Pediatric Orthopedic Conditions: Fractures, Dysplasia, and Growth Disorders
1/126
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
127 Terms
What are the five fracture patterns of the Salter-Harris classification system?
Type I (Same), Type II (Above), Type III (Below), Type IV (Through), Type V (Crush)
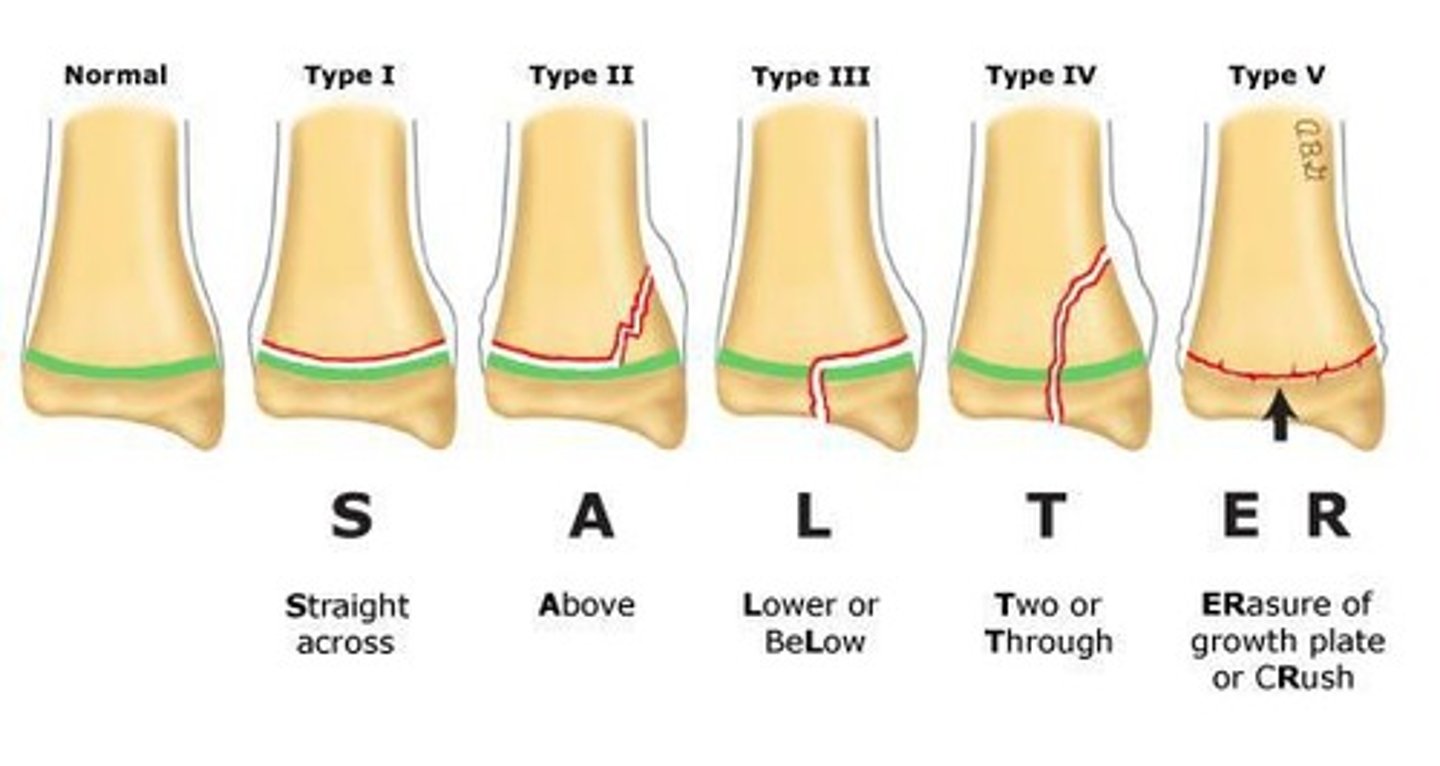
What is the significance of the Salter-Harris classification?
It classifies physeal injuries in skeletally immature individuals, with worse outcomes as the type number increases.
What is a common characteristic of pediatric bones?
Pediatric bones have lower cortical mineral content, allowing for greater plasticity and different fracture patterns.
At what age do girls typically stop growing?
Girls usually stop growing between 15 and 18 years old.
At what age do boys typically stop growing?
Boys usually stop growing between 18 and 21 years old.
What is the primary cause of apophysitis in pediatric patients?
Apophysitis is usually caused by inflammatory or stress injuries from repetitive overuse activities.
What are the common signs and symptoms of Osgood-Schlatter Disease?
Knee pain, tenderness at the anterior tibial tubercle, and swelling, especially during activity.
What is the most common age range for Little Leaguer Elbow?
The most common age range is 9 to 14 years old.
What are the signs of Little Leaguer Shoulder?
Signs include decreased ball control and velocity, pain related to activity, and tenderness at the proximal humeral physis.
What is the typical age range for Sever Disease?
Sever Disease commonly affects children aged 8 to 12 years.
What are the common symptoms of Sever Disease?
Symptoms include tenderness at the calcaneal physis and walking on toes.
What is the treatment approach for apophysitis?
Treatment typically includes rest, activity modification, NSAIDs, and physical therapy after 6 weeks.
What is the most common Salter-Harris fracture type?
Type II (Above) is the most common Salter-Harris fracture.
What is the prognosis for Type V Salter-Harris fractures?
Type V fractures have a high chance of growth disturbance.
What is the role of comparison x-rays in Salter-Harris fractures?
Comparison x-rays are ordered if there is concern about the fracture, to assess bilateral differences.
What is the primary cause of developmental dysplasia of the hip?
Developmental dysplasia of the hip is often due to abnormal hip joint formation during fetal development.
What are the common clinical findings for slipped capital femoral epiphysis?
Symptoms include hip pain, limited range of motion, and a limp.
What is the typical age range for Legg-Calve-Perthes disease?
Legg-Calve-Perthes disease most commonly affects children aged 4 to 8 years.
What is a Toddler Fracture?
A Toddler Fracture is a spiral fracture of the tibia commonly seen in young children, often due to a fall.
What is the primary concern with Type III Salter-Harris fractures?
Type III fractures involve the joint and require anatomic reduction due to potential joint involvement.
What is the significance of the metaphysis in bone anatomy?
The metaphysis is the region of bone that transitions between the epiphysis and diaphysis, important for growth.
What is the mechanism of injury (MOI) for a Toddler Fracture?
The child's body rotates around a fixed foot, often with minimal force in younger children (< 5 years) and extensive force in older children (> 5 years).
What are the physical exam findings for a Toddler Fracture?
Marked limp or refusal to walk, usually no swelling or deformity, tenderness to palpation or with twisting of the extremity, and full range of motion at the ankle, knee, and hip.
How can one differentiate unintentional from abusive trauma in toddlers?
90-95% of unintentional toddler fractures have a reported mechanism of injury, while spiral fractures are suspicious but not pathognomonic for abuse.
What imaging is used for diagnosing a Toddler Fracture?
Radiographs (AP and lateral views of the tibia/fibula) are used to identify faint hairline fractures or nondisplaced spiral fractures.
What is the treatment for a Toddler Fracture?
Immobilization with a cast for 4 weeks, along with NSAIDs and Tylenol for pain management.
What is Nursemaid Elbow?
Radial head subluxation that occurs when the annular ligament slips over the head of the radius and becomes trapped.
What is the common age range for Nursemaid Elbow?
Most commonly occurs in children aged 1 to 4 years.
What is the mechanism of injury (MOI) for Nursemaid Elbow?
Axial traction on a pronated forearm with the elbow in extension, often from swinging a child by the arms or sudden pulls.
What are the physical exam findings for Nursemaid Elbow?
Child shows no desire to move the arm, poorly localized pain, arm close to the body with forearm pronated, tenderness over the radial head/annular ligament, and full passive range of motion of the elbow and wrist without swelling or deformity.
Is imaging necessary for Nursemaid Elbow diagnosis?
No X-ray is needed; it is a clinical diagnosis.
What is the treatment for Nursemaid Elbow?
Reduction of the subluxation, with pain decreasing within 15-20 minutes and full active range of motion achieved without additional splinting or treatment.
What is the prognosis for Nursemaid Elbow?
Good prognosis with proper treatment and patient education.
What is Nursemaid's Elbow?
A common injury in young children where the radial head is subluxated, often treated using the Hyperpronation or Supination/Flexion techniques.
What are the techniques for reducing Nursemaid's Elbow?
1. Hyperpronation Technique: Support arm at elbow, apply pressure on radial head, grip distal forearm, and hyperpronate. 2. Supination/Flexion Technique: Support arm, apply pressure on radial head, pull gentle traction on distal forearm, then fully supinate and flex elbow.
What characterizes Slipped Capital Femoral Epiphysis (SCFE)?
Displacement of the femoral neck and shaft from the femoral epiphysis, with the neck moving anterior-superior relative to the epiphysis.
What is the male-to-female ratio for Slipped Capital Femoral Epiphysis?
2:1, with boys typically affected at age 13 and girls at age 12.
What are some associated conditions with Slipped Capital Femoral Epiphysis?
Obesity, periods of rapid growth, history of radiation therapy, endocrine abnormalities (like hypothyroidism), growth hormone deficiency, and genetic disorders.
What are the common symptoms of Slipped Capital Femoral Epiphysis?
Non-radiating dull ache, painful limp, Trendelenburg gait, leg externally rotated, and limited range of motion, especially in flexion, internal rotation, and abduction.
What imaging findings are indicative of Slipped Capital Femoral Epiphysis?
Radiographs show widening, lucency, irregularity of the physis, and blurring of the junction between metaphysis and physis, often described as 'ice cream slipping off a cone.'
What are the treatment options for Slipped Capital Femoral Epiphysis?
Non-weightbearing and operative stabilization, with potential complications including osteonecrosis of the femoral head and degenerative arthritis.
What is Legg-Calve-Perthes Disease?
Avascular necrosis of the femoral head without a known etiology, usually unilateral, most common in children aged 4-10.
What are the risk factors for Legg-Calve-Perthes Disease?
Family history, low birth weight, coagulation abnormalities, and secondhand smoke exposure.
What are the early and late physical exam findings for Legg-Calve-Perthes Disease?
Early: painless limp, pain related to activity, increased density of the femoral epiphysis. Late: Trendelenburg gait, restricted range of motion, positive crescent sign.
What are the treatment options for Legg-Calve-Perthes Disease?
Operative and nonoperative treatments, including activity restriction, physical therapy, and in some cases, femoral or pelvic osteotomy.
What is Developmental Dysplasia of the Hip?
A spectrum of conditions involving acetabulum and/or femoral head abnormalities, often influenced by forces applied in utero.
What are the risk factors for Developmental Dysplasia of the Hip?
Breech presentation, large gestational weight, female gender, family history, firstborn status, and inappropriate swaddling.
What are the key physical exam maneuvers for assessing Developmental Dysplasia of the Hip?
Barlow maneuver (dislocates a dislocatable hip) and Ortolani maneuver (reduces a dislocated hip).
What is the Galeazzi sign in the context of hip dislocation?
An apparent limb length discrepancy due to unilateral hip dislocation, assessed by flexing hips and knees at 90°.
What imaging techniques are used for Developmental Dysplasia of the Hip?
Ultrasound for infants under 6 months and radiographs for those over 6 months.
What is the success rate of the Pavlik Harness in treating Developmental Dysplasia of the Hip?
85-95% success rate when used for infants under 6 months with a reducible hip.
What are the indications for surgical treatment in Developmental Dysplasia of the Hip?
Open reduction and casting, or osteotomies for children older than 6 months or those with irreducible hips.
What are the two techniques for reducing Nursemaid Elbow?
1. Hyperpronation Technique: Support arm at elbow, apply pressure on radial head, grip distal forearm, and hyperpronate. 2. Supination/Flexion Technique: Support arm, apply pressure on radial head, pull traction on distal forearm, and fully supinate and flex elbow.
What is Slipped Capital Femoral Epiphysis (SCFE)?
A condition characterized by the displacement of the femoral neck and shaft from the femoral epiphysis, more common in boys aged 13 and girls aged 12.
What are the common risk factors associated with SCFE?
Obesity, periods of rapid growth, history of radiation therapy, endocrine abnormalities like hypothyroidism, and genetic disorders.
What are the typical symptoms of SCFE?
Non-radiating dull ache, painful limp, Trendelenburg gait, leg externally rotated, and limited range of motion.
What imaging techniques are used to diagnose SCFE?
Radiographs (AP and frog leg view) showing widening, lucency, and irregularity of the physis.
What is the treatment for SCFE?
Non-weightbearing and operative stabilization.
What complications can arise from SCFE?
Osteonecrosis of the femoral head, femoral acetabular impingement, contralateral hip SCFE, and degenerative arthritis.
What is Developmental Dysplasia of the Hip (DDH)?
A spectrum of abnormalities in the acetabulum and/or femoral head stability, often related to forces applied in utero.
What are the key physical exam maneuvers for diagnosing DDH in newborns?
Barlow maneuver (dislocates a dislocatable hip) and Ortolani maneuver (reduces a dislocated hip).
What imaging is recommended for DDH in infants?
Ultrasound for infants under 6 months and radiographs for those over 6 months.
What is the most reliable sign of DDH in children aged 3 months to 1 year?
Limitation of hip abduction.
What is the treatment for DDH in infants under 6 months?
Pavlik Harness, which has an 85-95% success rate.
What are the treatment options for DDH in children older than 6 months?
Closed reduction and spica casting or surgical options like open reduction and osteotomies.
What is the prognosis for successfully treated DDH?
Generally better than SCFE and Perthes due to early detection and treatment.
What is the Salter-Harris classification used for?
It classifies physeal injuries in skeletally immature individuals, describing fractures through the physis.
What are the five types of Salter-Harris fractures?
Type I: Same (through physis), Type II: Above (through physis and metaphysis), Type III: Below (through physis and exiting epiphysis), Type IV: Through (through physis, epiphysis, and metaphysis), Type V: Crush (injury to physis).
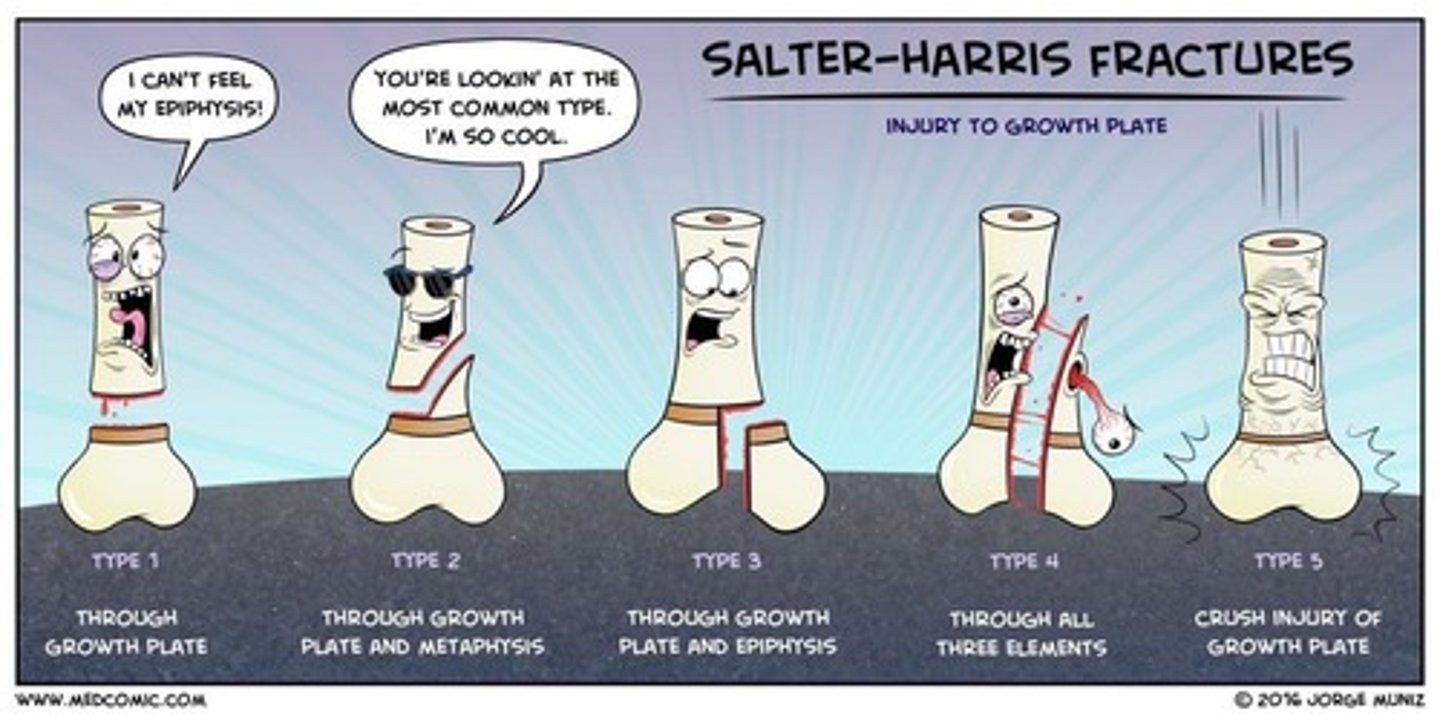
What characterizes a Type I Salter-Harris fracture?
It is an isolated growth plate fracture with a low chance of growth disturbance.
What is a common outcome of a Type II Salter-Harris fracture?
It may lead to variable growth disturbance as it involves the metaphysis.
What is the significance of a Type III Salter-Harris fracture?
It involves the joint and requires anatomical reduction due to potential growth disturbance.
What is a Type V Salter-Harris fracture?
It is a rare crush injury to the physis with a high chance of growth disturbance.
What is apophysitis?
An inflammatory or stress injury around the physis due to repetitive overuse activities.
What are common conditions associated with apophysitis?
Little Leaguer Shoulder, Little Leaguer Elbow, Osgood-Schlatter Disease, Sinding-Larsen-Johansson Disease, and Sever Disease.
What are the signs and symptoms of Osgood-Schlatter Disease?
Knee pain, tenderness, and swelling at the anterior tibial tubercle, worsened by activity.
What is Sever Disease?
An apophysitis of the calcaneal physis, common in gymnasts, characterized by heel pain and tenderness.
What is the typical treatment for Nursemaid's Elbow?
Reduction of the subluxation, often with no need for splinting or further treatment.
What are the risk factors for SCFE?
Obesity, periods of rapid growth, history of radiation therapy, and endocrine abnormalities.
What are the imaging findings for SCFE?
Widening, lucency, and irregularity of the physis, often described as 'ice cream slipping off a cone.'
What are the signs and symptoms of Legg-Calve-Perthes Disease?
Painless limp, activity-related pain, and restricted range of motion, particularly in internal rotation and abduction.
What is the primary treatment for developmental dysplasia of the hip (DDH)?
Nonoperative treatment with a Pavlik harness for infants under 6 months, or operative treatment for older children.
What are the key physical exam findings for DDH in newborns?
Positive Barlow and Ortolani tests, limb length discrepancy, and asymmetry of skin folds.
What is the significance of the Galeazzi test?
It assesses for leg length discrepancy due to unilateral hip dislocation.
What is the recommended imaging for DDH in infants under 6 months?
Ultrasound, as the acetabulum and femoral head do not appear on radiographs until 4-6 months.
What are common signs of apophysitis in young athletes?
Pain during activity, tenderness at the affected site, and swelling.
What is the typical age range for Little Leaguer Elbow?
Most common in children aged 9-14 years.
What is the common treatment for apophysitis?
Rest, activity modification, NSAIDs, and physical therapy after a period of rest.
What is the prognosis for children with successfully treated DDH?
Better prognosis compared to SCFE and Perthes due to early detection and treatment.
What mechanism of injury (MOI) typically causes a Toddler Fracture?
The child's body rotates around a fixed foot, often with minimal force in younger children and extensive force in older children.
What imaging is used to diagnose a Toddler Fracture?
Radiographs (AP and lateral views of the tibia and fibula) to identify faint hairline or nondisplaced spiral fractures.
What is the common mechanism of injury for Nursemaid Elbow?
Axial traction on a pronated forearm with elbow extension, often from swinging children by their arms or sudden pulls.
How is Nursemaid Elbow diagnosed?
It is a clinical diagnosis and does not require X-ray imaging.
What are the risk factors associated with Slipped Capital Femoral Epiphysis?
Obesity, periods of rapid growth, history of radiation therapy, and endocrine abnormalities like hypothyroidism.
What are the physical exam findings for SCFE?
Non-radiating dull ache, painful limp, Trendelenburg gait, leg externally rotated, and limited range of motion.
What imaging is used to diagnose SCFE?
Radiographs (AP and frog leg view) showing widening, lucency, and irregularity of the physis.
What are the early physical exam findings for Legg-Calve-Perthes Disease?
Painless limp, pain related to activity, and increased density of the femoral epiphysis on imaging.
What is the treatment for Legg-Calve-Perthes Disease?
Operative or nonoperative management depending on age and degree of hip abduction, including activity restriction and physical therapy.
What are the physical exam techniques used to assess for DDH in infants?
Barlow and Ortolani maneuvers to detect dislocatable or dislocated hips.
What imaging is used for diagnosing DDH?
Ultrasound for infants under 6 months and radiographs for those over 6 months.
What is the treatment for Developmental Dysplasia of the Hip?
Nonoperative treatment with a Pavlik harness for infants under 6 months or surgical intervention for older children.