Neurological Disorders
1/106
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
107 Terms
cognitive deficits may be due to a temporary malfunction, known as ______, or a gradual and permanent loss of cognitive function, known as ______
delirium, dementia
__________ represents the person's ability to process or retrieve what had previously been acquired.
Cognitive functioning
Complex attention
sustained attention,
divided attention,
selective attention,
processing speed
Complex attention major s/s
difficult concentrating with environment w. lots of stimuli.
Longer thinking and processing
needs simple and restricted input
Complex attention minor s/s
can process better without distractions
normal task take longer and more double-check
sustained attention assess
press button when tone heard
divided attention assess
tapping while listening to story
selective attention assess
count letters while hearing numbers and letters outload
process speed assess
time on task
executive function
planning
decision making
respond to feedback
working memory
mental flexibility
overriding habits
executive function major s/s
stops complex projects
focus one task at time
needs others to plan activities and make decisions
executive function minor s/s
more effort needed to complete multistage projects
difficulty multitasking
planning assess
ability to interpret a sequential picture or object arrangement/find exit
decision-making assess
tasks that involve deciding between alternatives
responding to feedback assess
infer rules from solving a problem
working memory assess
adding up a list of numbersment
mental flexibility assess
shift between two tasks, concepts, response rules (number to letter, verbal to keypress)
overriding habits assess
ability to name the color of word’s font, rather than the word
learning and memory
immediate memory, recent memory, very long-term memory
Except in severe forms of major neurocognitive disorder, semantic, autobiographical, and implicit memory are relatively intact, compared with recent memory.
learning and memory major s/s
repeats self in conversation
cannot keep track of short list of items when shopping or planning
learning and memory minor s/s
difficulty recalling recent events, needs reminders and lists
immediate memory
ability to repeat lists of words or digits
recent memory
word lists, short story, diagram
language
expressive
grammar and syntax
receptive language
language major s/s
significant difficulties w/ expressive/reactive language
uses pronouns rather than names and general use words like “that thing”
language minor s/s
noticeable word-finding difficulty
substitutes general for specific names of acquaintances
subtle grammatical errors
expressive
identify objects or pictures, or words starting with certain letterGr
grammar and syntax
errors observed during naming and fluency testsr
receptive language
comprehension or performing action
perceptual-motor
visual perception
visuoconstructional
perceptual-motor
praxis gnosis
perceptual motor major s/s
significant difficulties w/ previously familiar activities and environment.
often confused at dusk
perceptual motor mild s/s
relies more on maps and others for directions
uses notes
frequently lost if not concentrating on task
less precise in parking
greater effort for spatial tasks
visual perception
facial recognition
visuoconstructional
drawing, copying, block assembly
perceptual motor
inserting blocks into a form board w/o visual cues
praxis
imitating gestures or learned movements
gnosis
recognition of faces and colors
social cognition
recognition of emotions
theory of mind
social cognition major s/s
insensitivity to social standards of modestly and topics of conversation
makes unsafe decisions
social cognition minor s/s
subtle behavior or attitude changes
decreased empathy and inhibition, restlessness
recognition of emotions
identify emotions on faces
theory of mind
story cards with questions to elicit information about mental state of people in story
delirium vs dementia vs depression onset
delirium: hours-days
dementia: months to years
depression: gradual and exacerbation w/ stress
delirium vs dementia vs depression contributing factors
delirium: dehydration, low BG, fever, infection, hypoTN, drug reaction, heat injury
dementia: Alzheimer, vascular disease, HIV, traumatic brain injury, chronic SUD, neurological disorders
depression: lifelong or related to losses, crises, health/medical conditions, loneliness
delirium vs dementia vs depression cognition
delirium: impaired memory, judgment, attention, calculation
dementia: impaired memory, judgment, attention, calculation + abstract thinking, agnosia
depression: forgetfulness, inattention, difficulty concentrating
delirium vs dementia vs depression LOC
delirium: altered
dementia: not altered
depression: not altered
delirium vs dementia vs depression activity level
delirium: varies, restlessness, sundowning, sleep disruption
dementia: may have sundowning
depression: Decreased activity, fatigue, lethargy, poor sleep, lack of motivation
delirium vs dementia vs depression emotional state
delirium: Rapid mood swings; can be aggressive, fearful, anxious, paranoid (suspicious), and have hallucinations or delusions
dementia: flat affect, delusional
depression: Sad, apathetic, anxious, irritable, inappropriate guilt, can be paranoid
delirium vs dementia vs depression speech and language
delirium: rambling, inappropriate rapid, incoherent
dementia: slow and incoherent, repetitious, inappropriate
depression: slow, low, flat
delirium vs dementia vs depression prognosis
delirium : can be reversed with intervention
dementia: will worsen
depression: medication and psychotherapy
delirium
disturbance in attention and cognition that develops over short time + disturbance of cognition
sleep-wake cycle and emotional disturbances
due to substance intoxication
substance intoxication → delirium
alcohol, cannabis, phencyclidine, hallucinogens, inhalants, opioids, sedatives/hypnotics/anxiolytics, amphetamines, and cocaine
withdrawal can lead to delirium
metabolic disorders (thyroid disorders), neurological disorders (head trauma), tumors, vitamin B-12 deficiencies, physical stressors (pain or sleep deprivation), and drugs like lithium, levodopa, tricyclic antidepressants, benzodiazepines, central nervous system depressants, digitalis, and steroids, dehydration
hepatic encephalopathy
older adult clients who are dehydrated or w/ UTI
delirium s/s
irritability, confusion, hyperactivity, trembling (DT’s, can be cause by alcohol withdrawal), tachycardia, sweating, tremors, nausea, vomiting, impaired consciousness, seizures, and hallucinations (visual, auditory, and tactile)
→ to death if not intervened
(use BZ, barbiturates, antipsychotics)
worsens if older, had medication, psychiatric disorder, poor diet
major neurocognitive disorder
wide range of disorders of cognitive functioning which interfere w/ ADLs
(DSM-5-TR) mild cognitive → major
DSM-5-TR disorders
Alzheimer’s disease, frontotemporal degeneration, Lewy body disease, vascular disease, traumatic brain injury, substance/medication use, HIV infection, prion disease, Parkinson’s disease, Huntington’s disease, and other medical conditions/multiple etiologies/unspecified etiology
alzheimer’s disease
from family hx
Decline in memory, learning, and cognition
insidious onset and gradual progression of impairment due to accumulation of amyloid plaques in neurons
evidence of memory and learning decline
at least one other cognitive domain decline;
progressive decline in cognition;
no evidence of a mixed etiology.
~10y prognosis = severe dementia → death
major Alzheimer DSM
genetic testing or family hx + :
Evidence of memory and learning decline, and at least one other cognitive domain
Gradual, but steadily progressive decline in cognition, without any extended plateaus
No evidence of mixed etiology
minor Alzheimer
Probable Alzheimer's disease with evidence of a genetic mutation from genetic testing and/or family history and possible Alzheimer's disease with no evidence
good ADLs and communication but may displace objects or forget appointments examples:
not choosing the right word or name,
forgetting material that was just read or names of people just introduced,
having difficulty performing tasks,
having trouble planning or organizing,
and losing or misplacing objects.
neologisms, deficit of language and memory.
keep working on healthy behaviors + make end of life decisions
Moderate Alzheimer
needs more help → frustrated, confused, angry, and irritable → trouble expressing thoughts, or simple tasks
forgetting events or personal history,
being withdrawn or labile (moody),
having trouble recalling information,
being confused about location or time,
needing help dressing appropriately for the occasion or season,
experiencing disrupted sleep patterns,
having a tendency to wander or become lost
, demonstrating behavioral changes,
and losing bowel/bladder control.
sundown, perseverate, confabulate, aphasia, apraxia, agnosia
(repetitive verbalization or motions due to cognitive disturbance)
perseverate
make repetitive verbalizations or motions due to cognitive disturbances
confabulate
To create fabricated or distorted memories.
agnosia/ apraxia
inability to recognize objects, even though sensory ability is intact
inability to perform motor activities even though physical ability remains intact
severe Alzheimer
many cognitive losses: diff communicating, responding to environment, controlling movement
behaviors uncorrelated w/ personality
agraphia, hyper metamorphosis, hyperorality
continuous monitoring, vulnerable to infections
respite care and palliative care
+ help w/ ADL
frontotemporal degeneration dementia (Pick’s disease)
Behavioral or language issues
frontotemporal lobe damage
onset or gradual with 3 variants:
disinhibition,
apathy,
inertia,
loss of sympathy/empathy,
perseverative/stereotyped/compulsive/ritualistic behavior, or
hyperorality and dietary changes)
EPS: prominent, with palsy, muscle atrophy, and hallucinations
+decline in social cognition/ language variant, or learning and memory
~genetic tau (MAPT), the granulin gene (GRN), and the CNORF72 gene
+ younger age
CT/MRI
Lewy body disease dementia
fluctuating cognition, recurrent visual hallucinations (women), and spontaneous features of parkinsonism,
REM sleep behavior and severe neuroleptic sensitivity can also be suggestive (men)
tactile hallucination that do not disappear when touched
more impairments of attention, visuospatial abilities, and executive function than Alzheimer
cognitive decline before motor → ends with severe dementia and death
co-occurring w/ Alzheimer and cerebrovascular disease
Parkinson and alzeihmer’s s/s
take pt hx
vascular disease dementia
decreased blood flow to brain (2nd most common after Alzheimer)
decline in attention and frontal- executive function
duration varies
CT/MRI, physical exam, hx of CVA
difficulty clock drawing
TBI dementia
loss of consciousness, posttraumatic amnesia, disorientation, and confusion ← after injury + recovery
can mimic dementia → misdx
due to accidents (fractures present), co-occurring SUD, strangulation (interpersonal/ domestic violence)
more likely for under 4, adolescents, over 65y
SUD dementia
intoxication + withdrawal from substance that can produce neurocognitive impairment = long term
Temporal course of disorder consistent with substance use
alcohol, inhalants, amphetamines, and sedative/hypnotic/anxiolytics. methamphetamine
can increase w/ vascular disease, liver disease, nutritional deficits, cerebrovascular disease, and cardiovascular disease + after age 50y
HIV dementia
depending on HIV status, dementia worsens or betters
unprotected sexual activity, reuse of needles, infected blood products, and iatrogenic factors
prion disease dementia
infected with prion → myoclonus/ataxia
→ Creutzfeldt-Jakob disease (CJD) [bovine spongiform encephalopathy or mad cow disease], kuru, Gerstmann-Staussler-Scheinker syndrome, or fatal insomnia
=s/s = rapidly progresses to anxiety, problems with sleeping or appetite, difficulties with concentration, fatigue, lack of coordination, altered vision, abnormal movements, and progressive dementia (wing beating)
from animals, transplanted corneas, human growth factor injection, or from infected the client to the health care worker
dx w/ biopsy/ autopsy or where livestock or outbreak of madcow
NO CURE/ MED
Parkinson dementia
develop motor manifestations before cognitive
tremors, rigidity, bradykinesia, postural instability, dystonia, vocal manifestations, and gait/walking problems
apathy, depressed mood, delusions, personality changes, anxiety, hallucinations, daytime sleepiness, rapid eye movement, and sleep behavior disorder
herbicides and pesticides or have a history of traumatic brain injury.
Huntington’s disease dementia
insidious onset and gradual progression
cognitive → motor (core first) for 10y or more → difficult to understand → severe chorea (involuntary jerking)
dysarthria, impaired gait, and impulsive/irritable behaviors.
HTT gene in X 4 ( use genetic testing)
comorbidities in dementia
delirium, sleep disorders, epilepsy, oral disease, malnutrition, falls, and visual impairment.
in older adults = chronic obstructive pulmonary disease (COPD), vascular disease, diabetes mellitus
can be caused due to anticholinergics
comorbidities in Alzheimer
CV,
due to confusion → nonadherence to med
eye disease due to poor blood flow = macular degeneration, diabetic retinopathy, and glaucoma
Alzheimer risk factor
age, women (longer lives, pregnancy, low estrogen, genotype)
genetic in polymorphism apolipoprotein E4
Down syndrome, vascular disease, TBI
stress in childhood
Prolonged use of androgen deprivation therapy (ADT) in men
hyperactive or hypoactive delirium
hyperactive delirium where the person becomes overly reactive (agitated and restless),
hypoactive delirium where the client becomes underactive (sleepy, lethargic, or slow to respond). “acute apathy syndrome,”
alzheimer’s disease
ApoE4 (chromosome 19) and chromosome 21 (trisomy 21 or Down syndrome)
tangles of fibers found inside neurons accumulate proteins called tau → amyloid plaques
dementia patient interventions
consistent routines, calm environments, reorient patients w/ seasonal decorations, calendars, and clocks
delirium tests
hormone levels, vitamin levels, electrolytes, thyroid function, glucose, therapeutic drug levels, liver and kidney function, VDRL, HIV, and CBC
urine and blood tests for infection and electrocardiograms (ECG)
determine underlying cause
Alzheimer testing
for Positron emission tomography (PET) amyloid plaques, cortical atrophy, tau predominant neurofibrillary tangles
mini-mental status exam or functional assessment stage tools for stages,
FAST: 16-item: neurologic deficits of perception (such as puzzle-solving), attention span (sustaining an activity), memory (remembering something a few minutes later), emotional control (gauging whether emotions coincide with the situation), and reasoning/judgment (following social conventions and making appropriate decisions).
Stage 1 / 2 functional assessment
1: no change = normal adult
2: trouble w/ words/ location but good ADL = normal ADL
Stage 3 functional assessment
stressful setting → deficit but return when stress ends
may require assistance and monitoring
designate power of attorney
= incipient + possible Alzheimer
Stage 4 functional assessment
requires assistance w/ organizing/ planning, no housework
may abandon hobbies
minimal/ moderate assistance w/ ADL
probably needs power of attorney
=mild Alzheimer
Stage 5 functional assessment
needs prompting and assistance for hygiene/ dressing
inappropriate emotions
moderate assistance w/ ADL
power of attorney is in place
= moderate Alzheimer
Stage 6 functional assessment
must be assisted w/ dressing and bathing → incontinence,
moderate to total care/ monitor
moderately severe Alzheimer
Stage 7 functional assessment
all s/s worsen. Few words. Total care
severe Alzheimer
Stage 8 functional assessment
not able to hold head, sit, smile
fetal position + immobile
seizure, total care
= severe alzheimer
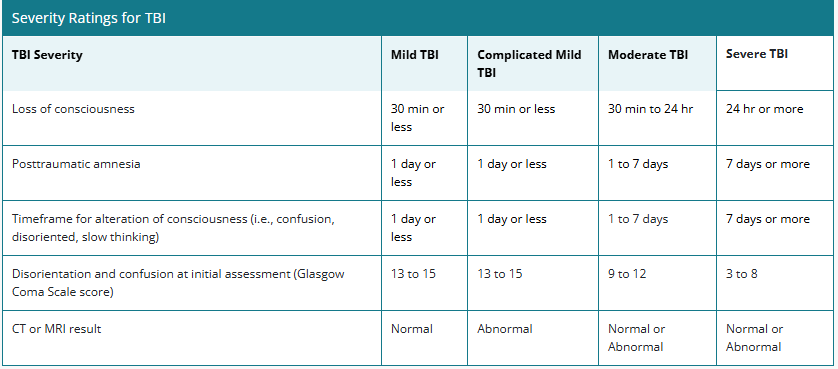
TBI severity
_________ is evident on MRIs of clients who chronically use alcohol.
Cortical thinning
depression
lack of motivation and interest in activities previously enjoyed.
trigger and experience loneliness
Alzheimer diet prevention
Mediterranean diet: fish, fresh vegetables, and plant oils + exercise
MIND: Mediterranean-DASH
Omega 3: fish, flaxseed oil, flaxseeds, nuts, and leafy vegetables
high intake of flavanol-rich foods like olive oil, tea, beans, wine, kale, broccoli, spinach, oranges, tomatoes, and pears
Alzheimer interventions
use hearing aids
reminiscence therapy: build a scrapbook or legacy book to record important events that the client may want to remember
self esteem for clients
music → evoke autobiographical memories
massage therapy (cranial-sacral to improve CSF), face- recognition practice, pet-therapy
monitoring for proper hydration and nutrition, daily exercise
early mobility, families in care, and restricting the use of analgesics or sedatives
when progresses: live at home but may need some assistance with reminders for appointments, wear a location device to prevent getting lost,
high locks but with caregivers present
-—> 24hr facility for supervision
unit enviroment
the safety of the client, to prevent elopement, to minimize sensory stimulation, to make pathways clear, and to facilitate viewing of the client.
minimize mirrors, railings in hallways and grab bars in bathrooms, well-light
minimize the use of restraints and instead use distraction or redirection for clients
Dementia in home
Ensure supervision is appropriate to the stage of illness.+ monitor medication adherence.
Consider placing the bed mattress for fall risk
Contact important people (spouse, children, EMS).
Educate family on the disease, importance of monitoring, and client needs.
Ensure adequate nutrition and hydration.
Ensure hot water and oven safety.
Prevent elopement/place a tracking device on the client.
Notify law enforcement, as needed, of the need for monitoring/chance of wandering.
Evaluate the house for safety hazards (poorly placed furniture, and throw rugs).
Remove smoking materials.
Minimize sensory overstimulation.
Ensure locks and windows are secure.
Install safety rails on hallways, steps, and bathrooms.
Remove sharp objects.
Restrict or forbid the use of the car, and arrange transportation services as needed.
Label rooms and drawers.
Explore installing sensor devices and web-based GPS systems/bed monitors.
Consider meal delivery/home health aides/home health services/respite services as needed.
Encourage activities the client enjoys and can perform well.
patient education
teach family and pt about disease: Printed handouts,
teach delirium abut self-limiting nature of disorder
Peplau: stated that the relationship between the nurse and the client is essential (therapeutic presence)
dementia take redirection well, so using distraction and anticipating the client’s needs are important to communicate empathy.
Reminiscence therapy
reinforce reality
The nurse must always assess for safety, depression, and suicidality, as well as signs of cognitive dysfunction
delirium assess
alert for manifestations of irritability, confusion, hyperactivity, trembling, tachycardia, sweating, tremors, nausea, vomiting, impaired consciousness, seizures, and hallucinations (visual, auditory, and tactile).
herbs
Buckwheat honey → potential source of cholinesterase inhibition
Lemon, rosemary, and lavender essential oils → sleep, cognitive function, and memory and decrease anxiety, agitation, aggression, and psychotic manifestation
meds for s/s Alzheimer
Mild to moderate stage: cholinesterase inhibitors (donepezil, tacrine, rivastigmine, and galantamine)
Moderate to severe stage: IV-methyl-d-aspartate antagonist memantine and combination of memantine hydrochloride extended release and donepezil hydrochloride
meds for disease progression
aducanumab: reduce amyloid beta plaques for early stage