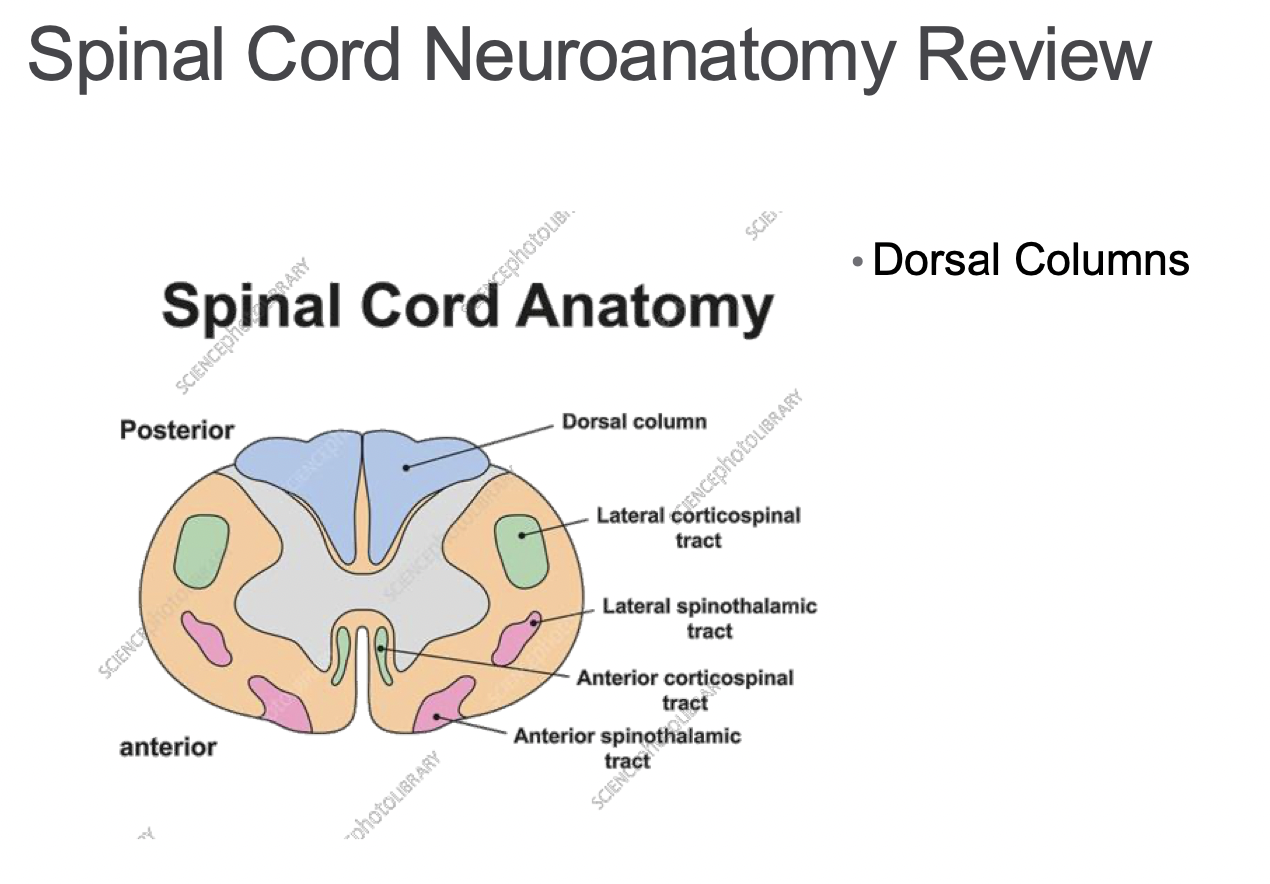
Spinal cord neuroanatomy review: Dorsal columns
-transmits to sensory cortex:
-discriminative touch
-pressure and vibration
-conscious proprioception- awareness of where our body is in space
Faciculus gracilis )entire cord primarily related to legs) and
Fasciclus cuneatus T6 and above
Sacral → cervical (medial → lateral)
Decussates in medulla
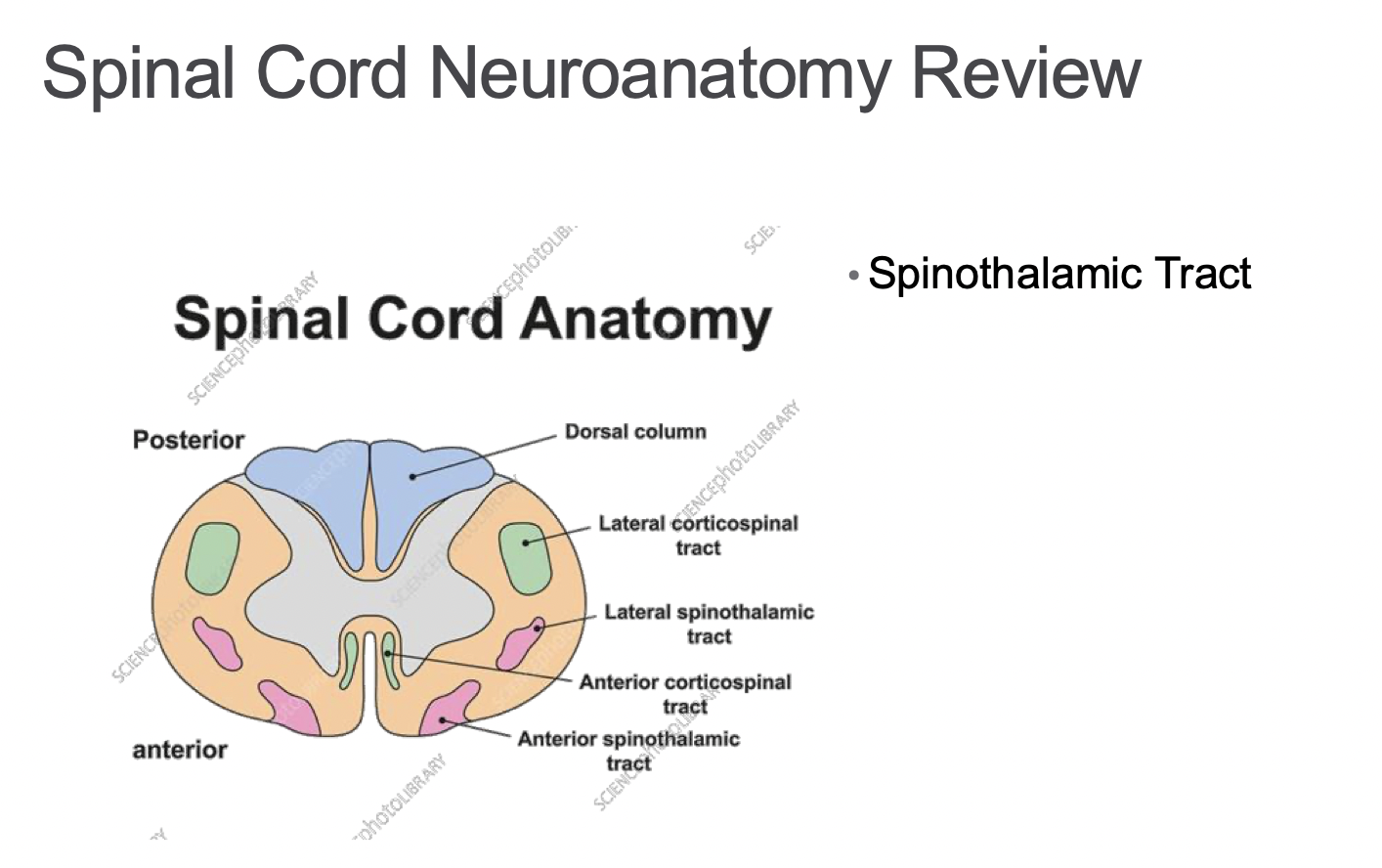
Spinal cord neuroanatomy review: Spinothalamic tracts
Anterior- crude touch (itches, tickles) not rlly specific location
Lateral -pain and temperature
Cervical → sacral (medial → lateral)
Deccusates 1-2 spinal levels above entry
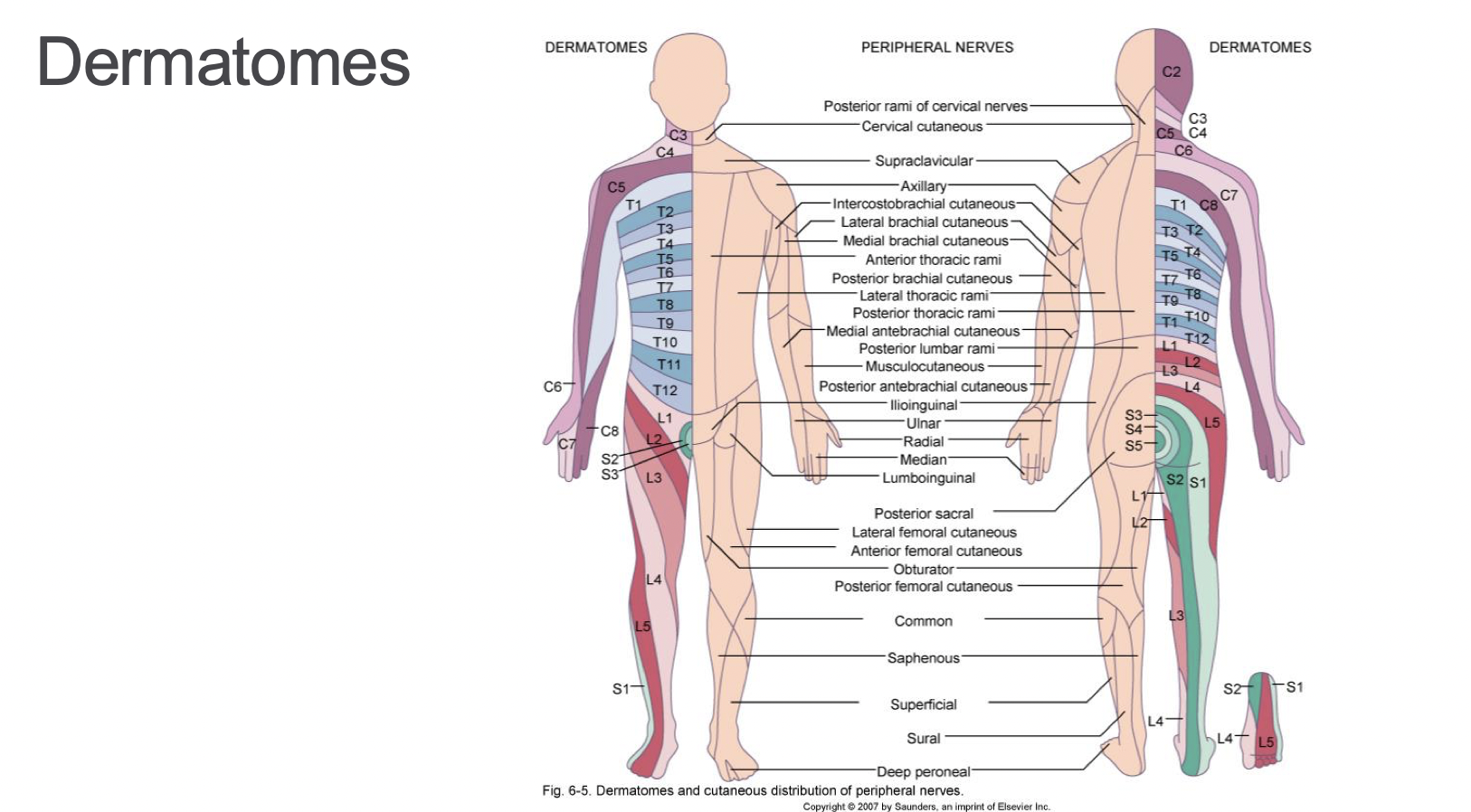
Dermatomes
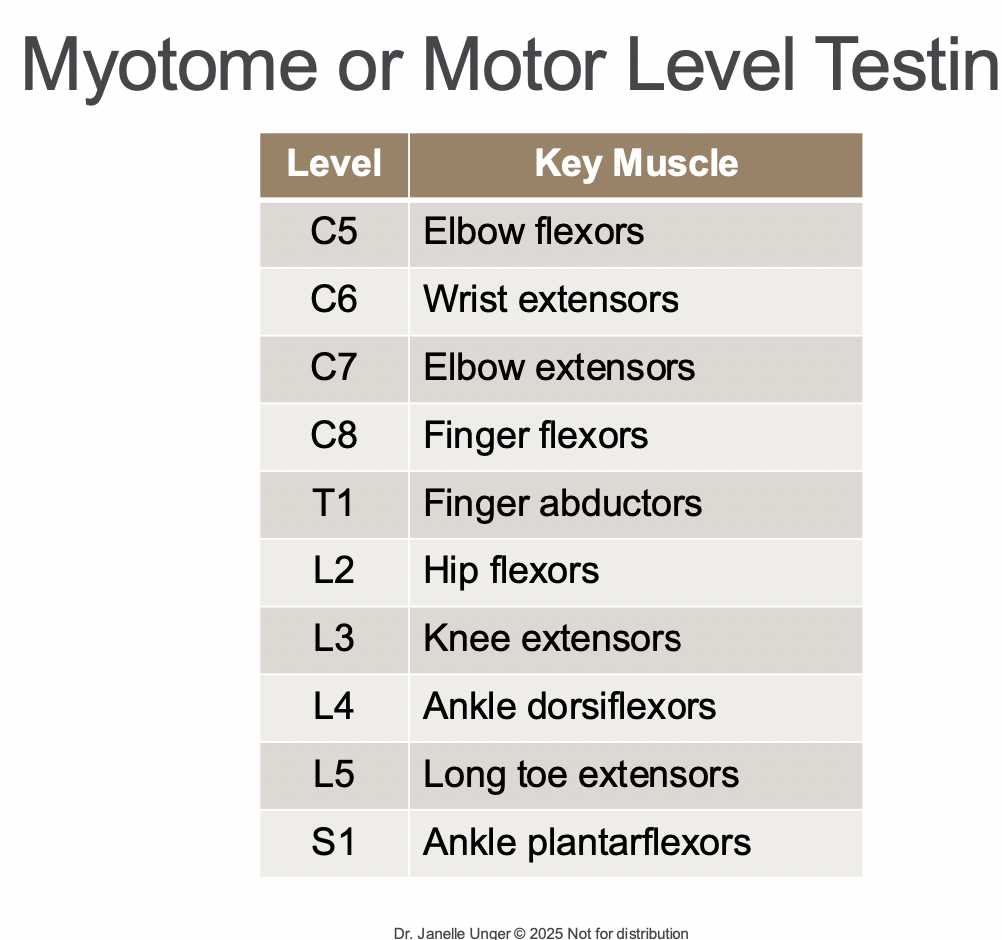
Myotome or motor level testing
movements not muscles- rlly hard to test only 1 muscle,
every nerve root contains more than muscle- creates a redundancy
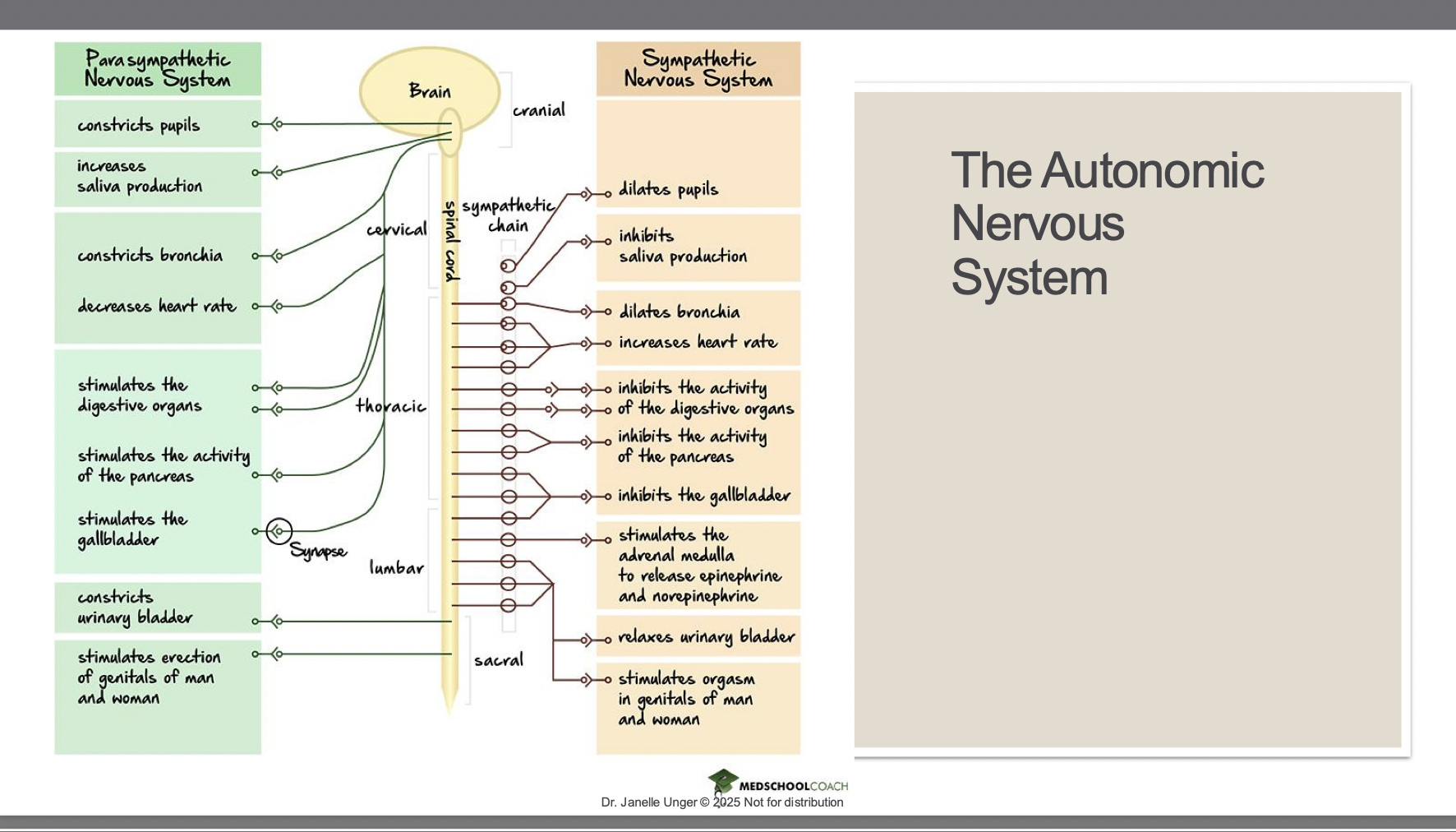
The autonomic nervous system
EPIDEMIOLOGY AND PATHOPHYSIOLOGY
Defining SCI
When temporary or permanent impairment occurs due to damage to the spinal cord
*different than a spine injury (just the vertebra damaged) this has to have the neural component with it
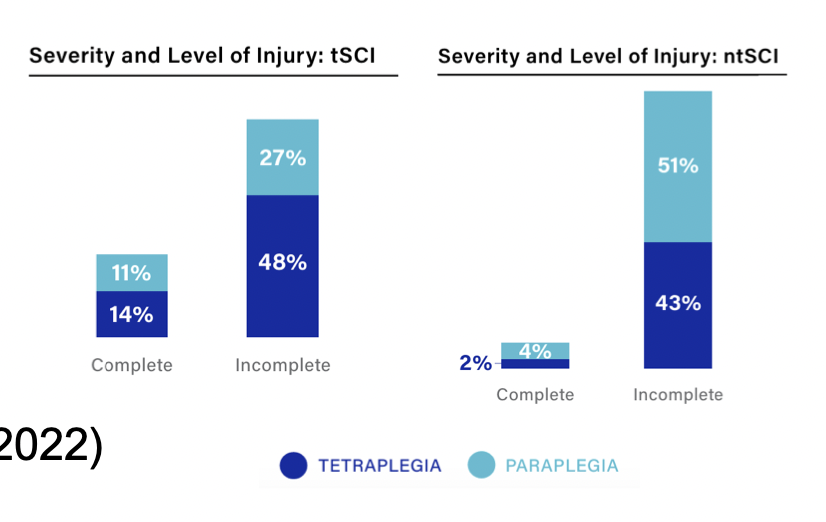
Classification of SCI
• Traumatic versus non-traumatic
• Tetraplegia versus paraplegia (quadplegia is an old term)
• Complete versus incomplete
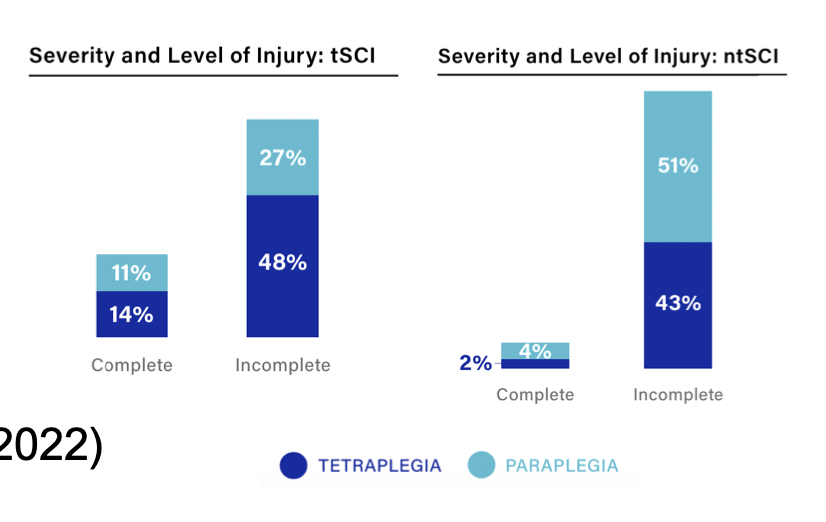
Epidemiology of SCI
In Canada, > 86,000 people living with SCI (Praxis Spinal Cord Institute, 2020-2022)
• 30,000 have a traumatic injury
• Estimated costs: >2 million per person (lifetime)
*not as prevalent as stroke, lots of more money because of sci (loss of income, rehab, usually occurs younger, more years to live)
• Annual cost to healthcare system: 2.7 billion
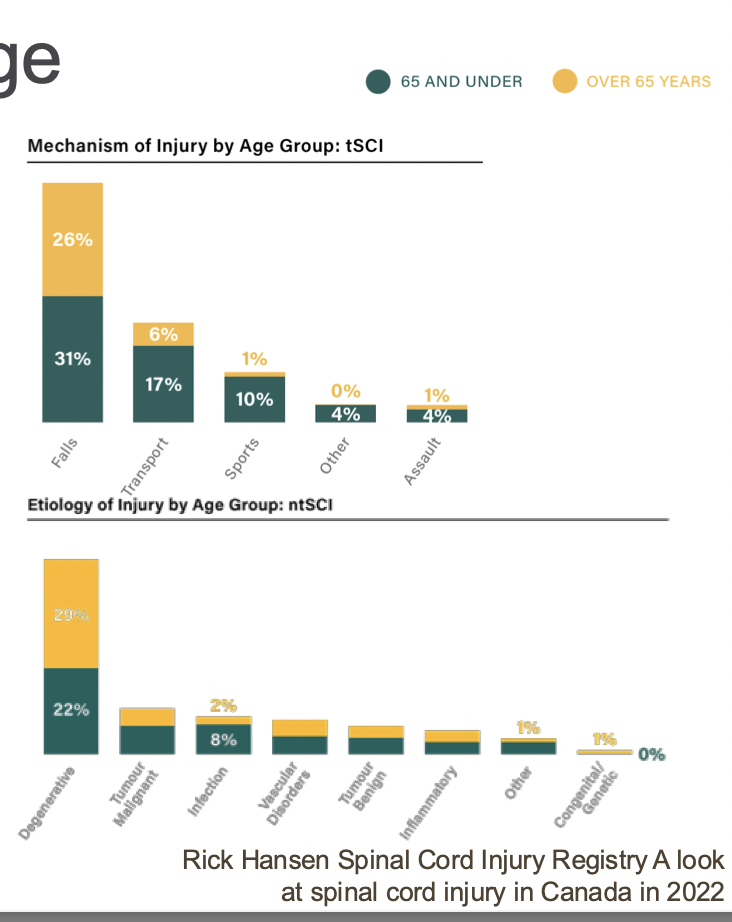
Impact of age
• Average age of SCI incidence is increasing – why?
-use to think of males and age 30,
people live longer, non-traumatic, safety measures put in place (mandatory seatbeat)- was a leading cause before
WHOs falling- typically older adults
• Traumatic injuries typically affect younger individuals (~55), non-traumatic injuries typically affect older individuals (~62)
• Sex/Gender differences
• Traumatic injuries affect men more than women
Ratio 3:1 76%-79% men due to risk taking behaviours
• Non-traumatic injuries affect men and women more equally (64% male)
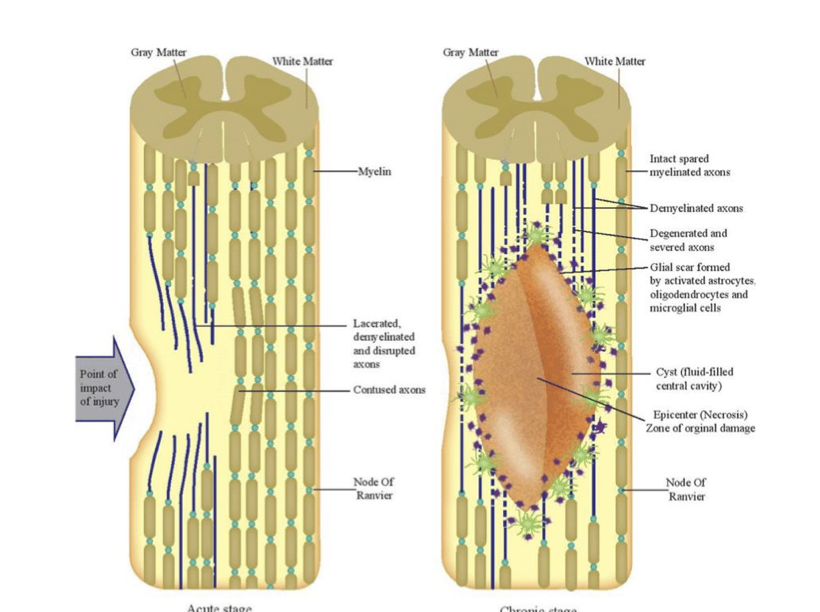
Pathophysiology- primary
• Non-traumatic injuries depend on disease process
• Traumatic injuries follow similar pattern
• Primary (usally due to ischemia or lack of bf)
Ischemia is one of the main determinants for SCI severity (along with duration of compression)
Initial mechanism: 1) Impact plus persistent compression; 2) Impact alone with transient compression; 3) Distraction (SC pulled w traction) ; 4) Laceration/transection (stab or gunshot wound)
Destruction of neural tissue (parenchyma), axonal networks, and glial membrane, hemorrhaging
Clotting and edema exert pressure on surrounding tissues → further ischemia- just cascades down
Cells stop signalling as usual → called spinal shock
Acute phase of SCI- secondary injury cascade
• Vascular dysfunction* (hemorrhage and hypotension in microcirculation)
• Ischemia results in endothelial damage → damages membrane and ionic dysregulation (influx of Ca2 in cell because easier to get in)
• Excitotoxicity caused by excessive glutamate from cells dying and releasing toxins
• Neuronal apoptosis and necrosis (including oligodendrocytes → demyelination)
• Acute Axonal Degeneration 15 mins after initial injury – both anterograde (Wallerian) and retrograde (dieback)- axons dying from both ends
Sub-acute phase of SCI
• Free radical injury, lipid peroxidation, immune-associated neurotoxicity
• Glial scar begins to form- creates the big problem with us takes us into chronic phase of injury- fully formed with 2-3 weeks
Chronic phase- secondary injury cascade
• Continued degeneration of axons
• Glial scar (astrocytes are structural cells responsible for this) formation
• Cells inside the scar die, resulting in a fluid-filled cyst
Difficult area for healing because:
• Glial scar prevents cells from entering
• No structural cells within this (bc its fluid) to support axon growth within cyst
*lost all of the axons that exist in the area
Spinal Shock
-loss of descending input resulting in increased inhbition (not active as much anymore)
• Loss of excitation and descending input, increased inhibition
• Dampened or absent spinal reflexes and hypotonicity (low muscle tone)- tone goes away right after injury
• Neurogenic shock refers to hemodynamic instability (drop in BF, BP)
• Hypotension, bradycardia, and hypothermia (cervical injuries – why?)
-baroreceptors in there, autonomic system those cardiac are within thoracic (and lost cervical so lose that ability to come from brain)
Resolves in phases, typically completely resolves after year
Resolves in phases, typically completely resolved after 1 year
• Phase 1 (0-1 day): areflexia/hyporeflexia – DPR onset (delayed plantar response)
• Phase 2 (1-3 days): initial reflex return – pathological (babinski- not a good sign) and cutaneous reflexes come back on
• Phase 3 (1-4 weeks): initial hyper-reflexia – DTR onset (deep tendon reflex), DPR integration
• Phase 4 (1-12 months): final hyper-reflexia – spasms, neurogenic bowel/bladder, AD
*ppl have hyper-reflexia last after SCI
*when someone first injured almost completely flaccid its very concerning they think they will always be like that- just spinal shock- but it can come back
C-spine stable injuries
• Vertebral components won’t be displaced with movement or loading
• Intact ligaments
• No danger of secondary neurological injury (1/3 spinal columns damaged)
• Does not usually require operative management
C-spine unstable injuries
• Unable to tolerate loading without incurring neurological deficit or pain
• Failure of spinal columns (2/3 damaged)
• At risk for neurological injury if not protected
• Require operative management for stabilization
Spinal columns
1/3 stable
2/3 unstable
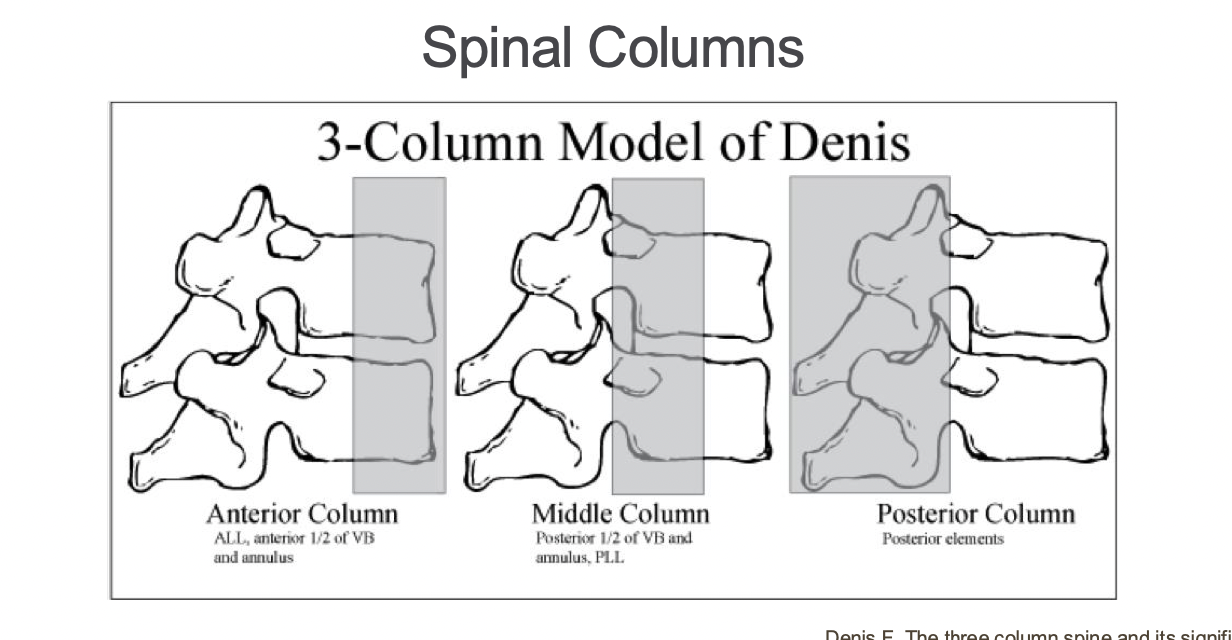
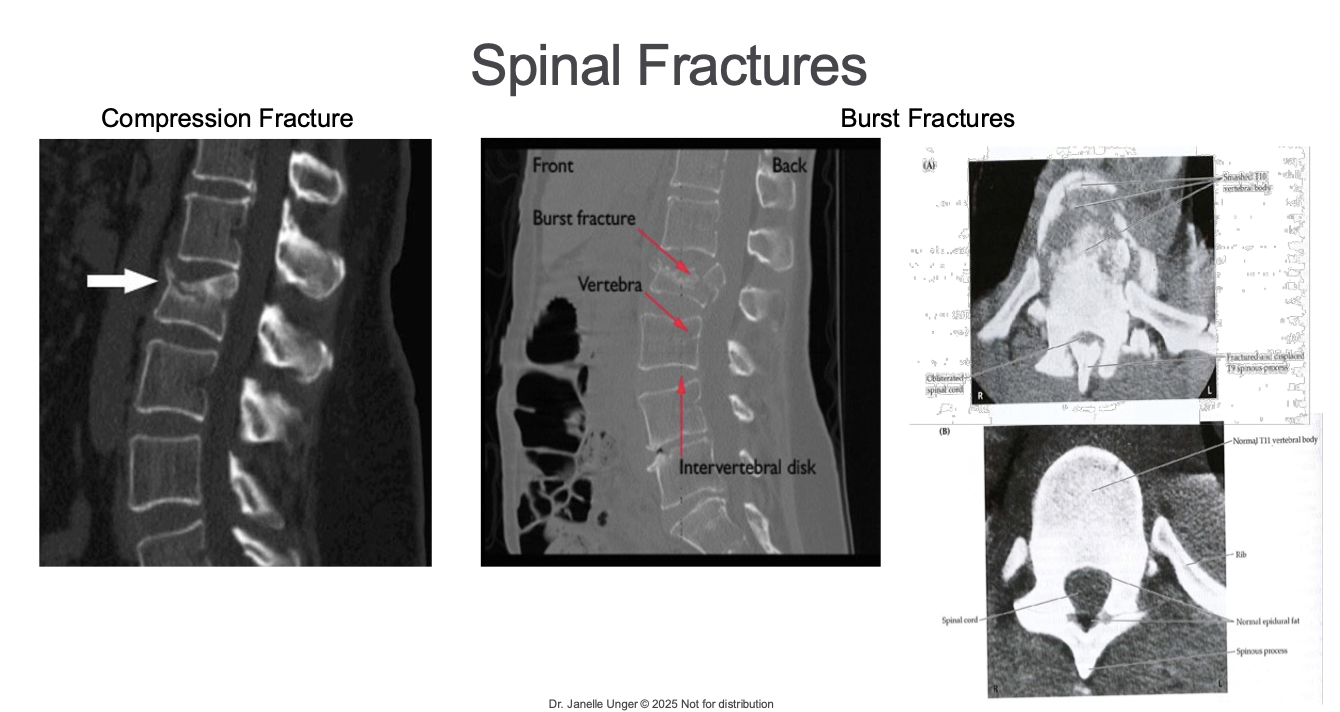
Compression fractures
• Decreased vertical height of vertebrae in anterior column often from degeneration
(e.g., osteoporosis), typically stable
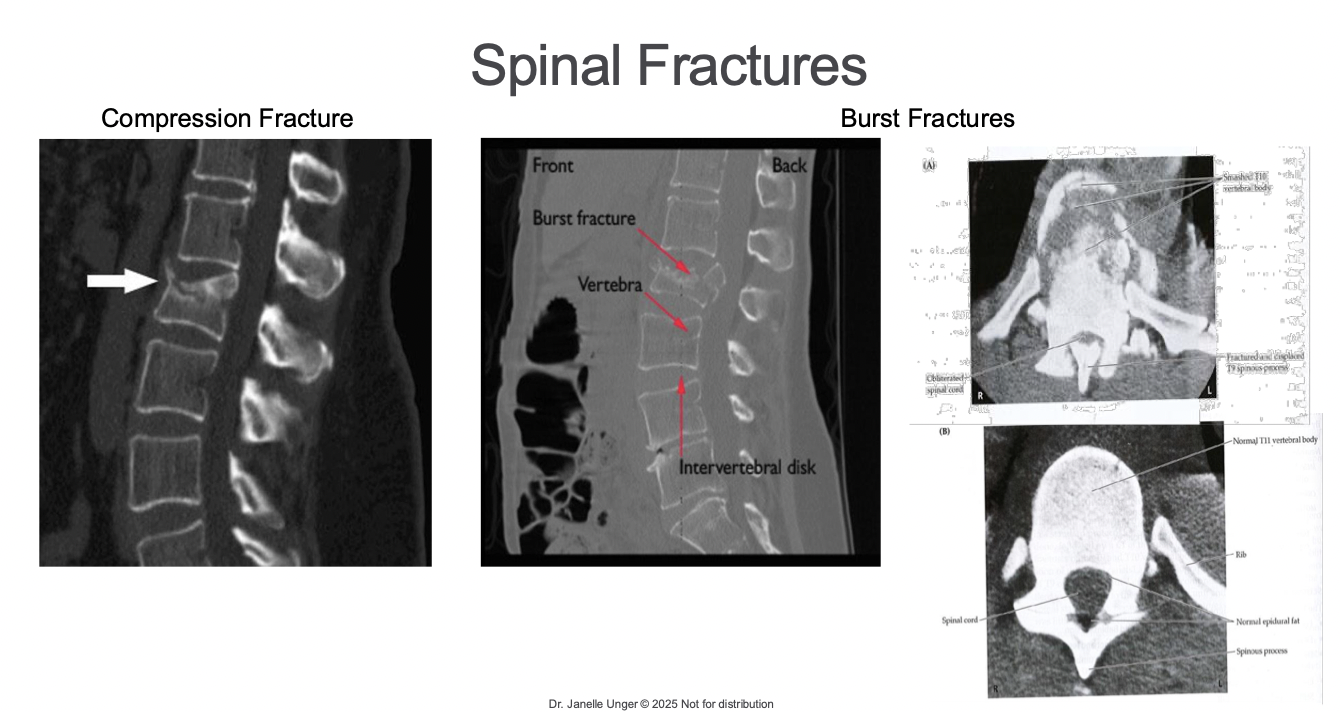
Burst fractures
• High axial load, decreased vertical height of vertebrae in both anterior and middle column, typically unstable and can have shards of bone projected into cord
e.g. gymnast in shallow put, force transmits up and broke her neck
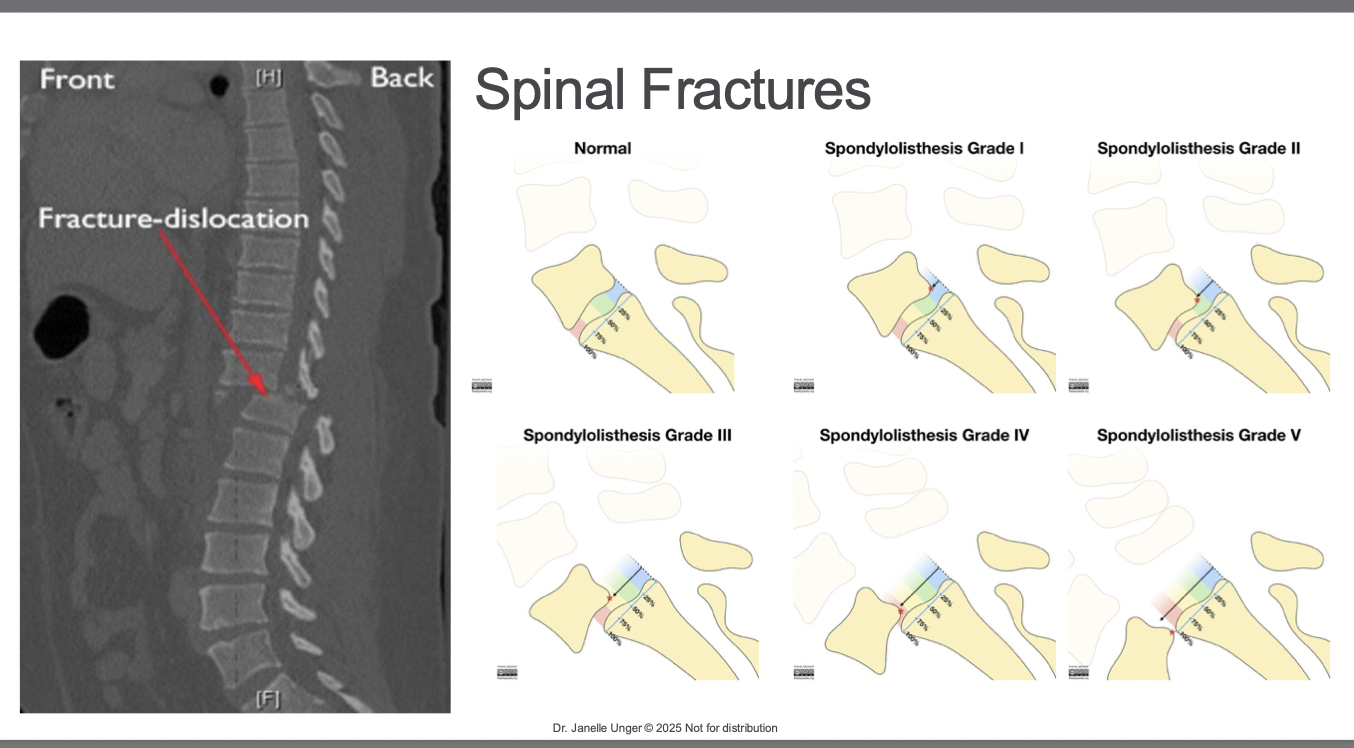
Fracture/Dislocation (Spondylolisthesis)
• Results from hyperflexion or hyperextension with possible rotational component typically unstable and compress the spinal cord
*typically see in MVA, rotation of head
grade the amount of dislocation
grade 5- one completely slipped off the other vertebra
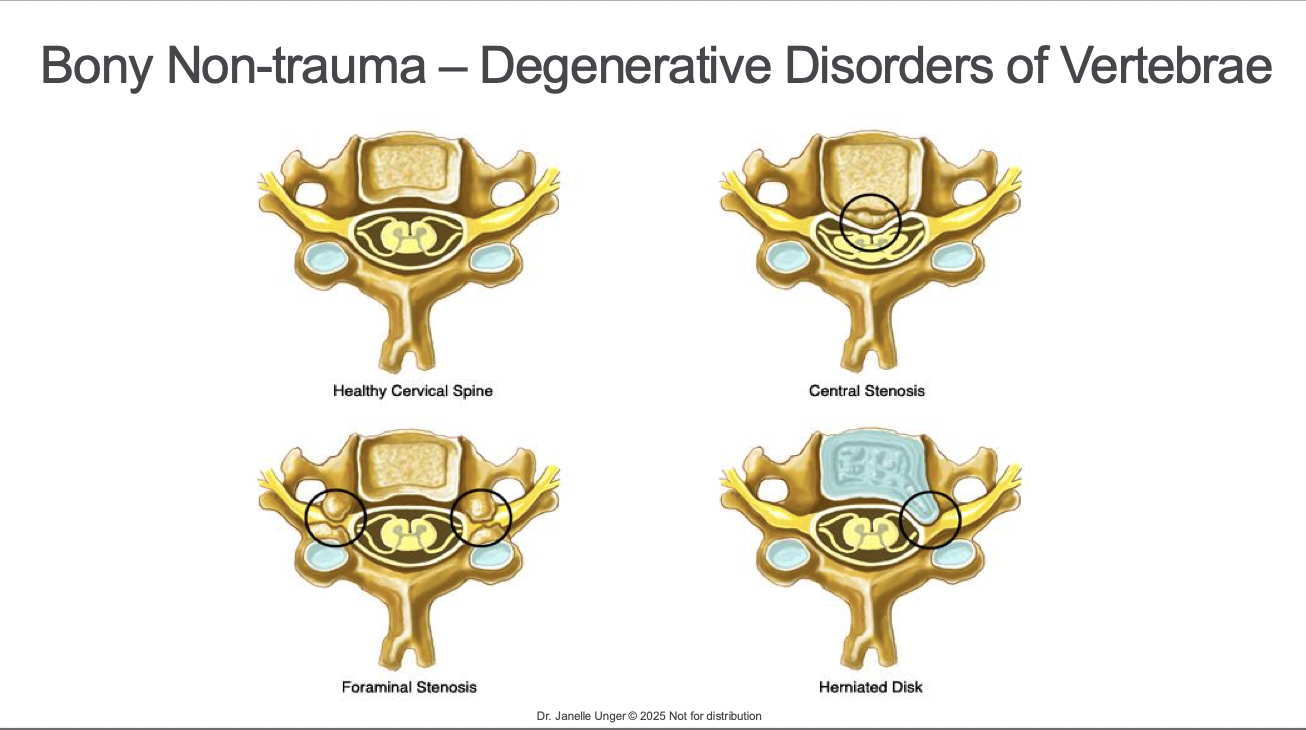
Bony non trauma- degenerative disorders of vertebrae
central stenosisi- disc bulding out- directly compresses the SC
for- compresses neural foramen where nerve roots exit thru vertebra- nerve roots
herniated- nerve roots but can impact cord-
Social Impacts After Spinal Cord Injury
40% were employed become unemployed after 5 years, huge loss of income after a SCI
-not see dec in relationships die to caregiving role anymore
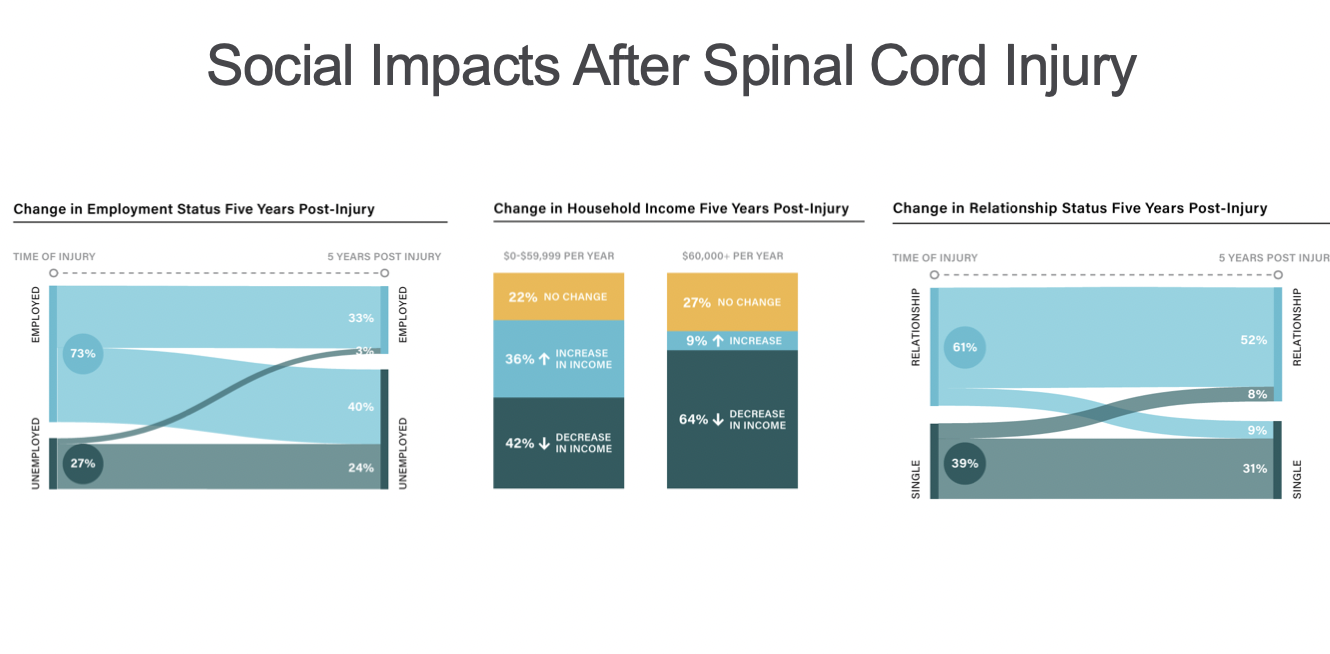
Social impacts after sci
data only for traumatic injuries
priv- their own home not long term care
*you can live your life but things will be different
*very hard, life trajectory changes
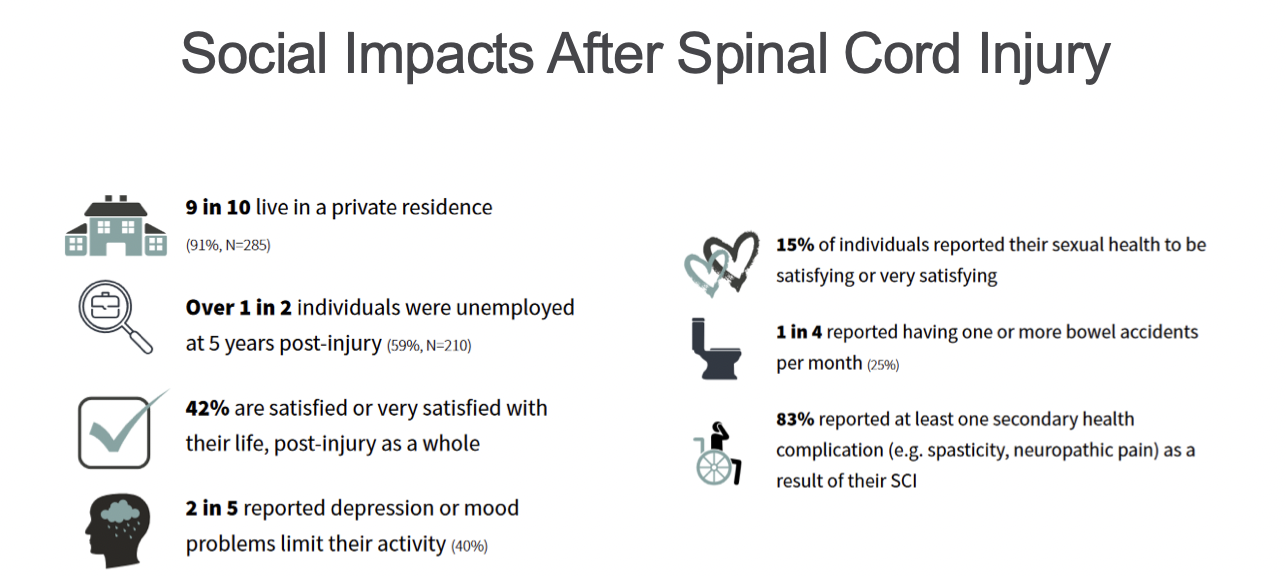
Secondary complications
-affect every system in the body
-entire body
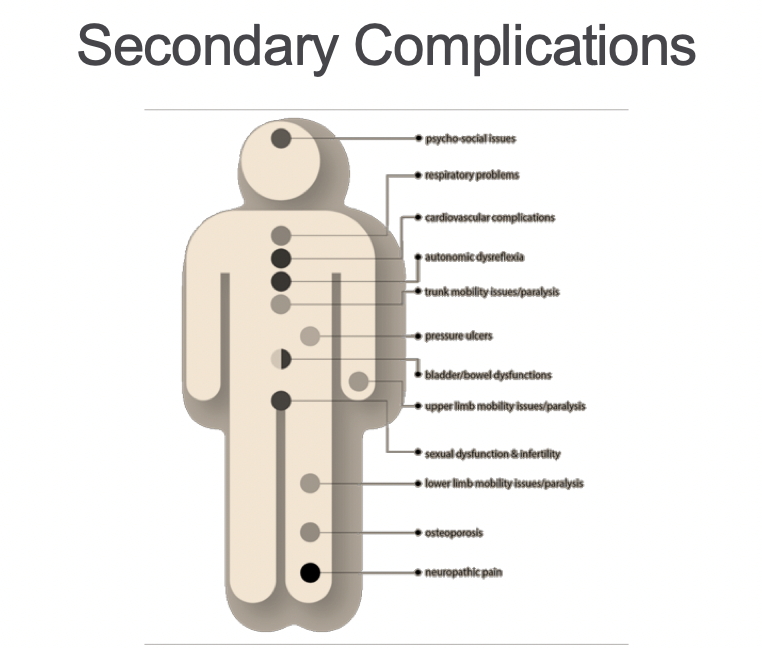
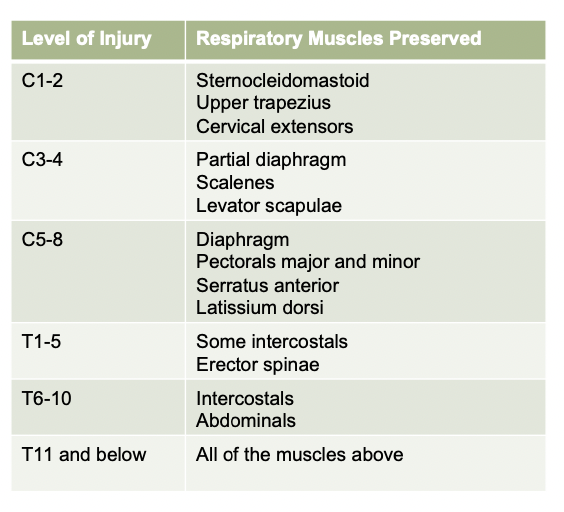
Respiratory impairment
c3, c4,c5- hard to cough,
• Respiratory function varies widely
• Respiratory problems are the leading cause of death in people with high cervical lesions
• People with injuries below T10 likely to have near-normal function bc resirratory muscles innervated
• Respiratory complications:
• Inspiration restricted
• Mucous clearance – lack of efficient cough
• Atelectasis-air sacs collapse of fail to inflate properly
• Pneumonia
can result in illness/death
Orthostatic hypotension
In individuals with an intact spinal cord, cardiovascular function is regulated by the brainstem and hypothalamus through the parasympathetic and sympathetic nervous systems
Parasympathetic input to the heart: Vagus nerve (CN X) = decrease heart rate
Sympathetic input to the heart: Spinal segments T1 to L2 through the sympathetic trunk which runs parallel to spinal cord = increase heart rate and peripheral vasoconstriction
SCI can result in loss of sympathetic communication between the brainstem and heart while parasympathetic input remains intact
Drop in BP when going from lying to sitting or standing (↓ of 20mmHg SBP and/or 10mmHg DBP)
S/S: dizziness, nausea, light headedness, visual changes (tunnel/spots)
More common with higher or complete injuries
*can be challenging and limit ppl from participating in rehab
-slowly lift them degree by degree with lift bed
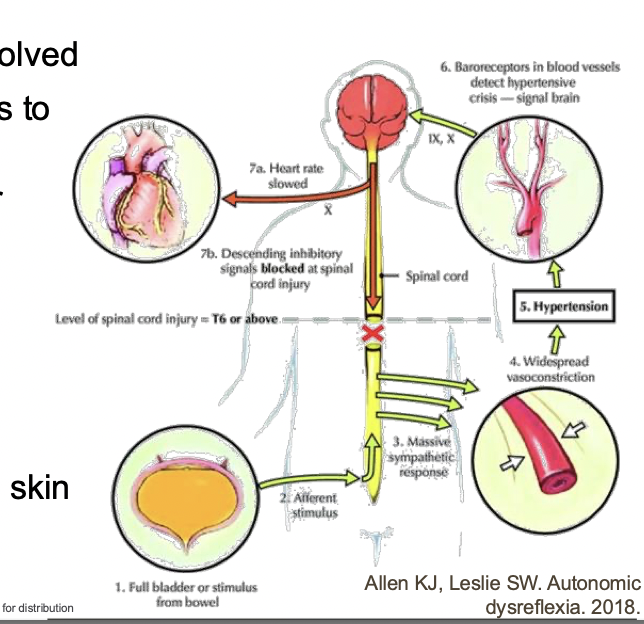
Autonomic dysreflexia
• Will not appear until spinal shock has resolved
• Imbalance in sympathetic discharge leads to mass autonomic reflex response
• SBP ↑ 25mmHg, (severe is ↑ 40mmHg or >150mmHg )
• Results from noxious stimulus below NLI • Only occurs in injuries at or above T6 (controls bp response)
• S/S: headache, anxiety, visual changes, nausea (feeling impeding doom)
• Above NLI: piloerection (goosebumps), sweating, flush skin
• Below NLI: pallor, cool skin- bc mass vasoconstriction
*could become noxious stim- goes into fight/flight mode e.g. pebble in the shoe or clothes twisted wrong way
brain cant interpret the full bladder sensation but peripheral nerves can still feel but the communication is not making it to the brain, send afferent stimu to brain saying smtg is wrong- when SC in tact we get that
-that signal isnt making it to brain- body saying hey smtg wrong idk though
-peripheral body will inc BP, but above the injury level it says why is my bp so high so it tries to bring it down
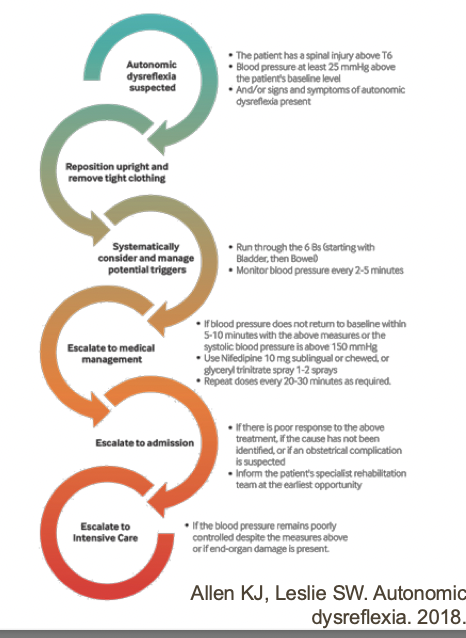
Management of autonomic dysreflexia
• Sit patient upright and remove compression
• Use OH to your advantage
• Check for and remove noxious stimulus
• Empty bladder, loosen clothing, etc
• If cannot remove stimulus/symptoms persist for >1hr- Medical Emergency!
• Can lead to stroke, coma, or death
*if we can remove nocious stim the whole thing goes away- loosen clothing, pee, if cant find for an 1 hour its ER bc now they need medication to regulate bp
Impaired temperature control
• After SCI the hypothalamus cannot control cutaneous blood flow
• Autonomic dysfunction results in loss of internal thermoregulatory responses
• Lose ability to shiver and sweat below the level of the lesion- esp if injury is in your neck
• Severity of impairment depends on level of lesion and whether injury is incomplete or complete
• Greatest concern in people with tetraplegia
• Initially after the injury – risk of hypothermia due to peripheral vasodilation
• Chronic injuries – risk of hyperthermia due to lack of sympathetic control of sweat glands
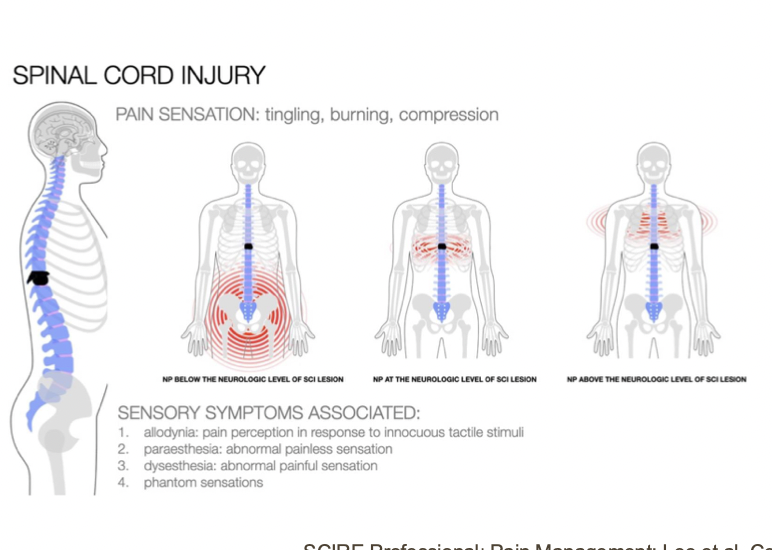
Noiceptive pain
• Musculoskeletal
• Visceral (stomach hurt)
• Other
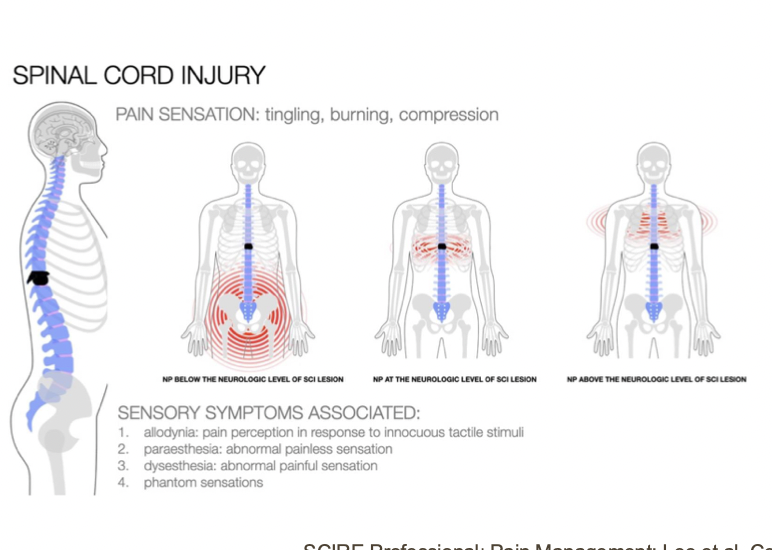
Neuropathic pain
• At level
• Above level
• Below level
Spasticity
Spasticity presents below the level of the lesion after spinal shock resolves
Managed through stretching and medications, including botulinum toxin injections
In extreme cases that aren’t managed with above then surgery
Dorsal rhizotomy – resection of posterior nerve roots to disrupt the stretch reflex
Pressure injuries
• Skin and tissue breakdown (usually overweight-bearing areas) which can lead to infection
• Caused by pressure, friction/shear forces, skin changes, loss of sensation, reduced mobility, weight changes, inappropriate surfaces
• Prevention is key
Sublesional osteoporosis
• Excessive bone resorption, reduced loading, and decreased muscle activity
• Increased risk of fragility fracture
• Risk factors: female sex, motor complete injury, chronicity, alcohol consumption, low weight • Can be treated with medications, electrical stimulation, weight-bearing activities, exercise
not moving muscles not pulling on bones so therefore not loading the bones
Bowel/bladder dysfunction
• Issues with storing and/or emptying very common because of neural control
-conus medullaris at L1-L2 below that is cauda equina
NLI above conus medullaris
→ spastic or reflex or upper motor neuron • Overactive bladder muscles and discoordination with sphincter
• Bowel reflexes are intact but no longer controlled
NLI below conus medularis
→ flaccid or non-reflex or lower motor neuron
• Underactive bladder muscles and external sphincter, internal sphincter often in spasm
-very loose, everyhing hard to constriction
• Loss of bowel reflexes and muscle tone
• Bladder: catheterization common (↑ risk of UTIs – very common secondary complication)- ppl do this themselves
• Bowel: scheduled program with suppositories, digital stimulation, or manual evacuation
Sexual dysfunction
Changes to sexual desire, sensation, arousal, and orgasm depending on individual
Multifactorial (B&B, self-image, mobility)
People with SCI can maintain healthy sex lives and relationships
Injuries at T10 and above typically lose the ability to become aroused from sexual thoughts (psychogenic) but are usually able to become aroused through touch (reflexic arousal)
Injuries from L3 to S1 may be able to experience both psychogenic and reflex arousal, although these responses may be poorly coordinated
Injuries from S2 to S4 typically lose the ability to experience reflex arousal but may be able to have psychogenic arousal
Fertility depends on ability to ejaculate and sperm quality for those with a penis, typically unchanged for those with a uterus
-bowel/bladder cant control you dont want to engage in this as much
Learning Objectives
Analyze the functional assessment of SCI
Learn about SCI rehabilitation practices
Level of involvement: International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI)
Level of involvement →
Neurological Level of Injury (NLI): most cephalad/rostral segment between right and left sensory and motor levels →
Sensory Level: most caudal segment with intact sensation bilaterally →
Motor Level: most caudal segment with anti-gravity strength bilaterally, so long as segments above have full strength
above t1- tetra
below t2- para
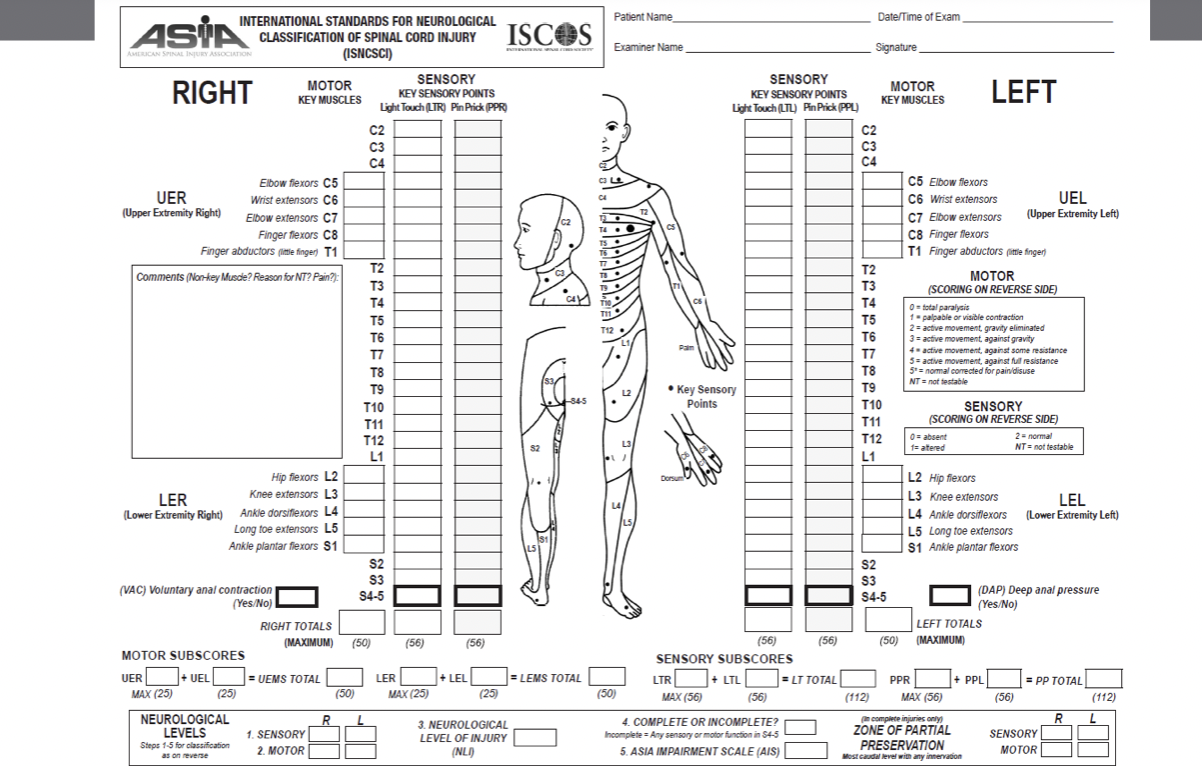
Level of severity: International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI)
Level of severity→
Complete
Sensory incomplete
Motor incomplete
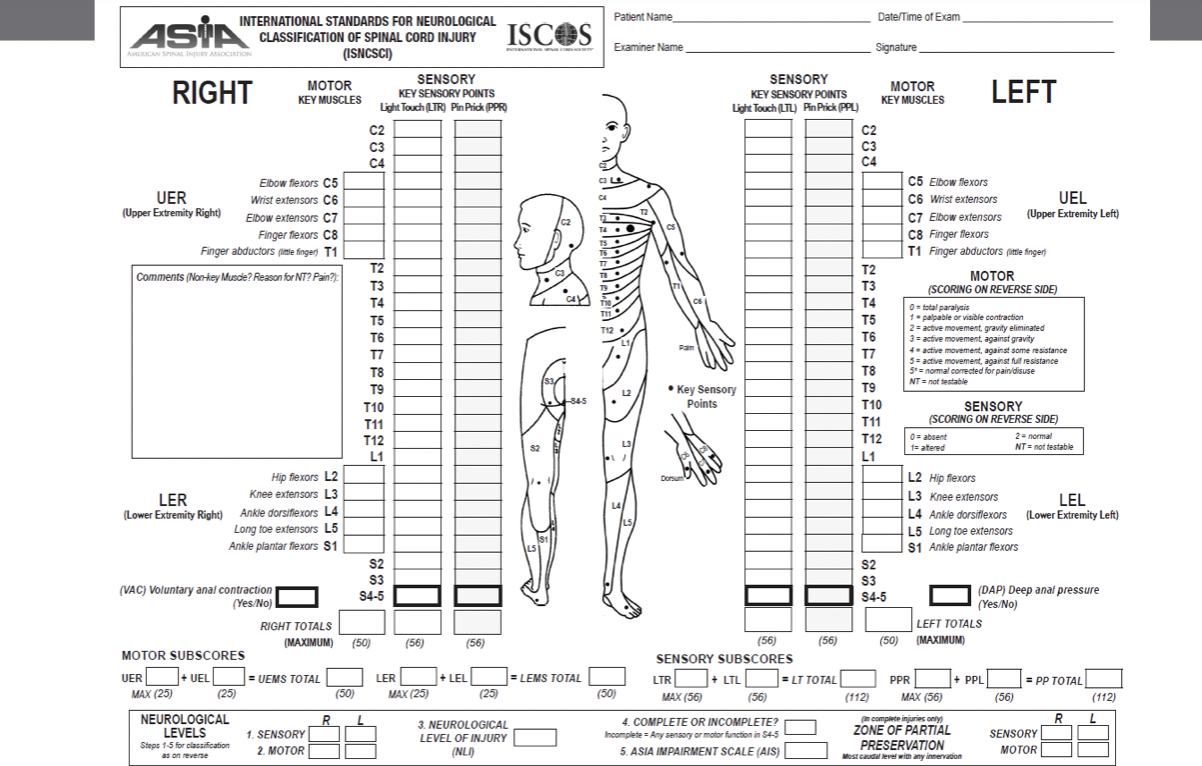
Sensory testing
• Test light touch & pin prick at ALL key dermatomes
• Tracts?
dorsal column (light touch) and another one?
• Grade with 3 point scale
• 0 = absent
• 1 = impaired (compared to face) -usually forehead and check and assumed to be in tact because cranial nerves
• 2 = normal
if has two across in both left and right will be the sensory level of injury
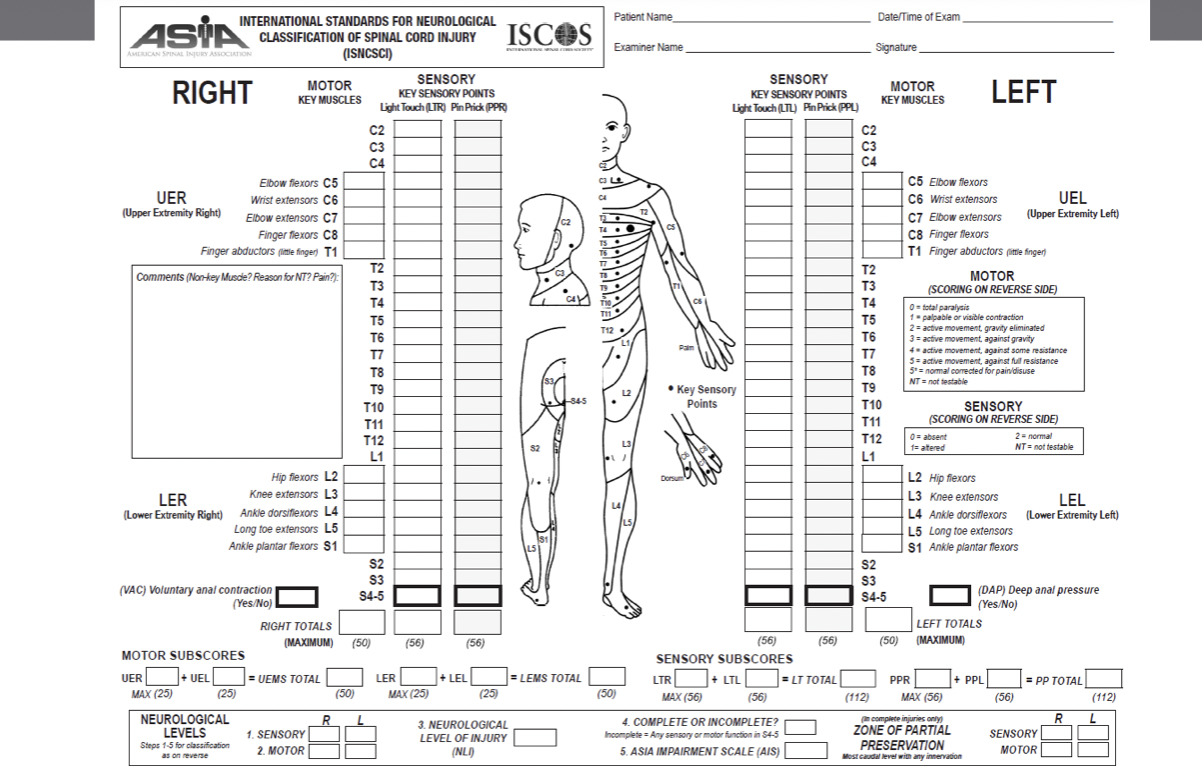
Motor testing
• Test strength of key muscles for each myotome
• Grading of muscle strength out of 5
• 0 = total paralysis- no muscle activity
• 1 = palpable or visible muscle contraction (flicker in muscle no active mvmt of joint- not strong enough)
• 2 = active movement, full ROM with gravity eliminated • 3 = active movement, full ROM against gravity
• 4 = active movement, full ROM against moderate resistance in a muscle specific position
• 5 = (normal) active movement, full ROM against full resistance in a muscle-specific position
expected from an otherwise unimpaired person
• Motor level = Score of 3/5 & next most rostral level has 5/5
if the level above is only a 4 then that will be the motor
dont score throacic spine
if you cant figure out motor usually say its the same as sensory levels
Sacral testing: Deep anal pressure (DAP)
is part of the sensory exam
• Examined through insertion of the examiner‘s index finger and application of gentle
pressure to the anorectal wall (S4/5)
• Graded as yes or no for consistent ability to feel pressure
• Tests for sensory incomplete injuries
-helps us determine if the injury is complete or incomplete
if they have sensation in lowest segments then
if they cant feel this, we think it is sensory complete injruy somewhere in that tract there is njo more sensory info
Sacral testing: Voluntary anal contraction (VAC)
is part of the motor exam
• External anal sphincter examined through voluntary contractions against inserted index finger (S2 – S4)
• Graded as yes or no (cannot be a reflex contraction)- has to be a voluntary contraction
• Tests for motor incomplete injuries if there is some info coming thru the spine- if they have stuff then its motor incompeltye
if no- motor compelte some point in track no more info getting through
Neurological level of injury
• Motor and sensory levels may be different
Right and left sides may also be different
NLI is the most caudal level with intact sensation and anti-gravity strength bilaterally, as long as the level above has intact sensation and full strength
• If the sensory level is at a segment not able to be tested for motor function (C1 – C4; T2 – L1; S2 – S5) than the motor level is presumed to be the same as the sensory level, given that rostral testable motor function is normal (higher)
-its not based off of where the damage is in SC its more -maybe got injured higher above- maybe because of swelling and stuff it could go below causing dmaage
-not based on tissue damage more based on the function
*8all of this was for level of impaiirment
American Spinal injury association (asia) Impairment scale (AIS)
NOW LEVEL OF SEVERITY
-grade compelteness of injury

A
complete
No sensory or motor function in lowest sacral segments (S4/5). No sacral sparing
when they did the anal tests- we know theres a block in the system someone
-does not mean there was not a full transection of cord it just means at some point theres no signal coming through
B
Sensory Incomplete
Sensory but no motor function preserved in the lowest sacral segments (sacral sparing) and no motor function > 3 segments below motor level bilaterally
-have dap but no for vac- more likely to see sensory come back before motor
-still can be some below level of lesion but for grade B we dont see anything more than 3 levels below because of redundancies in the system
sometimes called motor complete bc still intact
C
Motor incomplete
Motor function preserved in the lowest sacral segments or patient is sensory incomplete with motor function > 3 segments below motor level.
less than half of the muscles below NLI have strength against gravity
D
motor incomplete
Defined as motor incomplete, but at least half of the muscles below NLI have strength against gravity (grade 3, 4, or 5 strength)
E
normal
No changes in sensory or motor function
-all has resolved, but had temporary impairment
AIS scores
• Recovery is possible!
• First year is when the most changes occur
• Both motor and sensory improvements
• NLI may change
• ~25% of AIS A will become AIS B
• ~75% of AIS B will become AIS C
• ~75% of AIS C will become AIS D
• <25% of AIS D will become AIS E
Monroe and more axons can. grow and regenerate
Zone of partial preservation (ZPP)
Used only in injuries with absent sensory or motor function in lowest sacral segments (S4/5) either sensory or motor complete
• Write NA if not applicable
Refers to dermatomes or myotomes caudal to sensory and motor levels with partially preserved function (any score other than a 0)
• Most caudal level with any function recorded
• If none, sensory or motor level is recorded
practice 1
Motor Level = c6
Sensory Level =c6
NLI = c6
AIS Grade = we know its incomplete because they have both and motor and sensory
we have 16 muscles so magic number is 8 ace D
practice 2
Motor Level =T5
Sensory Level =t5- assume
NLI = T5
AIS Grade = A
ZPP present
Recovery Prognosis Following SCI
• Most changes occur during the first 6-9 months post-injury (1-year defined as chronic)
• Pinprick preservation closely linked to functional recovery – Why?
-highly likely to regain motor function, corticospinal tract very close to spinothalamic tract- they will gain one more motor level
• Pinprick preservation at NLI indicates motor recovery one level below
• Pinprick preservation increases chance for functional motor recovery at same level
• Sacral/lower extremity pinprick preservation significantly linked to ambulation ability at 1- year post-injury
• Neuropathic pain below NLI indicates motor recovery in incomplete injuries
-bc also transmitted by spinothalamic tract
Rehab goals
Recovery
• Restore neuromuscular system in order to regain pre-injury function
Compensation
• Use the body (unaffected muscles), assistive devices or technology to compensate to neuromuscular deficits in order to achieve function
Level of Spinal Cord Injury: C1-C4
• Innervated Muscles: Face and neck, cranial nerve, partial diaphragm (C3-4)
• Available Movements: Talking, chewing, sipping, blowing, scapular elevation (raise and shrug shoulders)
• Functional Capabilities: Head control wheelchair mobility or a blow straw, voice control electronics, directing care
• Equipment/Assistance Required: Requires full-time care and mechanical lift, potential need for ventilator
what they would still have available
Level of Spinal Cord Injury: C5
• Innervated Muscles: Shoulder muscles, biceps (flexion)
• Available Movements: Elbow flexion, shoulder external rotation, flexion,
abduction to shoulder height, forearm supination
• Functional Capabilities: Able to perform some basic self care (eating, grooming), participates in transfers, positioning, and manual wheelchair mobility-might choose not to because it takes a lot of energy, can use power wheelchair independently and drive with adaptive controls- joystick
• Equipment/Assistance Required: Uses adaptive equipment and requires assistance for set up, requires assistance for some self care (bowel/bladder)
Level of Spinal Cord Injury: C6
• Innervated Muscles: Scapular muscles, large shoulder muscles, some wrist extensors
• Available Movements: Shoulder and scapular movement, forearm pronation, wrist extension (creates tenodesis grip)- can grab things by extending their wrist because fingers automatically go into flexion for grip and grasp
• Functional Capabilities: Able to perform basic self care including upper body dressing, can use manual or power wheelchair, increased ability to transfer independently
• Equipment/Assistance Required: Uses adaptive equipment and may require assistance to set up, part-time care necessary
Level of Spinal Cord Injury: C7
• Innervated Muscles: Triceps, wrist muscles, some finger control
• Available Movements: Elbow extension, wrist flexion, finger extension
• Functional Capabilities: Independent with most self care, manual wheelchair,
• Equipment/Assistance Required: Assistance with heavy household tasks but may not require formal care
*usually completely independent
Level of Spinal Cord Injury: C8
• Innervated Muscles: All wrist and finger muscles
• Available Movements: Finger flexion
• Functional Capabilities: Independent with self care and manual wheelchair, may be able to transfer from floor to chair
• Equipment/Assistance Required: Some adaptive equipment
Level of Spinal Cord Injury: T1-T12
• Innervated Muscles: Rib cage, postural muscles, abdominals (T7 and below)
• Available Movements: Trunk control, improved breathing
• Functional Capabilities: Independent with self care and manual wheelchair, may be able to stand and ambulate with adaptive equipment (therapeutic)
• Equipment/Assistance Required: Hip-knee-ankle-foot orthoses, forearm crutches or walker
*use lat to lift pelvis and advance foreward and ambulate fwd
Level of Spinal Cord Injury: L1-L3
• Innervated Muscles: Back muscles, some hip control
• Available Movements: Hip flexion, adduction, knee extension
• Functional Capabilities: May be able to ambulate in home and short distances
• Equipment/Assistance Required: knee-ankle-foot orthoses, forearm crutches or walker
-ankles and glutes
Level of Spinal Cord Injury: L4-S1
• Innervated Muscles: Ankle and glute muscles
• Available Movements: Ankle dorsiflexion, toe movements (L5), ankle plantarflexion (S1)
• Functional Capabilities: Independent ambulation in community (may use wheelchair for long distances)
• Equipment/Assistance Required: May require ankle-foot orthoses, canes, 4- wheeled walker
Falls in SCI
78% of ambulatory people fall each year
of those 78%, 68% of these people are frequent fallers (>1 fall/year)
56% of wheelchair users fall each year (uneven surfaces and tip out of chair)
Causes of falls
BIOLOGICAL
-Muscle weakness/impaired balance
Behavioural
- Inattention/distraction
Social & Economic
- Variable fall prevention training Environmental
-Hazards or obstacles
Consequences of falls
Physical
Injuries
Hospital admissions
Secondary complications Psychosocial
Embarrassment
Fear of Falling
Decreased social participation
Neural Changes Impact on Motor Function
• Motor spinal circuits activated through extrinsic signals:
• Afferent input: Proprioceptive pathways
• Efferent input: Corticospinal tract
• Efferent input is limited below the lesion, meaning afferent signals become primary source of information
• Voluntary muscle control from the brain is reduced (i.e., muscles are driven by sensory input)
• Hyper-reflexia occurs (increased excitability to sensory input)
efferent info cant get down
afferent bc primary source for info below the level of the lesion
Central Pattern Generators (CPGs)
• Neural networks in the spinal cord
• Interneurons are activated to facilitate rhythmic motor outputs such as walking
• Relies on sensory input
• Role of muscle synergies
• Not adaptable without supraspinal input
• Bottom line: The spinal cord can generate a stepping pattern in absence of input from the brain with specific and appropriate sensory information
wont be able to do stairs or uneven surfaces
compelte sci they will step babies will do when born
-on treadmill thats moving body responds with what it thinks its supposed to do. an innate function of the SC
Neural Recovery in the Central Nervous System
McGill University (Purves et al. Neuroscience. 2001)
• Grey matter does not regenerate → focus for neural recovery is on the axons
• Need to regulate spinal circuit function and excitability following loss of efferent input
(Martin. Handbook of Clinical Neurology. 2022;184:317-30)
• Mechanisms: (Darian-Smith. Neuroscientist. 2009;15(2):149-65; Anjum et al. Int J Mol Sci. 2020;21(20):7533)
Reorganization: plasticity in the spared nerves (both spinal and supraspinal) • Repair: remyelination of axons- sometimes not completely dmaaged and jsut needs to be remyelinated
Regrowth: axonal regeneration or sprouting- severed axon start to regrow from severed end- not yet seen in humans
sprouting -neuron next door comes help has been seen in humans
vs regen is the fixing of the broken nneuron
CNS can recover, done in canada
grey matter does not regenerate so the focus becomes the axons
Spontaneous Neuroplasticity in the CNS
Cortical Motor Map Reorganization
• Motor areas in the brain representing impaired muscles shrink or are lost
(replaced by proximally adjacent functional muscles)
Corticospinal Tract Regrowth
• Animal models show axonal sprouting and even regeneration of CST axons
Spinal Circuit Repair, and Regrowth
• Changes in electrophysiology, remyelination, and axonal sprouting to form new spinal circuits and bypass lesion
Rehabilitation Facilitates Neuroplasticity
as physios try to give the right feedback back to sc and use motor imagery and think about the movement to strengthen those connections
-intatc systems on either sides and trgint. ostrengthen communications
Principles of Neuroplasticity

Elements of SCI Rehab
• OVERALL GOAL = maximize independence • Prevent secondary complications
• Stretching/range of motion
• Grip/grasp retraining
• Balance and falls prevention • Mobility
• Transfer training
• Wheelchair and seating • Wheelchair skills
• Gait retraining
Activity-Based Therapy
-activate muscles below the level of the lesion
-if someone wants to walk they need to practice walking (task specific stuff)
Locomotor Training
• Body-weight supported treadmill training, exoskeletons, overground walking
Principles
Maximize weight bearing
Optimize sensory cues
Optimize kinematics
Minimize compensation patterns
relay back to me giving the right sensory input
Central Excitability - Neuromodulation
• Spinal Cord Stimulation
• Activation at level of spinal circuitry
• Axon remyelination and sprouting, increased excitability
• Brain-Machine Interfaces
• Augment corticospinal tract activity
• Increase drive to paralyzed muscles or a prosthetic (robot over hand they will think open and it will open)
• Brain Stimulation
• Cortical excitability and corticospinal tract reorganization
• Restore supraspinal drive of motor output, axon regeneration and sprouting
electrical or magnetic stimulation