Geriatrics
1/174
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
175 Terms
What does presbycusis mean?
age related hearing loss
True or false: the ear loses some conduction function with increasing age
True
(High or low) frequency sounds are more difficult to distinguish with age
Give examples
High
(Female voices, higher pitched musical instruments, quick consonants (t, c, s)
What structural changes occur in the ear with age?
1. Eardrum thickens
2. Ear wax accumulates - affects hearing and balance and can cause tinnitus
Hearing loss in elderly can lead to significant _____________
Social isolation
Taste decreases with age due to a decrease in _________ and _________
Taste bud number and sensitivity
As we age it becomes harder to distinguish ______ and ______ tastes which makes food taste _____ and _____
Sweet and salty; bitter and sour
How does smell affect taste with age?
Smell decreases with age, especially subtle smells, which can cause food to taste bad
Taste decreases with age due to what 6 things?
1. Decrease in number of taste buds
2. Decrease in tongue sensitivity
3. Decrease in saliva (dry mouth) due to pharmaceutical side effects or a disorder
4. Gums may recede causing accumulation of plaque
5. Tooth enamel decays and leads to tooth loss
6. Smell decreases with age and causes food to taste bland
What 5 things happen to the skin with age?
1. Skin becomes thinner, drier, and less elastic (leads to wrinkles)
2. Fat layers which cushion skin decrease
3. The number of nerve endings in the skin decrease
4. Number of sweat glands and blood vessels decreases
5. Decrease in number of melanocytes
What is the negative impact of a reduction of melanocytes in the skin with age?
Less protection from UV light
What is the negative impact of decreased number of nerve endings in the skin as we age?
Causes a decrease in the sensation of pain, including temperature changes, which increases likelihood of injury
What is the negative impact of a reduction of sweat glands and blood vessels as we age?
As the blood flow decreases, especially to the skin's surface, the body cannot cool itself as easily when overheated leaving people more prone to heat stroke
It also slows healing processes
What happens to bones and joints as we age? (4)
1. Bone density decreases
2. The amount of bone marrow decreases
3. Cartilage thins
4. Ligaments decrease in elasticity due to changes in chemical composition
Bone density decreases with age due to decreases in _______ and _________ absorption
Calcium and vitamin D absorption
What is the negative impact of a decrease in bone marrow with age?
Fewer RBCs are made
Usually not a problem unless there is injury, infection, or disease (such as anemia)
What is the negative impact of thinning cartilage with age?
Joints don't flow as smoothly so injury can occur more easily
What is the negative impact of decrease in ligament elasticity with age?
Causes stiffness and flexibility decreases
Ligaments will then tear more easily and heal more slowly
Muscle mass and strength decrease with age, starting at age ______
30
True or false: the amount of fat in the body decreases with age
False; it increases
Overall loss in mass/brain weight of _____% in elders
10%
How does the brain compensate for the reduction in nerve cells in the brain with age?
Compensations made by new connections between remaining cells
After age ______, the number of cells in the spinal cord decreases which decreases sensation. This can lead to increase in susceptibility to injury and disorders
60
True or false: essential tremor is age-related, benign, and slowly progressive
True
Essential tremor usually manifests by age _____ and tremor amplitude slowly increases over time
65
Parkinson's tremor vs. essential tremor: which one decreases with posture holding and action?
Parkinson's
Parkinson's tremor vs. essential tremor: Which one has a higher frequency?
Essential tremor (5-12 Hz)
Parkinson's is only 3-6 Hz
Parkinson's tremor vs. essential tremor: which one is asymmetrical?
Parkinson's
Parkinson's tremor vs. essential tremor: which body parts are involved in each?
Parkinson's: hands and legs
Essential Tremor: hands, head, voice
Parkinson's tremor vs. essential tremor: which one has a stronger link to family history?
Essential tremor (30-50%)
vs. Parkinson's which is only 1%
What happens to the heart and blood vessels with age?
Walls of the heart stiffen and fill more slowly with blood. Artery walls thicken and become less elastic which means they are less able to respond to changes in the amount of blood pumped through them and this increases BP
What happens to lung function with age? (4)
1. The diaphragm weakens and less oxygen is absorbed from the air
2. Respiratory muscles lose strength and tissue loses elasticity
3. Alveolar surface area diminishes
4. Reduction in the number of cilia and villi
What is the negative impact of a reduction in the number of cilia and villi in the lungs with age?
Allows germs and debris to accumulate and therefore more severe infections may occur (coughing is not as efficient)
A decrease in ________ with age causes a decrease in the digestion a of dairy products resulting in lactose intolerance
Lactase
Which two organs decrease in function and affect drug metabolism with age?
Liver and kidneys
What reproductive changes are seen in women as they age?
Estrogen levels DECREASE after menopause making pregnancy impossible, and the skin direr and less elastic.
There are generally no changes in libido
What are the reproductive changes seen in men with age?
Testosterone levels decrease in men but do not generally affect reproduction potential.
Libido may decrease and impotence may increase
Aldosterone can (increase or decrease) with age, causing an increase in dehydration
Decrease
What happens to melatonin levels with age?
Decrease; causes insomnia
Pineal gland synthesizes melatonin from the neurotransmitter ___________
Seratonin
True or false: allergies become more severe with age
False; they become less severe
True or false: vaccines are less effective with age
True
More likely to have life-threatening simple infections like influenza or pneumonia
True or false: immune system becomes less effective with age
True
Not usually noticeable unless severe infection present.
Autoimmune diseases increase because the immune system cannot distinguish its own cells from other foreign substances
What does rhytid mean?
Wrinkle
What is malar fat descent?
as fat composition in skin changes and skin loses elasticity, gravity can cause malar fat to descend below the orbital rim, leaving the lower peri orbital area "hallowed"
Fluid can accumulate in the peri orbital area and presents as bags under a patient's eye
What is the recommended treatment to help with malar fat descent?
Low salt diet, especially prior to bed
What causes an involutional ptosis?
Due to dehiscence or stretching of the levator aponeurosis connection to the tarsal plate
When is surgery of a ptosis recommended?
Recommended to be medically necessary (covered by insurance) when function is reduced and demonstrated on perimetry ("functional ptosis")
How do you prove a medically necessary ptosis surgery?
2 VFs must be done, one with taped lid and one without. VF loss from a lid will be an absolute defect (<0 value)
What is the difference between dermatochalasis and ptosis?
Dermatochalasis occurs when redundant lid skin falls beyond eyelid margins, muscle function is normal but it is the extra skin causing the drooping
Measured MRD1 is normal if skin is retracted and measured
What are the 2 types of orbital fat prolapse?
1. Intraconal - subconjunctival herniated orbital fat
2. Extraconal fat prolapse
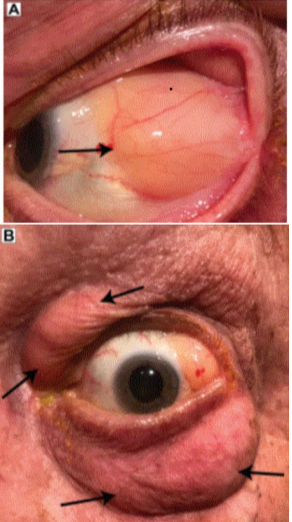
What does intraconal mean? Extraconal?
Inside the extra-ocular muscle cone
Outside the extra-ocular muscle cone
What location of intraconal orbital prolapse is more common?
Superiotemporal
Which is more common, intraconal or Extraconal orbital prolapse?
Extraconal (very common age-related finding)
List the differentials for intraconal fat prolapse
1. Conjunctival dermolipoma
2. Conjunctival lymphoma
3. Epidermoidal cyst
4. Prolapse of lacrimal gland
What does the term festoon mean?
Extraconal fat prolapse
What is the difference between TED and involutional eyelid changes?
In TED the eyebrow and cheek fat tends to grow alongside the orbital fat, and congestion from inflammation can also occur in the orbital fat. These patients will have difficulty closing their eyes, involutional ptosis or dermatochalasis will NOT
What causes a brow ptosis?
With age, the bones of the skull undergo a rotational shifting, leading to a more prominent brow that looks like an involuntional eyelid ptosis
What causes involutional ectropion?
Occurs due to acquired horizontal laxity of the eyelid and canthal tendons (lateral, medial)
What is the snap back test?
Used to assess entropion and ectropion
Evert lower lid down and away from orbit, look for response as you release the lid. Normal eyelid muscle tone will return to its proper position opposed against the globe within 1-2 seconds, with or without a blink
What is considered a positive "snap back" test?
When the eyelid fails to "snap back" into proper apposition with the globe and there is visible lower lid laxity
List the grades for the grading system of the "snap back" test
Grade 0 - eyelid returns to position immediately upon release
Grade 1 - eyelid returns 2-3 seconds after release
Grade 2 - 4-5 second response time
Grade 3 - >5 seconds returns to position with a blink
Grade 4 - severe laxity, does not return to position against the globe
Lacrimation _________ with age
decreases
Tear production at age 40 is ______ of that in the first decade of life; at age 80 it is ________
1/2; 1/4
What is the difference between tear thinning time and tear break up time?
Similar except TTT does not use NaFl
Tear thinning time decreases by ______ between the ages of 8 and 80
Half
True or false: there are no significant clinical studies on changes in the blinking with age
True
But it likely contributes to change in tear film
What corneal changes happen with age? (2)
1. Corneal sensitivity decreases
2. Corneal endothelial density decreases with age
Threshold to touch the cornea doubles between the ages of ____ and ____
10 and 80
What is the corneal endothelial density at birth? Adult? 9th decade?
Birth: 3500-400 cells/mm^2
Adult: 1400-2500 cells/mm^2
9th Decade: 900 cells/mm^2
in the normal eye free from cataract and diabetes, refractive change is _________ until age 70. Why?
Hypermetropia
Due to increase in axial thickness of lens and flattening of anterior surface
After age 70 refractive change trends towards ______. Why?
Myopia
Due to growth of crystalline lens (increases refractive power of eye)
______ astigmatism increases with age
ATR
Depth of anterior chamber _______ with age. Why?
Decreases
Due primarily to growth in crystalline lens
Typical AC depth for 15-20 year old is ______mm vs. 70 year old which is ______mm
15-20: 3.6mm
70: 3.0mm
What causes the pupil size to decrease with age?
Due to atrophy of the dilator and increased rigidity of iris blood vessels
The difference between light and dark-adapted pupils ________ with age
Decreases
How should you adjust refraction to account for the reduced pupil size in the elderly?
Because this will increase their depth of focus and decrease their blur circle, it may make the standard +/- 0.25D JCC difficult between the two choices. Should adjust by using +/- 0.50D JCC if response in phoropter isn't defined
Axial thickness of the lens (increases or decreases) with age
Increases
What happens to the nuclear thickness and cortical thickness of the lens with age?
Nuclear = remains relatively constant
Cortical = increases
Equatorial diameter of the lens (increases or decreases) with age
Increases
In the lens, growth in the __________ diameter is much slower than growth in the ________ diameter
Equatorial; axial
The lens becomes (steeper or flatter) with age
Steeper
The radius of curvature of the central portion of the anterior surface of the lens decreases by about _______mm/year
0.1mm/year
?
True or false: the radius of curvature of the central portion of the posterior lens surface remains fairly constant throughout life
True
What are the 2 explanations for lens yellowing with age?
1. Lens thickening and lens pigmentation
2. Chronic UV exposure induces a photochemical generation and accumulation of two chromophores which increase in accumulation with age
What happens to the ciliary body with age? Does this affect accommodation?
It becomes hypertrophic rather than atrophic with increasing age, and is not thought to be the source of the loss of accommodative function
What causes the loss of accommodative function with age?
Changes in the lens. Lens capsule loses elastic force, fibers become more compacted with age
Dark adaptation threshold (increases or decreases) with age. Why?
Increases
The decline in sensitivity is due to media and neural changes, but lens changes and pupillary miosis are the primary causes of decreased dark adaptation
____% of the elderly use prescription medications
71%
_____% of the elderly use OTC meds
54%
25% of the elderly take ____ or more prescription meds
4
The elderly uses ______% of ALL prescription medications
25-35%
____% of the elderly's out-of-pocket health care budget is spent on prescription and OTC meds
50%
What does the acronym ADME stand for?
A-absorption
D-distribution
M-metabolism
E-excretion
Majority of drug absorption occurs in the GI system, most in _______ and __________
Stomach and intestine
How is absorption of drugs affected with age (4)
1. There is atrophy and thinning of stomach mucosa, and accelerated and sustained cell turnover leading to a decreased secretion of mucous
2. There is an elevation of gastric pH with age that may alter ionization and solubility of some drugs
3. There is decreased gastric emptying (allows ulceogenic drugs like NSAIDs to remain in contact with gastric mucosa longer)
4. There is decreased intestinal motility
What does drug distribution mean?
The process by which a drug reversibly leaves the bloodstream and enters the interstitium (extracellular fluid) and/or cells of the tissues
What 4 things does drug distribution depend on?
1. Body composition (body weight, body fat, body water)
2. Plasma protein binding
3. Blood flow to the organs (perfusion)
4. Hydrophobicity of the drug
What happens to body composition in elderly patients? (2) What does this cause?
1. Decrease in total body water and lean body mass
2. Increase in the percentage of body weight contributed by body fat
These changes lead to reduced volume of distribution (Vd) for water-soluble drugs and an increased volume of distribution for fat-soluble drugs as they accumulate in adipose tissue