Pharmacology Pt. 1 Cardiac Drugs
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
36 Terms
What are the 2 categories of cardiac drugs?
antiarrhythmic + antihypertensives
only antihypertensives
What are the 2 types of antiarrhythmic and antihypertensive drugs?
What is the main function?
B blockers
Ca channel blockers
decrease the heart rate bc they affect the rhythm of the heart + also decrease blood pressure
What are the 3 types of only antihypertensive drugs?
What is the main function?
diuretics
ACE inhibitors
ARB blockers
only decreasing the blood pressure
What category are beta blockers and what is the suffix to remember?
What is the mechanism of action? (don’t necessarily need to know for NPTE but it will help us to connect the dots)
So what is the effect of beta blockers?
What patients would you NOT give beta blockers to?
beta blockers = anti-arrhythmic + antihypertensive = “-olol”
“lol” = we block when someone is LOL at us
mechanism
block the beta-adrenergic receptors, block the action of the sympathetic NS
SNS increases HR and BP, vasoconstriction, and bronchodilation = fight/flight response
effects
decrease HR and BP, bronchoconstriction, vasodilation
DO NOT give to patients with pulmonary conditions like COPD, asthma, because we don’t want the bronchioles to constrict
What are 3 indications for giving a patient beta blockers?
What are 6 adverse affects related to BP, head feeling, noises, HR
What ECG findings would you see?
indications
to reduce HR: arrhythmias, coronary artery disease (CAD), HTN
adverse effects
orthostatic hypotension, dizziness, lightheadedness, ringing of the ears, venous pooling (vascular system/veins are dilated and bloods are getting accumulated in the LEs and unable to pump back to the heart), bradycardia
ECG findings
PR interval increases (time taken for impulse from atria to ventricle) because this prolongs when the HR is reduced
What are 3 considerations for patients using beta blockers?
use RPE for exercise prescription
do NOT use in asthma, COPD
no abrupt withdrawal
Preload is end diastolic volume which means what?
recall which mechanism that works at the end of diastole?
end diastolic volume
the amount of blood in the ventricles at the end of diastole
frank sterling mechanism
when the ventricles are filled, the more stretch the ventricles have so the force of contraction is stronger
if we have a good preload, the force of contraction is good —> good cardiac output
What does afterload mean?
afterload
resistance the heart needs to overcome
if there is atherosclerosis/plaque deposition, there will not be good cardiac output and there is more afterload/resistance
it is hard for the heart to pump
we need a low afterload to have a good cardiac output
So what would we want for a good cardiac output?
And what happens to pre/after load with beta blockers?
good CO
good/normal preload, reduced after load
beta blockers slightly or do not reduce the preload, but they do reduce afterload, so it is good/beneficial for us
What category are calcium channel blockers for and what is the suffix(ces) to remember? Give three examples.
What is the mechanism?
What are the effects?
Compare it with beta blockers.
calcium channel blockers = antiarrhythmic + antihypertensive = “-Pines and -Zems” - CA has pine trees and zem(n) people
amlodipine
verapamil
diltiazem
mechanism
typically, Calcium is for Contraction; calcium deposits constrict in the arteries
so Ca blockers will block the entry of calcium in cardiac tissue, thereby reducing cardiac contractility and vasoconstriction
effects
decrease HR, decrease BP
it is similar to beta blockers, but calcium channel blockers DO NOT cause bronchoconstriction, so we can give it to patients with pulmonary conditions
Like beta blockers, what are the indications and adverse effects for patients using calcium channel blockers?
Consideration?
But what is the ECG change?
indications
CAD, HTN, arrhythmia
adverse effects
orthostatic hypotension, dizziness, lightheadedness, venous pooling, bradycardia, ringing of the ears
consideration
use RPE for exercise prescription
ECG change
prolonged QT interval
ventricular depolarization = QRS complex + T wave
entire contraction; since contraction is reduced, QT is prolonged
CA has pine trees, zen people, and QTs
Practice Question 1
A patient is taking B blockers for three years post myocardial infarction. Which of the following is the MOST LIKELY response to exercise seen in this patient?
A. Rapid increase in HR
B. Decreased exercise tolerance
C. Blunted response of HR with exercise
D. Increased BP
C. Blunted response of HR with exercise
RATIONALE: B blockers reduces HR, BP and improves exercise tolerance. Patient will show a blunted response to exercise; blunted = slow response
Recall the 3 only antihypertensives
Main function?
What are shared common characteristics for the effects of antihypertensives?
diuretics
ACE inhibitors
ARB blockers
ONLY REDUCE BLOOD PRESSURE, NOT HEART RATE
will be given for same function, HTN, CHF; reduce preload and after load
Which category are diuretics and what are 3 types of diuretics?
What is the mnemonic/suffix to remember?
diuretics = only antihypertensives
loop diuretics
potassium sparing diuretics
thiazides
di-uretics, -ides
Around the kidney tubule, recall there are small groups of nerve endings/blood vessels in capillaries.
It goes from the glomerulus, to proximal convoluted tubule, to loop of Henle, to distal convoluted tubule.
Where do loop diuretics act on?
What does this mean?
So, what are 4 indications to use loop diuretics?
usually, some water and electrolytes are re-absorbed into the body at the loop of Henle, but loop diuretics act on the loop of Henle
if loop diuretics act on the loop of Henle, this means they prohibit the reabsorption, then there is no water or electrolytes, they are flushed/excreted
LOOP diuretics = LOOP of HENLE
use
HTN, CHF, edema, pulmonary edema
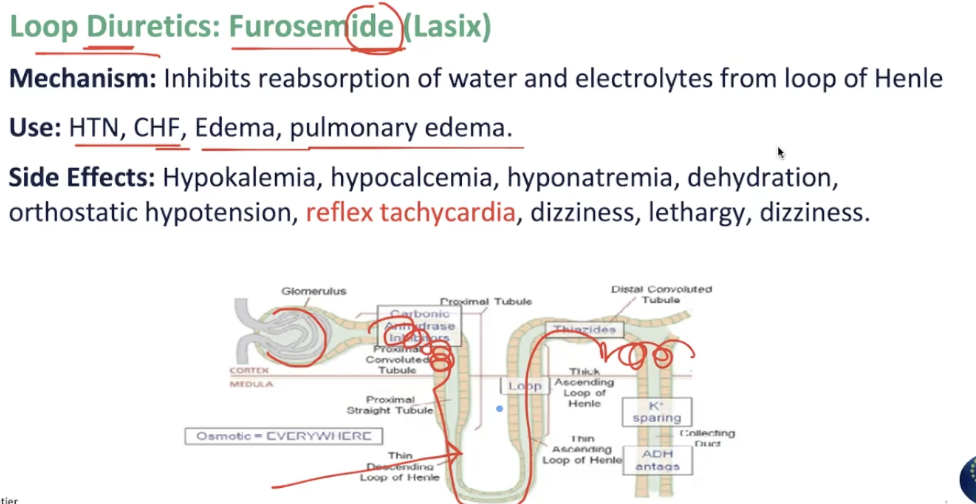
What are side effects for a patient using loop diuretics?
Which one is important when you take a lot of it?
Which side effect from B/Ca blockers would you not see in loop diuretics?
hypokalemia
hypocalcemia
hyponatremia
dehydration
OH, dizziness, lethargy - due to decrease in blood pressure
reflex tachycardia
although HR is not affected, when the BP decreases, the heart will response by reflexively increasing
will NOT see venous pooling, because all of the fluid is able to be flushed out
If the fluid is being excreted, what happens to preload and after load for someone with diuretics?
Which patients would you want this in?
both will decrease
need this in patients with congestive heart failure (CHF) because the heart is failing and they do not have much strength to have a large preload
we want to reduce the load on the heart
What is a type of potassium-sparing diuretic?
Think of how the mechanism is similar AND different from loop diuretics.
What are the side effects?
Used in which patients? (3) and do not have a lot of what?
potassium-sparing diuretic
Spironolactone (Aldactone)
mechanism
similar to loop diuretics, but acts on the distal convoluted renal tubule
does NOT collect potassium , so potassium stays in the body
side effects
similar to others (OH, dizziness, etc.) but + hyperkalemia, gynecomastia (anti-androgen)
use
CHF, HTN, combined with other drugs causing hypokalemia
use this specifically if the patient already has low potassium - should not take loop diuretics
do not give them bananas
What is a type of thiazide?
What mnemonic is important to memorize to know what 4 ions are spared?
Knowing this, in addition to regular antihypertensive side effects like dizziness, ringing of ears, OH, hypoKAlemia and hypoNAtremia, what are other side effects?
So who should this be avoided in?
thiazide = antihypertensive - HTN, CHF, edema
hydrochlorothiazide (HCT)
ions
CLUG - calcium, lipids, urea, glucose
side effects
similar +
hypercalcemia, hyperuricemia, hyperlipidemia, hyperglycemia
avoid use:
elderly, DM, renal dysfunction, hyperlipidemia, gout (uric acid), kidney

What category are ACE inhibitors and what is the suffix to remember?
Typically, what is the normal mechanism of the liver/angiotensin/aldosterone?
What is the normal function of aldosterone?
ACE inhibitors = antihypertensives = “-Prils” - A-pril
liver produces angiotensinogen —> angiotensin I —> lungs / angiotensin converting enzyme (ACE) —> angiotensin II —> adrenals —> aldosterone
aldosterone
retains Na and water, kicks out K
If ACE in the lungs are responsible for converting angiotensin, what would happen if a person takes ACE inhibitors?
What would happen with aldosterone?
How does this affect the side effects?
if ACE is prohibited, there cannot be conversion from I to II, there is no angiotensin II produced
without angiotensin II, then aldosterone will not be produced
if aldosterone is not produced, then there will be a lot of potassium and not enough sodium and water
hyponatremia, dehydration
hyperkalemia
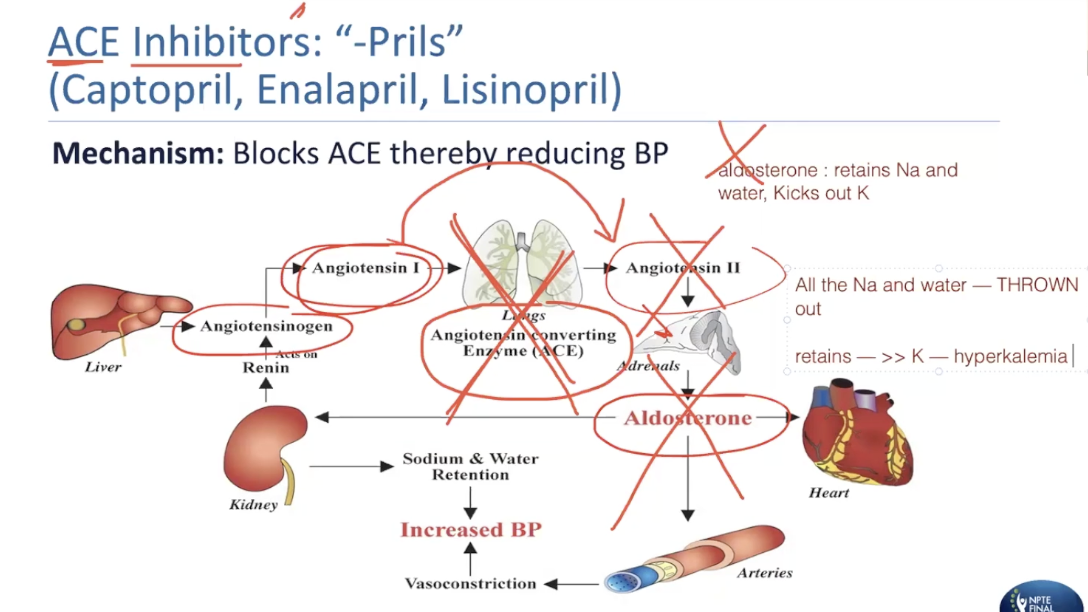
What patients would you give ACE inhibitors to?
In addition to OH, dizziness/lightheadedness, ringing in the ear, blurred vision, what other side effects would there be?
What is the most important symptom?
CHF, HTN, pulmonary edema, edema, taken orally
side effects
hyperkalemia, hyponatremia
dry hacking cough
spring season —> allergies —> dry cough = april
decreased taste perception
angioedema
swelling/fluid in the mucous membranes (lips, under skin)
What is the category for ARB blockers and what is the suffix to remember?
What is the mechanism of ARB blockers?
Therefore, what are the side effects?
Why would you use this over ACE inhibitors?
angiotensin RECEPTOR blocker = antihypertensive = SARTANS
Losartan, Telmisartan, Candesartan
mechanism
blocks the binding of the angiotensin to the receptor, so aldosterone will NOT be produced
same thing will happen as ACE inhibitors - will throw out all of the fluid/water/sodium
side effects
OH, dizziness, fatigue, hyperkalemia but there is NO dry hacking cough
use
HTN, CHF
intolerance to ACE
Can you combine the use of ACE inhibitors and ARB blockers?
What is another drug you cannot combine with?
NO, using ACE + ARB would cause too much dehydration and too much potassium
cannot combine with potassium sparing diuretic
hyperkalemia
ACE + ARB will NOT have reflex tachycardia, but both will reduce blood pressure and increase potassium
Practice Question 2
The physical therapist is educating a patient on the potential side effects from the medication Ramipril. Which of the following side effects will MOST LIKELY correlate with this drug?
A. Increased fluid retention
B. Causes hyperkalemia
C. Increases blood Pressure
D. Enhanced myocardial contractility
B. Causes hyperkalemia
RATIONALE: Ramipril is an ACE inhibitor. It reduces BP, does not affect the HR. It causes hyperkalemia and not Hypokalemia. It decreased fluid retention.
Practice Question 3
The physical therapist is educating a patient on the potential side effects from the medication Candesartan. Which of the following side effects will MOST LIKELY correlate with this drug?
A. Hypokalemia
B. Dry hacking cough
C. Hypotension
D. Prevents the recurrence of atrial fibrillation
C. Hypotension
RATIONALE: Candesartan is an ARB blocker. It reduces BP, reduces fluid retention, does not affect the HR. It causes hyperkalemia and not Hypokalemia. Dry hacking cough is a side effect of ACE inhibitors.
How could you remember cardiac glucosides? What’s an example?
What patients would you use this for? When exactly would this be implemented for the pt?
cardiac glucosides = digs, oxin - Digitalis, Digitoxin, Digoxin (Lanoxin)
used for CHF
systolic dysfunction = ventricles are not contracting forcefully, do not have the power to contract well
decreased ejection fraction <55%
used especially when patient demonstrates acute signs of decompensation
R side
fluid retention, edema, cyanosis, weight gain, JVD
L side
pulmonary edema, lung compensation
What is the function of cardiac glucosides/digoxin? (2)
ECG change?
End result?
Would a patient be using this drug long term?
function
slows down the HR, allowing better filling of blood
increases the strength of the contraction —> increases CO
ECG change
prolonged PR interval, shortened QT interval
reduced HR, increased contractility
fewer + better contractions/beats
only a SHORT TERM DRUG because the side effects are a lot more than the benefits of the drug
What are the side effects of cardiac glycosides/digitoxin/lanoxin?
How long would you use this for?
Understand those symptoms as if you think that something is wrong with the heart. (3) Think of toxic symptoms. (2) And cognitive (4).
And which common symptom we’ve seen?
DIGOXIN TOXICITY
only a SHORT TERM DRUG because the side effects are a lot more than the benefits of the drug
JUST USE WHEN THEY SHOW S/S ACUTE DECOMPENSATION
not long term with compensated heart failure
compensated = no acute s/s, pt is taking regular medication, low CO
would give compensated heart failure patients diuretics, ACE, ARB
arrhythmia, palpitations, fatigue
GI disturbances - N/V
visual disturbance, confusion, delirium, hallucinations
hyperkalemia
Practice Question 4
A patient with congestive heart failure is taking Digoxin since the last few weeks. Which of the following is an EXCEPTION to common side effects of digoxin toxicity?
A. Disorientation and delirium
B. Ringing in the ears
C. Fatigue and palpitations
D. Gastrointestinal disturbances
B. Ringing in the ears
RATIONALE: Ringing in the ears is due to Hypotension. A,C and D are side effects of Digoxin.
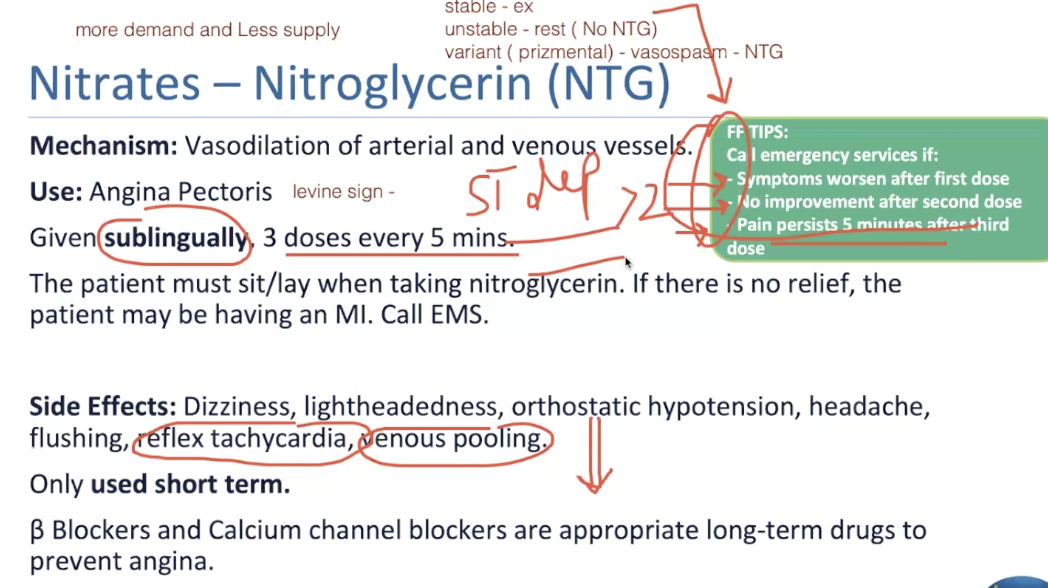
The LAST cardiac drug is nitrates, what is an example?
When is this used for? Explain why the patient would be experiencing that symptom.
nitrates = nitroglycerin (NTG) , nitrostat, nitroglyceride
use
stable angina - chest pain (Levine sign, when they grab their chest)
experiencing angina due to more demand and less supply of blood
Differentiate stable and unstable angina and variant/prizmental angina.
stable angina
occurs with exercise, works with nitroglyceride
heart’s demand is a lot more but not getting supply of demand
unstable angina
occurs at rest, does NOT work with nitroglyceride
variant/prizmental
vasospasm of arteries, works with nitroglyceride
Mechanism of nitrates: If you do not have enough blood supply to the heart, what is the purpose of nitroglycerides? What is the effect on HR and other side effects?
Since there is a drastic decrease in blood pressure, what other side effects would appear? (2)
How often would nitrates be used?
vasodilation of all vessels - arterial and venous
to allow for supply to increase
causes a decrease in BP —> OH, dizziness, venous pooling because of vasodilation
facial flushing - vasodilation
reflex tachycardia - due to drop in BP/vasodilation for heart to compensate
SHORT TERM when you have an acute episode
How are nitroglycerides taken?
How often?
What is the position the patient should be in when taking the drug?
When is it an emergency?
sublingually - under the tongue bc it gets absorbed fast
1 dose every 5 mins x3
patient must SIT/LAY when taking nitroglycerin because they can collapse with decrease in BP
if there is no relief or you feel worse after taking the drug, CALL EMS BC PT MAY BE HAVING AN MI
FF TIPS for when to call 911 after patient is taking nitroglyceride:
first, second, third dose
symptoms worsen after first dose
no improvement after second dose
pain persists 5 minutes after third dose
because if they are not getting better, the patient is experiencing UNstable angina and may go into MI
if going through ischemia/MI, the ECG will appear as ST depression >2mm
Practice Question 5
A patient with angina pectoris has been advised to use sublingual nitroglycerin for stable angina. This drug will MOST LIKELY cause which of the following?
A. Lower preload and afterload
B. Increase myocardial oxygen demand
C. Increase preload and afterload
D. Hypertension and bradycardia
A. Lower preload and afterload
RATIONALE: Nitroglycerin (NTG) decreases Preload and afterload, decreases myocardial oxygen demand. The side effects are hypotension and tachycardia and not hypertension and bradycardia.
vasodilation = less blood coming back to heart, decreased preload + less pressure of the heart, decreased afterload
that’s why we give it before exercise