Cleaning, Disinfection, and Sterilization
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
decontamination
combination of processes, in which pathogens are removed, inactivated or destroyed, to render a reusable item safe for further use
cleaning
Physically removes infectious agents and the organic matter
sanitize
Reduces the number of pathogens on a surface
disinfection
Process of inactivating pathogenic organisms except for bacterial spores
sterilization
Elimination of all viable microorganisms
antisepsis
A specific kind of disinfection, one that is mild enough for tissue
uses chemicals to disinfect tissue, such as skin or mucous membrane
sanitation
Removal of pathogenic microorganisms from inanimate articles by mechanical or chemical means
-cidal
suffix meaning death
-static
Suffix meaning the microorganism can no longer grow, but is not killed
low level disinfectants
Effectiveness: Low-level disinfectants are effective against most bacteria, some viruses, and fungi. They do not reliably kill bacterial spores.
Common Uses: Typically used for surfaces and equipment that come into contact with intact skin but are not involved in invasive procedures. Examples include general cleaning of floors, walls, and non-critical surfaces.
intermediate-level disinfectants
Effectiveness: Intermediate-level disinfectants are effective against a broader range of microorganisms, including bacteria, viruses, and fungi. They can kill mycobacteria (e.g., Mycobacterium tuberculosis) but generally do not kill bacterial spores.
Common Uses: Used for surfaces and equipment that come into contact with mucous membranes or non-intact skin, such as examination tables and other non-critical items. They are often used in medical settings where more thorough disinfection is required than low-level disinfectants can provide.
high-level disinfectants
Effectiveness: High-level disinfectants are capable of killing all microorganisms except large numbers of bacterial spores. They are used for items that come into contact with sterile tissues or are used in sterile procedures.
Common Uses: Typically used for semi-critical items that come into contact with mucous membranes or non-intact skin, such as endoscopes and some surgical instruments. They are also used for items that require high-level disinfection but are not suitable for autoclaving.
critical - splauding’s classification
Items that come in contact with normally sterile human tissue
Sterile
(i.e. scalpels, needles)
semi-critical - splauding’s classification
Items that come in contact with non-sterile mucous membranes or body surfaces
Free of pathogens
(i.e. endo-cavity probes)
non-critical - splauding’s classification
Items that come in contact with skin but not mucous membranes
(i.e. counter tops, beds, stretchers, u/s probe)
quaternary ammonium compounds (quats)
Detergents, low level disinfectants.
Quats attach to microbial cell membranes and cause a lethal disruption of the cell.
Quats were used for cleaning, disinfection of surfaces and skin antisepsis.
Effective against: Gram positive bacteria, fungi and most lipid viruses.
Not effective against: Bacterial spores, tubercle bacilli, HBV and non-lipid viruses are unaffected by quats.
Quats are inactivated by organic material, gauze and other plant fibers, soaps, hard water and other detergents.
Cases of nosocomial infections caused by Pseudomonas have been traced to contaminated solutions of quats.
alcohols
Ethyl alcohol (ethanol) and isopropyl alcohol (isopropanol) are the only two alcohols useful as disinfectants.
Low level disinfectant.
Used for skin antisepsis.
Advantages of Alcohol
•Economical
•Very little irritation to human tissue
•Ability to kill bacteria, some lipid viruses, and tubercle bacilli (in the absence of body fluids).
Disadvantages of Alcohol
•Antimicrobial action diminishes with heavy microbial load and organic material
•Does not kill spores and non-lipid viruses
•Rapid evaporation before proper disinfection
•Very drying
chlorine
Chlorine is readily available, effective, economical disinfectant. (intermediate level disinfectant)
Chlorine may be added to water to create a potent oxidizing agent that rapidly kills microorganisms.
Chlorine disinfectants are rapidly lethal to vegetative bacteria with most bacteria being killed in less than one minute.
Bacterial spores are more resistant to chlorine disinfectants and only extended exposure with strong solutions will kill spores.
Undiluted bleach is not recommended for use as a disinfectant and different strengths of bleach are required for different uses.
Chlorine based disinfectants are inactivated by organic material such as blood and mucus. This must be taken into consideration when deciding the concentration of bleach that is needed.
Advantages of Chlorine-Based Disinfectants
•Economical and readily available
•Rapid antibacterial action
•Kills tubercle bacilli and viruses
•Effective in diluted solutions
Disadvantages of Chlorine-Based Disinfectants
•Corrosive to metals and degrades plastics and rubber
•Must be diluted fresh daily
•Unpleasant odor and irritating to skin and eyes
•Inactivated by organic matter
•Only sporicidal at high concentrations
•Spoils your clothes if accidentally spilled
iodine
Iodine was one of the first antiseptics used to cleanse skin, wounds and mucous membranes.
Iodine has a wide antimicrobial spectrum killing vegetative bacteria, tubercle bacilli, fungi, most viruses and some bacterial spores (intermediate level disinfectant).
Most iodine disinfectants used in the health care setting are iodophors.
Iodophors are less irritating to tissue, less allergenic and do not stain skin and clothing as much as tincture of iodine.
Betadine, Dovidine, and Prepodyne are iodophors that are used for skin antisepsis.
Used for intact skin antisepsis preceding surgical incision or as skin preparation for venipuncture or to collect a blood culture.
Advantages of Iodophors
•Economical and may be diluted for use
•Broad spectrum acts within ten minutes
•Good cleaning agent when coupled with detergent
•Residual action
Disadvantages of Iodophors
•Must be diluted fresh daily and not be diluted with hard water
•Discoloration of some materials such as plastics
•Allergies
glutaraldehyde
Powerful disinfectant - high level disinfectant.
Glutaraldehyde 2% solution = proven to kill most bacteria within five minutes, tubercle bacilli and viruses in ten minutes and spores in ten hours.
Used for surface disinfection of some metal laboratory equipment where blood spills are present.
Glutaraldehydes do not cause corrosion or destruction of plastics, rubber and most metals.
Glutaraldehyde is considered to be effective for killing both hepatitis B virus and HIV, but not HPV.
Glutaraldehyde is used extensively for the disinfection of instruments and equipment that can not be sterilized by heat.
Advantages of Glutaraldehyde
•Broad antimicrobial spectrum
•Does not destroy rubber and plastic items
•Not inactivated by blood or body secretions
Disadvantages of Glutaraldehyde
•Expensive in the amounts required for immersion of items
•Toxic to skin and mucous membranes
•Fumes are irritating •Shelf life after activation must be adhered to
peroxygens
Hydrogen peroxide and peracetic acid are oxidizing agents that are effective disinfectants.
Peroxygens are high-level disinfectants.
*Trophon systems use hydrogen peroxide.
Advantages of Peroxygens •Readily biodegradable
•Rapid action in low concentration
•Minimally affected by organic compounds
•Leaves no residue
•Broad spectrum
•Can be used on a wide variety of surfaces (low corrosivity)
Disadvantages of Peroxygens
•High concentrations are irritants
•Unstable when diluted
cleaning in the ultrasound department
Potential for equipment and surface contamination
Patient environment means the patient and the area immediately (within 2 metres) surrounding the patient. It can accompany the patient in the healthcare environment, wherever the patient goes (e.g. a patient’s wheelchair, walker or IV pole; if the patient is in a lounge or dining room).
The patient environment includes any surfaces touched by the patient or healthcare provider during care, such as bedrails, over-bed tables, bedside table, infusion pumps and tubing, and nearby surfaces touched by the healthcare provider including monitors, knobs, and high frequency touch surfaces.
Accountability and record keeping of cleaning are determined by the department itself or Infection Prevention and Control staff.
Potential for equipment and surface contamination.
Remember we do not always see the contamination.
endocavity probe reprocessing - trophon
closed system that uses hydrogen peroxide to decontaminate and disinfect ultrasound transducers, especially endocavity transducers
uses ultrasonic vibration to convert high concentration hydrogen peroxide into mist particles that can access very small spaces to ensure all areas of the item are disinfected
Trophon reduces the risk of ultrasound-related cross-infection:
•Highly effective bactericidal, fungicidal and viricidal high-level disinfection to reduce the risk of patient cross-contamination.
•Proven to kill high-risk HPV (Ryndock, Robinson, & Meyers, 2015).
•Offers a safer patient environment as infection risk in a healthcare facility is greatly reduced (Vickery, et al., 2013).
•An automated closed system minimizes patient exposure to chemicals.
endocavity probe reprocessing - glutaraldehyde
high-level disinfectant used for the reprocessing of ultrasound probes, particularly those that come into contact with mucous membranes or non-intact skin
1. Preparation:
Check Solution Concentration: Use a glutaraldehyde solution with a concentration of 2-3%. Ensure that the solution is freshly prepared or within its recommended use period.
Safety Precautions: Wear appropriate personal protective equipment (PPE) such as gloves, goggles, and masks to protect against the toxic effects of glutaraldehyde vapors and splashes. Work in a well-ventilated area or fume hood if available.
2. Pre-Cleaning:
Remove Debris: Before disinfection, thoroughly clean the ultrasound probe to remove any organic material such as blood, gel, or other residues. This can be done using a mild detergent and water, followed by rinsing with clean water.
Dry the Probe: Ensure the probe is dry before proceeding to disinfection, as excess moisture can dilute the glutaraldehyde solution and affect its efficacy.
3. Disinfection:
Immerse the Probe: Submerge the cleaned and dried probe completely in the glutaraldehyde solution. Ensure that the probe is fully covered and that no air bubbles are trapped within the probe’s crevices.
Contact Time: Allow the probe to remain in the glutaraldehyde solution for the manufacturer-recommended contact time, typically 20-30 minutes. This ensures effective disinfection of all surfaces.
4. Rinsing and Drying:
Rinse Thoroughly: After the contact time has elapsed, carefully remove the probe from the glutaraldehyde solution. Rinse the probe thoroughly with sterile water or a suitable rinsing solution to remove any residual glutaraldehyde, which can be irritating to tissues and affect the probe’s performance.
Dry the Probe: Dry the probe completely using a clean, lint-free cloth or air-dry it in a clean, designated area to prevent any residual moisture from affecting its functionality.
5. Storage and Handling:
Store Properly: Store the reprocessed probe in a clean, dry, and appropriately labeled area to prevent contamination before its next use.
Dispose of Solution: Properly dispose of the used glutaraldehyde solution according to your facility’s hazardous waste disposal protocols to ensure safety and environmental compliance.
6. Documentation:
Record Keeping: Document the reprocessing procedure, including the date, time, solution concentration, and contact time, in accordance with your facility’s infection control policies and regulatory requirements.
sterile/surgical asepsis
the absence of all microorganisms within any type of invasive procedure
sterilization
Destroys all forms of microbial life
Categories of Sterilization:
•Incineration
•Autoclave
•Chemical/Ethylene Oxide
•Irradiation
incineration
•To burn or reduce to ash
•Very effective method of terminal sterilization
•Some hospitals have their own incinerators and some ship biological waste to a commercial incineration site.
•The preferred method biomedical waste is incineration.
Examples of material that is incinerated:
•Used needles and syringes
•IV sets
•Used gloves
•Discarded Bandages
•Lab cultures
•Blood products
autoclave
•A pressure cooker that uses steam to kill microorganisms
•Typically, not used for rubber or plastic
•Used for metal, cloth, gauze
•uses chemical indicators to confirm sterilization
Sterility Check
A biological monitor (bacterial spores) is commercially available and used to test quality assurance of the autoclave. These tests should be run weekly of whenever a procedure change is made.
chemical/ethylene oxide
Gas sterilization that uses Ethylene Oxide (ETO).
This is expensive and toxic to human tissue.
Materials must be aerated before human contact.
Used for non-disposable equipment made from plastic or other heat sensitive materials such as endoscopes.
irradiation
•Facilitated with Gamma Rays – not typically used in health care facilities
•An effective method of sterilizing many products that are composed of different materials, with varying densities, configurations and orientations.
Gamma radiation is ideal for:
•Sterilization of single-use medical supplies(opens in a new tab) such as syringes, implants, catheters, IV sets, surgical gloves, gauze, etc.
•Eliminating organisms from ointments and solutions
•Sterilization of biological based products such as tissue
autoclave tape
white lines turn black when sterilization is complete
paper strips or sterile gauge
black line moves into the accept range when sterilization is complete
3 basic workers rights:
right to know
right to participate
right to refuse
purpose of WHMIS
provide information about the hazards of chemicals used in the workplace and how to handle them safely
components of WHMIS
Labels: Provide essential information about hazardous materials, including the type of hazard and handling instructions.
Safety Data Sheets (SDS): Detailed documents that provide information on the safe handling, storage, and emergency procedures for hazardous materials.
Worker Education and Training: Ensures that workers understand the information provided by labels and SDS, and know how to protect themselves from hazards.
labels
Identification: Learn to recognize WHMIS labels on containers, which include symbols, signal words (e.g., Danger, Warning), and hazard statements (e.g., causes skin irritation).
Information: Read and understand the information on labels to handle materials correctly and follow safety precautions.
safety data sheets (SDS)
Access: Know where to find SDS for chemicals used in your workplace. SDS are typically available in a central location or through a digital system.
Content: Familiarize yourself with key sections of SDS, such as hazard identification, handling and storage, first aid measures, and emergency response.
hazard recognition
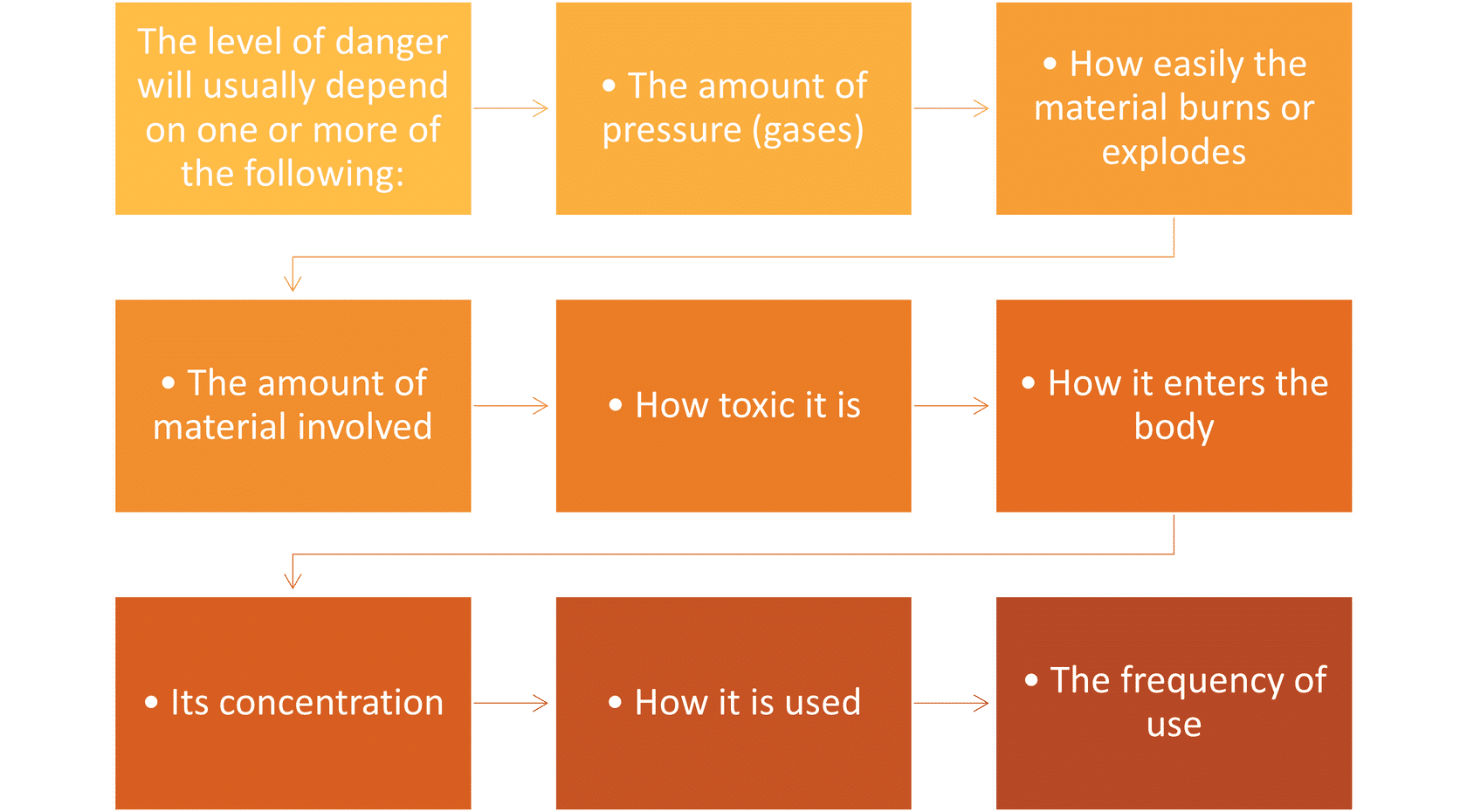
Types of Hazards: Understand different types of hazards that may be present in your work environment, including chemical, biological, and physical hazards.
Protective Measures: Learn the appropriate personal protective equipment (PPE) and procedures to minimize exposure to hazardous materials.
emergency procedure
Response Actions: Be aware of the procedures for responding to spills, exposure incidents, or other emergencies involving hazardous materials.
First Aid: Know basic first aid measures and emergency contact information for dealing with chemical exposure or other hazards.
training and compliance
Training: Participate in WHMIS training sessions provided by your employer to stay informed about the latest safety protocols and regulatory requirements.
Compliance: Follow all WHMIS guidelines and procedures to ensure a safe working environment and maintain compliance with workplace safety regulations.
role specific considerations
Sonography Equipment: Be aware of the specific chemicals used in ultrasound equipment maintenance, such as cleaning agents and gel, and ensure proper handling and disposal.
Workplace Environment: Understand how WHMIS applies to your specific work environment, including any additional safety measures for the unique aspects of a healthcare setting.
SDS lets us know..