L8 | Fluid and Electrolyte Imbalances
1/50
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
51 Terms
______________ — volume of fluid within all cells
Intracellular Fluid (ICF)
___________ — all non-intracellular fluid (interstitial fluid [ISF], intravascular compartment [plasma], lymph and transcellular [other])
Extracellular fluid (ECF)
Total body water (TBW) = ________% of body weight in liters
60%
The amount of __________ in the body is a prime determinant of the ECF volume
sodium
Excess sodium is secreted by the ____________
kidneys
Solutes (NaCl, NaHCO3) are confined to the ______________ compartment
ECF
What is the result of dietary salt overload?
-adds NaCl to the ECF compartment
-increases total solute concentration of the ECF (increases OsmECF)
What is the result of dietary water overload?
-decreases total solute concentration of the ECF (decreases OsmECF)
[Na+]plasma indicates ________________
water balance
-not Na+ balance
[Na+]ECF controls __________________
ECF/ICF water distribution
___________ describe the pressures that control fluid movement in and out of capillaries.
Starling Forces
________ and ________ are hydrostatic pressures that push fluid
-Capillary pressure (PC)
-interstitial fluid pressure (Pif)
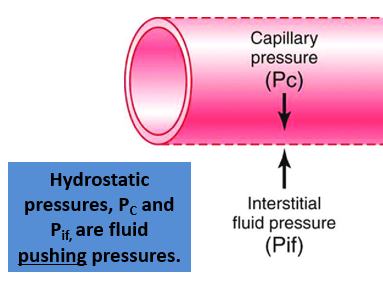
___________ and _________ are colloid osmotic pressures that pull fluid
-Plasma colloid oncotic pressure (πp)
-Interstitial fluid colloid osmotic pressure (πif)
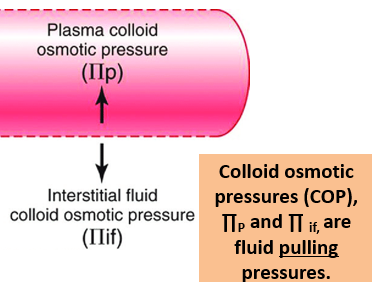
Which starling forces keep plasma fluid inside the capillary?
-Plasma colloid ocmotic pressure (πp)
-interstitial fluid pressure (Pif)
Which starling forces keep plasma fluid inside the interstitial fluid?
-Capillary pressure (PC)
-Interstitial fluid colloid osmotic pressure (πif)
What occurs at the arterial end of the capillary?
-blood pressure is greater than colloid osmotic pressure
-fluid flows out of the capillary into the interstitial fluid
What occurs at the venular end of the capillary?
-blood pressure is less than colloid osmotic pressure
-fluid flows from the interstitial fluid into the capillary
True/Flase: The amount of fluid that is filtered at the arterial end equals the amount of fluid absorbed at the venular end
True
Edema is produced by an increase in ______________
interstitial fluid volume
Edema does not become evident until the interstitial fluid (ISF) has been increased by __________
3 liters
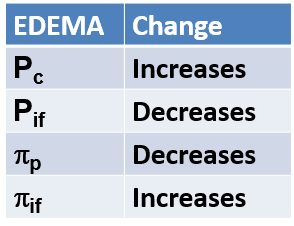
Why does edema occur?
Starling forces have a strong favoring of fluid filtration out of the capillary and into the interstitium
-fluid from capillary pushed or pulled into the interstitium.
What are the changes in starling forces that make edema happen?
_______ edema only occurs at the site of trauma
Localized
_______ edema is associated with diseases such as renal failure
Systemic
________ edema is where fluid pools in gravity-dependent areas, may be a sign of systemic edema, and is also known as pitting edema
Dependent
What are the four physiologic mechanisms that contribute to edema?
-increased capillary permeability
-decreased plasma oncotic pressure
-increased plasma hydrostratic pressure
-obstruction to lymph flow (lymphedema)
How does increased capillary permeability contribute to edema?
When capillary pores become enlarged or the integrity of the capillary wall is damaged, capillary permeability is increased → large Plasma proteins and other osmotically active particles leak into the interstitial spaces, increasing the tissue colloidal osmotic pressure and contributing to the accumulation of interstitial fluid.
-causes: burn injury
How does decreased capillary oncotic pressure contribute to edema?
May be caused by decreased plasma protein synthesis (liver disease), glomerular diseases, drainage from large, open wounds
-liver typically synthesizes the plasma proteins, including albumin
-produce generalized edema
How does increased capillary hydrostatic pressure contribute to edema?
-localized edema — allergic or inflammatory conditions resulting from the release of histamine or other inflammatory mediators
-generalized edema — result of increased vascular volume, caused by venous obstruction, excessive salt intake, or water retention due to congestive heart failure or renal failure
How does obstruction of lymphatic flow contribute to edema?
-Obstruction of lymphatic flow prevents excess interstitial fluid and proteins from being returned to the circulation, causing fluid to accumulate in the tissues. This buildup of fluid results in edema.
-Edema due to impaired lymph flow is commonly referred to as lymphedema
-May be caused by infection, surgical excision of lymph nodes or tumors
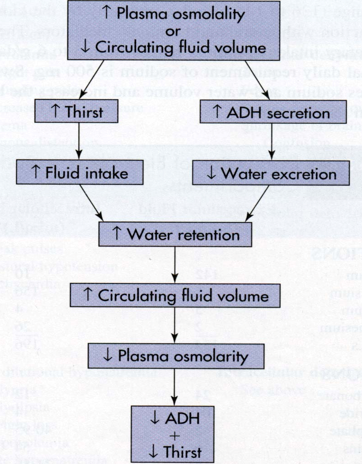
How do increased levels of antidiuretic hormone (ADH) decrease urine output?
ADH prevents diuresis by causing more water to be reabsorbed in the collecting ducts (CD) of the kidneys. If more water is reabsorbed, there is less water left to eliminate as waste, decreasing urine output.
What does high osmolarity result in?
-increase in thirst
-increase in ADH secretion
What does low osmolarity result in?
-lack of thirst
-decreased ADH secretion
How is high osmolarity related to low osmolarity?
-low osmolarity balances high osmolarity
-high osmolarity causes increased thirst and ADH secretion, which increases water retention, which increases circulating fluid volume. This then causes low plasma osmolarity to decrease thirst and ADH secretion
_________ is excessive thirst
Polydipsia
__________ and _________ can cause inappropriate/false thirst
-Congestive heart failure
-Chronic kidney disease
__________ is the decreased ability to sense thirst
Hypodipsia
What causes hypodipsia?
Damage to brain cells (osmoreceptors) that are responsible for detecting the osmolarity of the extracellular fluid
Thirst is regulated by the _____________ in the ______________
osmoreceptors; hypothalamus
________ is where the kidneys pass an abnormally large volume of urine that is insipid (diluted & odorless)
Diabetes insipidus (DI)
What causes diabetes insipidus?
deficieny of or decreased response to ADH, which causes the inability to concentrate urine even during periods of water restriction which results in polyuria (increased urine production)
Identify this type of diabetes insipidus:
-lack of ADH production in the hypothalamus
-symptoms: polyuria (increased urine output), nocturia (urinating at night), polydipsia (excessive drinking)
Neurogenic
Identify this diabetes insipidus:
-kidneys do not respond to ADH, impairment of urine concentrating ability
-symtpoms: polyuria, nocturia, polydipsia
Nephrogenic
Identify this type of diabetes insipidus:
-defect of or damage to thrist mechanism (hypothalamus)
Dipsogenic
Identify this type of diabetes insipidus:
-excess placental production of vasopressinase (increased breakdown of mother’s ADH)
Gestational
__________________ — body retains water instead of excreting in urine due to inappropriate elevated ADH
Syndrome of inappropriate ADH (SIADH)
What causes SIADH?
-failure of negative feedback, which leads to dilutional hyponatremia (low sodium concentration in plasma)
What are some potential causes of syndrome of inappropriate ADH (SIADH)?
-surgery
-intracranial (infection or head injury)
-alveolar
-drugs
-hormonal
How is syndrome of inappropriate ADH treated?
-fluid restriction
-diuretics
Why would retaining sodium cause high blood pressure?
The excess sodium is going to hold onto water. That sodium is in the extracellular compartment, which plasma is also located
-increase in volume = increase in pressure
It's a very hot day and a PT falls down the stairs on the way to see the doctor about their hepatitis and renal disease. Explain why they have edema in their sprained ankle and foot?
1.Hepatitis – decreased albumin production by diseased liver leads to decreased plasma oncotic pressure (∏P)
2.Renal disease – proteinuria resulting from loss of protein in urine leads to decreased plasma oncotic pressure (∏P)
3.Fall – inflammation and leaky capillaries leads to increased capillary hydrostatic pressure (Pc) and decreased plasma oncotic pressure (∏P)
-all cause an increase in filtration of fluid from capillaries into the interstitial fluid which leads to edema