Unit 2 - Pediatric Examination, Perinatal Diagnoses, Cardiopulmonary Conditions and Fitness
1/149
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
150 Terms
International Classification of Functioning, Disability, and Health
Health Condition Ex
Down Syndrome
International Classification of Functioning, Disability, and Health
Impairments Ex
Hypotonia
Ligamentous laxity
Muscle weakness
Poor endurance
International Classification of Functioning, Disability, and Health
Activity Limitations Ex
Pulling to stand
Cruising
Walking
International Classification of Functioning, Disability, and Health
Participation Restrictions Ex
Interacting with siblings
Playing with toys on sofa
International Classification of Functioning, Disability, and Health
Environmental Factors Ex
Home environment
Access to siblings for play
International Classification of Functioning, Disability, and Health
Personal Factors Ex
Family support
Other medical comorbidities
Examination: History
Obtained via interview with child and family and review of medical records
The child’s past and current health status
PT to identify:
Child and family strengths
Resources
Expectations
Desired outcomes of PT
Review of systems
Examination: Systems Review
Cardiovascular and pulmonary
Integumentary
Musculoskeletal
Neuromuscular
Communication ability, affect, cognition, language, ability to read, and learning style
Movement
Movement Analysis of Tasks

Examination: Tests and Measures
Aerobic Capacity/Endurance
Anthropometric Characteristics
Adaptive and Assistive Technology
Balance
Circulation (Arterial, Venous, Lymphatic)
Cognitive and Mental Function
Community, Social, and Civic Life
Cranial and Peripheral Nerve Integrity
Education Life
Environmental Factors
Gait
Integumentary Integrity
Joint Integrity and Mobility
Mobility (e.g., Locomotion)
Motor Function
Muscle Performance (Strength, Power, Endurance, and Length)
Neuromotor Development and Sensory Processing
Pain
Posture
Range of Motion
Reflex Integrity
Self-Care and Domestic Life
Sensory Integrity
Skeletal Integrity
Ventilation and Respiration
Work/Community Integration
Pediatric Pain Scale
The FLACC Scale
Face, legs, activity, cry, and consolability
For children who are pre-verbal or non-verbal
Pediatric Pain Scale
The Wong-Baker Faces Rating Scale or Visual Analog Scale (VAS)
For children who can verbalize type and/or level of pain

Evaluation Leads to Diagnosis/Prognosis/ Plan of Care
Diagnosis
Identify the impact of a condition on function at the level of the movement system and the whole person
Example: Force Production Deficit and Movement Pattern Coordination Deficit
Evaluation Leads to Diagnosis/Prognosis/ Plan of Care
Prognosis
In the likelihood that a child or youth will achieve the desired goals of intervention
Optimal level of improvement in function
Amount of time needed to reach that level
SMART Goals
Short Term Goals (4 weeks)
Long Term Goals (8 weeks)
Patient Client Management
Evaluation process identifies:
Body function and structure impairments
Activity limitations
Participation restrictions
Physical Therapy Goals
ICF model
Activity
Participation
Physical Therapy Goals
SMART-F Goals
Specific
Measurable
Achievable
Relevant
Time-bound
Short term goals (3 months)
Long term goals (6 months)
Function
Chronological Age
The age of a child from actual birth
what a parent will answer when you ask "How old is your child?"
Gestational Age
Age of a pregnancy started at the woman's last menstrual period
Also described as the amount of time that a baby has been in mom's belly ("The child was born at 32 weeks GA")
Adjusted or Corrected Age
The chronological age reduced by the number of weeks the child was born before 40 weeks gestation
For example, a 3-month-old baby who was born 1 month early would have an "adjusted" aged of 2-months-old.
allow adjustment up tp 2 years old
What are single task outcome measures?
Assesses one domain
Features:
Standardized
Psychometrically sound
Predictive, discriminatory, or useful for showing change in motor performance or functional mobility
Takes less time to administer than multi-domain measures
Single task outcome measures
TUG
stands and walks 3 meters, and then turns and walks 3 meters back and sits back in the chair
or 10 feet
Single task outcome measures
TUDS
child walks up and down 14 stairs
The participants are allowed to choose any method of traversing the stairs. This includes using a "step to" or "foot over foot" pattern, running up the stairs, skipping steps, or any other variation
Handrails can be available
The participants wear shoes, but no orthotics
Single task outcome measures
30 Second Walk Test
will tell us more about walking speed and when physical disability restricts the time or distance that a child can walk
Single task outcome measures
6 Minute Walk Test (6MWT)
could be used for a child with cystic fibrosis to monitor their endurance and gain insight into how their pulmonary status impacts their functional mobility
Single task outcome measures
5 x Sit-to-Stand (5xSTS)
just like the adult test, but with a chair that allows the child to start at a 90/90 position
Single task outcome measures
Timed Floor to Stand - Natural
requires the child to stand up from the floor, walk 3 meters, and then come back to sit on the floor again with their legs crossed
related to skills children may need to do daily at school or home
Single task outcome measures
Pediatric Balance Scale
very reminiscent of the Berg Balance Scale for adults and allows us to examine functional balance in the pediatric population
A PT would like to assess a kindergartener’s physical ability to participate in his school’s circle time (floor) with his peers. Which outcome measure would be most appropriate?
Timed Floor-to-stand — natural
A 12-year-old adolescent who underwent a heart transplant one year ago would like to go on a field trip to a science center with his classmates. Although there will be intermittent rest breaks, the adolescent will be expected to walk substantial distances. The PT is unsure if the child has the endurance. Which outcome measure would be most appropriate?
6 MWT
A school-based physical therapist is completing her beginning of year assessment for a child with mild cerebral palsy. The therapist takes note that the child has two classes on the second floor of the school. Which outcome measure would be most appropriate to determine if the child will need an elevator pass to get to class on time?
TUDS
A physical therapist would like to assess static and dynamic sitting and standing balance for an 8-year-old who sustained a brain injury two weeks ago. Which outcome measure would be the most appropriate?
Pediatric balance scale
A physical therapist would like to assess a 6-year-old child with Down Syndrome’s self-paced walking speed. Which outcome measure would be the most appropriate?
30 second walk test
Why are multi-item standardized outcome measures important in pediatrics?
Standardized application and scoring
Provides accurate and reliable data
Used for decision-making regarding:
Justification for services
Intervention
Goals
Plan of Care
Monitor progress
quite involved and can take anywhere from 15 to 60 minutes to administer
Multi-item standardized outcome measures
Selection based on ICF
Segmental Assessment of Trunk Control (SATCO)
Body Function & Structure
assesses postural control
Multi-item standardized outcome measures
Selection based on ICF
BOT-2/BOT-3
Body Function & Structure
Activity
measures strength and coordination
assesses mobility tasks such as running and jumping
Multi-item standardized outcome measures
Selection based on ICF
School function assessment (SFA)
Participation
assesses how a child experiences and performs in the school setting
Multi-item standardized outcome measures
Selection based on ICF
Activity
GMFM-66 and –88
PDMS-2/PDMS-3
TIMP
BOT-2/BOT-3
Multi-item standardized outcome measures
Selection based on Scoring and Interpretation
Criterion-referenced
Evaluate a child's performance on a specific set of skills
You complete the outcome measure with the child, and they get a score
There is no comparison of that score to any one other than that child you evaluated
Multi-item standardized outcome measures
Selection based on Scoring and Interpretation
Norm-referenced
Compare children to the child's same-aged peers
can make the determination of the child you are seeing is performing at, above, or below average because researchers have tested hundreds of typically developing children to make that data set
Multi-item standardized outcome measures
Selection based on Age and Diagnosis
For what age is the outcome measure validated?
Is there a diagnosis/condition/functional level associated with the measure?
For example
the GMFM is appropriate for children between 5 months old and 16 years old
The Alberta Infant Motor Scale is appropriate for children between 0 and 18 months old
Multi-item standardized outcome measures
Selection based on Technology / Equipment / Feasibility / Cost
Does the outcome measure require
a computer program?
special equipment?
How long does the outcome measure take to administer?
Can the child fully participate during the assessment?
What is the cost associated with the outcome measure?
Does the setting have requirements for certain outcome measures?
*Is the test reliable and valid?
Multi-item standardized outcome measures
Test of Infant Motor Performance (TIMP)
Alberta Infant Motor Scale (AIMS)
Peabody Developmental Motor Scales (PDMS)
Bruininks-Oseretsky Test of Motor Performance (BOT)
Gross Motor Function Measure (GMFM)
Pediatric Evaluation of Disability Inventory (PEDI)
School Function Assessment (SFA)
Segmental Assessment of Trunk Control (SATCO)
Multi-item standardized outcome measures
Important Information to Know
Age Range
Construct(s)
ICF domain
Norm or Criterion Referenced
Special populations or general?
Other unique factors
Multi-item standardized outcome measures
Norm-referenced
BOT
AIMS
PDMS
PEDI
Multi-item standardized outcome measures
Criterion referenced
TIMP
Multi-item standardized outcome measures
Both norm-referenced and criterion referenced
SFA
GMFM
SATCO
AIMS age range
0-18 months
PDMS age range
0-60 months
BOT age range
4-21 years
PEDI age range
6 months - 7.5 years
GMFM age range
5 months - 16 years
SFA age range
kindergarten - 6th grade
TIMP age range
34 weeks GA - 4 months
Brachial Plexus Injury (BPI)
Etiology and Incidence
Injury to the brachial plexus complex during a difficult vaginal delivery
Most frequent cause is shoulder dystocia or a unilateral traction injury to the brachial plexus
Incidence ranges from 0.38 to 4.6 per 1000 based on regional obstetrical care and mean birth weight
Brachial Plexus Injury (BPI)
Risk Factors
Shoulder dystocia
birth weight >90th percentile (4500–5000 g)
Maternal gestational diabetes
Prolonged maternal labor
Labor induction
Mechanical assistance (forceps, vacuum)
Breech delivery
Previous delivery of an infant with BPI
Brachial Plexus Injury (BPI)
Pathophysiology
Injury can occur anywhere between the spinal nerves to the peripheral nerves
Type of injury can vary from complete rupture to partial rupture
May require surgical repair
Regrowth 1 mm/day so up to 4-9 months depending on location
Recovery can continue up to 2-4 years depending on location
Approx. 65% of infants recover
Brachial Plexus Injury (BPI)
Injury Classification and Motor Impairments
Erb’s Palsy
Most common classification at 52%
Injury to C5 and C6 nerve roots (sometimes C7)
Shoulder held in extension, IR and ADD, elbow extension, forearm pronation, hand and finger flexion
Referred to as a “waiter’s tip position”
Brachial Plexus Injury (BPI)
Injury Classification and Motor Impairments
Klumpke’s Palsy
Rare
Involvement of the lower roots or spinal nerves of C8-T1
Forearm in supination and elbow flexion, paralysis of wrist flexors and extensors, and intrinsic muscles of the hand
Horner’s Syndrome
results from a T1 root abortion or an injury to the sympathetic ganglion, which can cause deficient sweating, the recession of the eyeball, abnormal pupillary response, miosis ptosis, and the irises of different colors
Brachial Plexus Injury (BPI)
Injury Classification and Motor Impairments
Global Palsy
Combination of injury to the upper and lower plexus C5 –T1
Total arm paralysis and loss of sensation
Approximately 13% of children
Can present with a milder form of Horner’s syndrome
Brachial Plexus Injury (BPI)
Clinical Presentation
Impairments
Torticollis and/or plagiocephaly
Muscle substitutions based on strength of available innervated muscles
Presents unilaterally
Neglect of upper extremity
Soft tissue contractures
Abnormal bone growth
Sensation changes can cause injuries
Brachial Plexus Injury (BPI)
Clinical Presentation
Activity and Participation
Varies based on injury, recover, and residual impairments
Asymmetrical developmental milestones
Creeping
Reach and grasp skills
Bilateral UE tasks: catching a large ball or lifting objects, and ADLs
Brachial Plexus Injury (BPI)
Medical Management
Diagnostic Testing
MRI
EMG
CT
CT-myelogram
Diagnostic ultrasound
Brachial Plexus Injury (BPI)
Medical Management
Surgical Intervention
Infants without full recovery by 1 month should be referred to specialty clinic
Neurosurgery
Primary nerve repair or reconstruction
Age 3 to 9 months typically recommended
<3 months if complete paralysis and/or with Horner’s syndrome
Post-op: immobilization for 3 weeks and then PROM/AROM
Orthopedic Surgery may also be warranted
Botox of antagonists
Brachial Plexus Injury (BPI)
PT Examination
History/Interview
History of birth and complications
Results of MRI and/or EMG
Parent understanding/perception of diagnosis
Brachial Plexus Injury (BPI)
PT Examination
Physical Examination
PROM & Strength/Motor Function – cervical and UE
Posture
Pain – FLACC scale
Sensation
Tone
Developmental positions
Gross motor skills – symmetry, age-appropriate
Brachial Plexus Injury (BPI)
Outcome Measures
Active Movement Scale: infants <1 yo
Modified Mallet Scale: 3-4+ yo
Test of Infant Motor Performance (TIMP): <4 months old
Alberta Infant Motor Scale (AIMS): 0-18 months
Brachial Plexus Outcome Measure: 4-19 yo
Brachial Plexus Outcome Measure Activity Scale: 4-19 yo
Assisting Hand Assessment: 18 mo-12 yo
Mini-Assisting Hand Assessment: 8-18 months
Brachial Plexus Injury (BPI)
PT Intervention
Instruct family on ROM
Gentle stretching
Stabilize scapula manually during ROM and reaching
Positioning guidelines to prevent contracture and to emphasize function
Facilitate normal movement patterns
Immobilize unaffected arm – CIMT
Kinesiotaping
Electrical Stimulation and Biofeedback – older children
Utilize tactile stimulation
Joint compression
Splinting
Gross motor skills and transitions
Brachial Plexus Injury (BPI)
Rehab Goals
Increase PROM
Increase strength
Increase sensation
Decrease pain
Prevent contractures
Facilitate symmetrical gross motor development
Decreased activity limitations or participation restrictions
What is Developmental Delay?
When a child does not achieve their developmental milestones compared to their age-matched peers
Mild
Moderate
Severe
What is Developmental Delay?
Significant delay
performance is two or more standard deviations below the mean on standardized norm-referenced testing
Common Etiologies of Developmental Delay
Prenatal
Genetic disorders: Down syndrome, Fragile X syndrome, chromosomal microdeletion or duplication
Cerebral dysgenesis: microcephaly, absent corpus callosum, hydrocephalus, neuronal migration disorder
Vascular: occlusion, hemorrhage
Drugs: cytotoxic, anti-epileptic
Toxins: alcohol, smoking
Early maternal infections: rubella, cytomegalovirus, toxoplasmosis
Late maternal infection: varicella, malaria, HIV
Common Etiologies of Developmental Delay
Perinatal
Prematurity, intrauterine growth retardation, intraventricular hemorrhage, periventricular leukomalacia
Perinatal asphyxia: hypoxic-ischemic encephalopathy
Metabolic: symptomatic hypoglycemia, bilirubin- induced neurological dysfunction
Common Etiologies of Developmental Delay
Postnatal
Infections: meningitis, encephalitis
Metabolic: hypernatremia, hyponatremia, hypoglycemia, dehydration
Anoxia: suffocation, near-drowning, seizure
Trauma: head injury, either accidental or non-accidental
Vascular: strok
Common Etiologies of Developmental Delay
Others
Social: severe understimulation, maltreatment, malnutrition
Maternal mental health disorder
Unknown
Domains of Development
Physical
Social-Emotional
Language
Cognitive
Domains of Development
Physical
gross motor and fine motor
Types of Developmental Delay
Isolated
Global
Types of Developmental Delay
Isolated
a single domain
Types of Developmental Delay
Global
two or more developmental domains affecting children under the age of five years old
Where does physical therapy come in?
Early Identification!
Early Intervention!
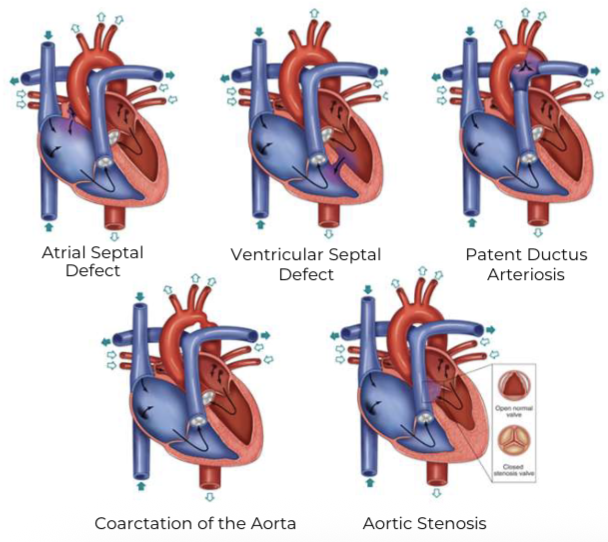
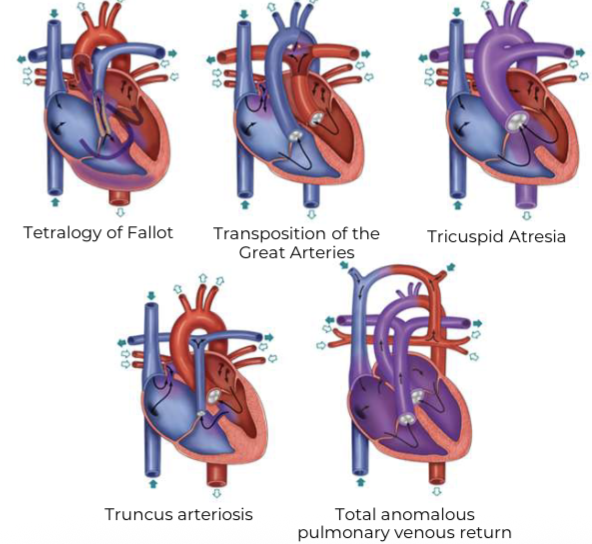
Congenital Heart Defects (CHD)
The most common birth defect
Occurring in ~1% of births each year
Often require physical therapy
Understanding the difference between acyanotic and cyanotic heart defects
Acyanotic Congenital Heart Defects
Definition
Impact the normal flow of blood through the body, including left-to-right shunting of blood through the heart and outflow obstructions.
Acyanotic Congenital Heart Defects
Types
Atrioventricular Septal Defect
Pulmonary Stenosis
Key Considerations for Children with Acyanotic Congenital Heart Defects
Tummy time may be limited and sternal precautions may vary
Promote safety with physical activity
At risk for executive functioning impairments
Follow up with cardiologist for exercise prescription
Pre-operative PT: optimize neuromotor development and endurance
Post-operative PT: upright positioning to maximize pulmonary function, airway clearance, and developmental handling with sternal precautions
Caregiver education and family-centered care
Cyanotic Congenital Heart Defects
Definition
Defects that allow the mixing of oxygenated and non-oxygenated blood
Cyanotic Congenital Heart Defects
Types
Pulmonary Atresia
Hypoplastic Left Heart Syndrome
Key Considerations for Children with Cyanotic Congenital Heart Defects
Critical CHDs result in cyanotic presentations
Tummy time may be limited and sternal precautions may vary
At risk for executive functioning impairments
More physical activity limitations compared to acyanotic peers
Activity considerations for patients with single ventricles
Inspiratory muscle training after Fontan procedure
Cardiac rehab is shown to be safe and beneficial
Pre-operative PT
Post-operative PT
Caregiver education and family-centered care
Physical Fitness Is…
Multidimensional
Health related fitness
includes daily function and health maintenance
Components include:
Cardiorespiratory endurance
Muscular strength and endurance
Flexibility
Body composition
Motor fitness
includes physical abilities related to:
Athletic performance
Agility
Coordination
Fitness Components
Cardiorespiratory endurance
improves their physical working capacity
reduces fatigue
reduces their risk of coronary heart disease
optimizes their growth and development
Fitness Components
Muscular strength and endurance
improves their functional capacity for lifting and carrying
reduces the risk of low back pain
optimizes their posture
optimizes their growth and development
Fitness Components
Flexibility
enhances their functional capacity for bending and twisting
reducing the risk of low back pain
optimizing their growth and development
Fitness Components
Body composition
reduces the risk of hypertension
reduces the risk of coronary heart disease
reduces the risk of diabetes
optimizes their growth and development
Fitness Testing
FITNESSGRAM
Is a National youth fitness test used throughout the United States
Uses criterion-referenced standards that reflect levels of fitness important for good health
Fitness Testing
Brockport Physical Fitness Test
Health related criterion referenced test for youth with disabilities
Offers options that can be individualized based on health-related needs
Targets the following populations
Visually impaired
Intellectual disability
Cerebral Palsy
Spinal Cord Injury
Amputation
Cardiorespiratory Endurance
Measured using Maximum Oxygen Uptake (VO2max)
VO2max increases throughout childhood
Slightly higher in boys than in girls
Estimated peak O2 consumption is measured in the field through distance run tests commonly a 1-mile run/walk
Studies report improved aerobic power with training suggesting the principles of training (frequency, intensity and duration) of children before puberty are similar to those for adults
Boxing, running, rowing, swimming, cross-country skiing and bicycling are highly correlated to improving cardiorespiratory endurance
Muscular Strength and Endurance
Strength is required for movement and effective performance
Important for optimal posture & reduced risk of low back pain
Lack of reliable, valid laboratory, and field standards for musculoskeletal fitness
Isokinetic and isometric dynamometry have been used in laboratories
Field tests such as the flexed arm hang, push up, curl up and trunk lift from the FITNESSGRAM are common but lack data
Muscular strength increases linearly with chronological age to ~age 13-14 years in both sexes (boys have greater strength than girls at all ages)
Strength and muscle mass can be achieved with training in children
Increases in strength, relate to increases in muscle mass during growth
Controversy exists as to the efficacy of strength training for children and adolescents