Why Is This Patient Restricted? and Pleural Disease Discussion
1/17
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
18 Terms
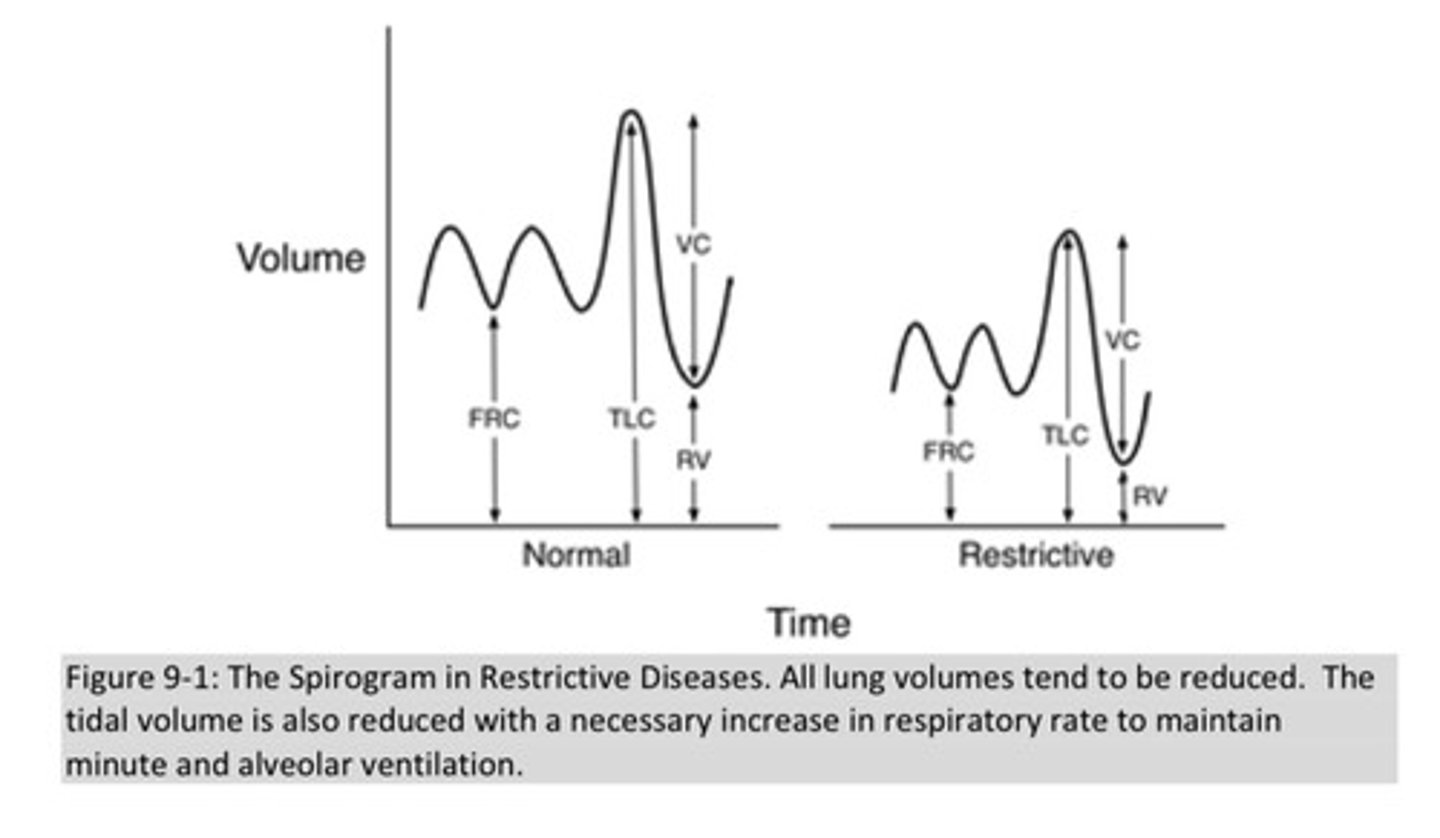
what is the characteristic finding of restrictive lung disease on a spirogram?
restrictive processes are defined by a reduced total lung capacity and are usually accompanied by proportionate reduction in the other subdividison of lung volume, including vital capacity
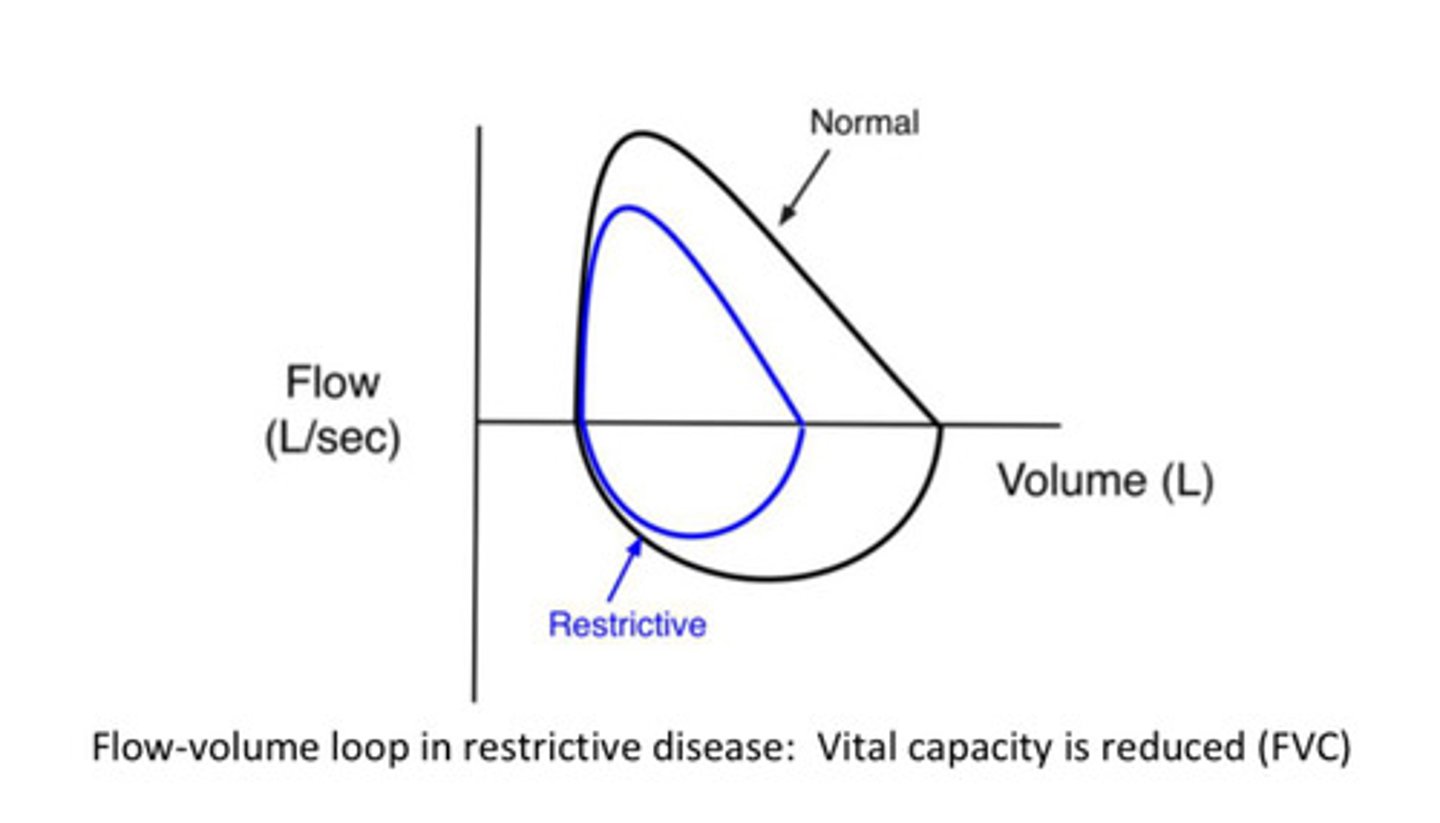
what do we see on a flow volume loop in restrictive lung disease
FVC is reduced
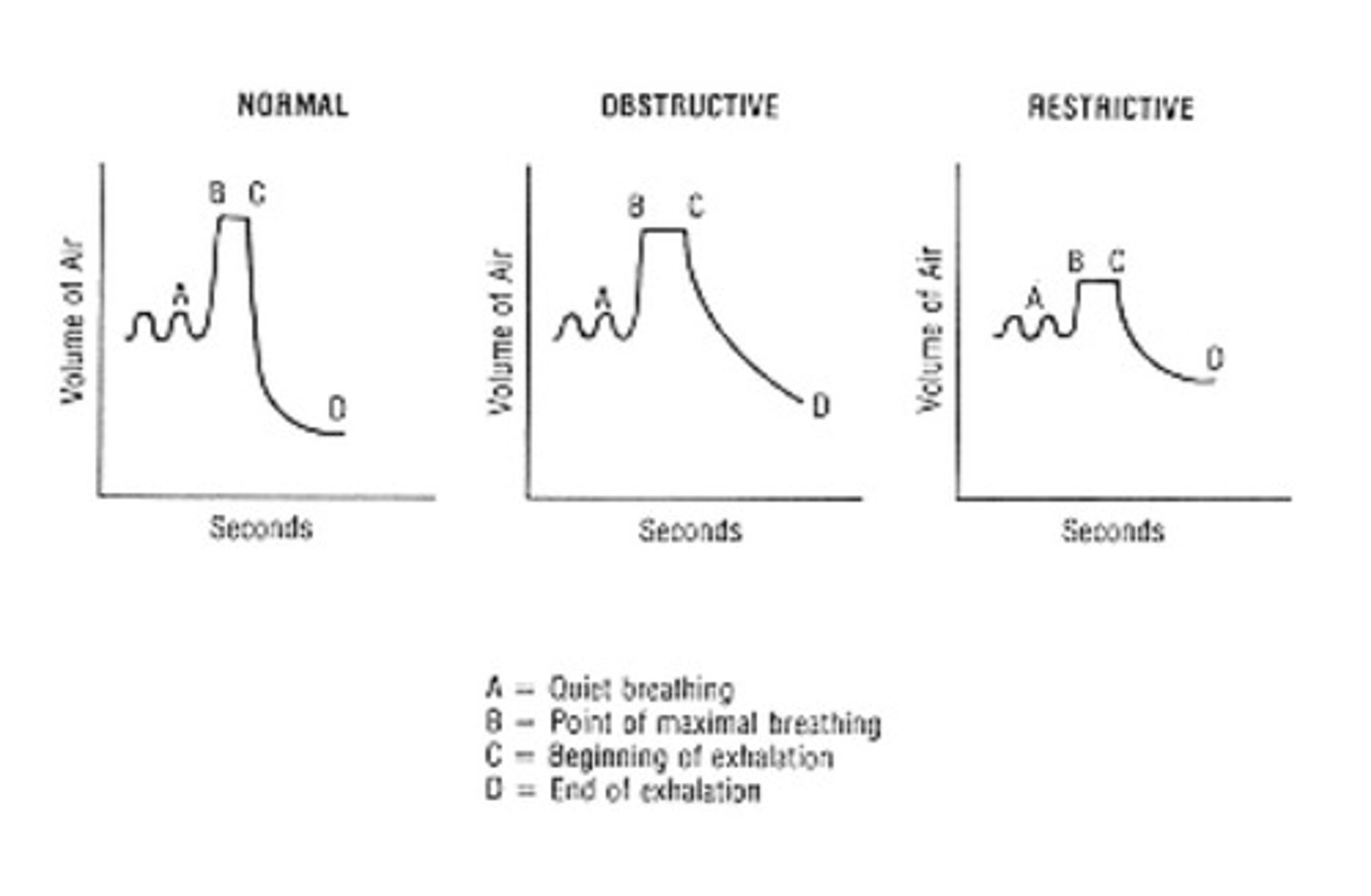
compare the typical PFTs of obstructive to restrictive pulmonary disease
obstructive: FEV1/FVC < 70%
restrictive: volumes are decreased (TLC, FRC, and RV); they may have normal VC and FEV1/FVC
what are the 3 categories of restrictive lung disease? what is an example of each?
1) a lung parenchymal process that decreases compliance of the lung: DPLD (diffuse parenchymal lung disease) —> there are many diseases under the category of DPLD - also called interstitial lung disease (ILD). one subtype involves exposures to toxic substances like asbestos, silica, beryllium as well as exposures to anti cancer medications and radiation. another subtype are pulmonary manifestations of systemic diseases like SLE (lupus), sarcoidosis, and RA (rheumatoid arthritis). the last subtype of DPLDs is idiopathic such as pulmonary fibrosis
2) neuromuscular defect restricting inspiratory effort —> ALS, myasthenia gravis, spinal cord injury
3) chest wall/pleura space problem that limits lung expansion —> scoliosis, pulmonary effusion, extreme obesity
what looks abnormal in this chest xray?
1) lung fields are small (should normally occupy the space of 8-10 ribs)
2) lung fields are dense: this is usually described as "diffuse bilateral reticular opacities" (net-like) and is seen throughout the lungs, but denser at the bases compared with the apices
3) "hilar prominence" meaning that hilar areas are denser, especially on the right. this is likely from enlarged lymph nodes
4) heart is pushed upward; overlaying lymphadenopathy

what is the prognosis of restrictive lung disease for each category
1) for DPLD category: many many causes. some people can halt progression and even go into remission if they can avoid whatever initially triggered the process, some people have unrelenting progression regardless of all interventions. pulmonary arterial hypertension and right heart failure develops in some patients. there are some new anti fibrotic medications, but they do not work for everyone. some pts require lung transplant as only option
2) neuromuscular: prognosis depends on modulating the neuromuscular disease; much effort is made to preserve respiration
3) chest wall: if cause can be removed or reversed (such as weight loss in obesity), prognosis is excellent as lung tissue itself is not damaged
what is a pneumothorax and what can it originate from
a collection of air in the pleural space between the chest wall and the lung. it can originate from a penetration on the chest wall side, such as a stabbing or a broken rib, or from a rupturing of an area of lung, usually a "bleb" or cystic air space. it is typically very uncomfortable and causes shortness of breath.
what is a pneumothorax that occurs without warning? who might this affect, who is it primary in and who is it secondary in?
"spontaneous pneumothorax" and can be "primary" such as in a male in his teens with no underlying lung disease or "secondary" such as in emphysematous COPD
what is a pleural effusion
an abnormal collection of fluid in the pleural space. the normal amount of healthy pleural fluid is less than 15 cc. an effusion is a volume greater than this.
what can the excess fluid in a pleural effusion be from
excess fluid can be comprised of many substances, including pus from infection, serous effusion which can either be transudative or exudative, blood (hemothorax), or lymph (chylothorax)
what 2 things does the effect of the pleural effusion depend on?
1) whether it is acute or chronic
2) the volume
what is thoracentesis
a procedure in which a hollow-bore needle is placed into the pleural space for the purpose of decompression or drainage of the pneumothorax or pleural effusion
what is a chest tube
a tube that is placed in the pleural space to drain a pneumothorax or pleural effusion when a longer-term solution is needed over simply the needle thoracentesis
use this case for the following questions
a 60 year old presents to the ER with chest pain, shortness of breath, and mild cough. pt gets a thorough work up, and his CXR shows this

what do you see? what could we do next to figure out the cause?
1) pleural effusion on the right is clear with the meniscus seen in the radio-opaque area —> could perform thoracentesis to sample a fluid to give us some clues
2) blunting of the costophrenic angles as well; should usually be sharp as her left side; looks more like the image attached

we perform a thoracentesis. if we find serous fluid (as opposed to blood), it can either be a transudate or an exudate. what is a transudate and what are likely causes?
transudate: a "thin" fluid with a low amount of protein, low specific gravity, low number of cells in it; transudate pleural effusions are associated with congestive heart failure, cirrhosis (fibrosis of the liver), and nephrotic syndrome (a severe kidney syndrome in which the kidneys allow important proteins, esp albumin, to leak out of th body in urine, so these pts have low serum protein)
what is an exudate and what are some causes
exudate: a fluid with more protein, higher specific gravity, and sometimes containing cells and other substances. sometimes pus is considered to be in the category of an exudate. the constitution of the exudate helps give clues to the underlying process. for instance, if bacteria are seen in it, the cause is likely pneumonia or infection. people with TB, for instance, often have exudative pulmonary effusions with mycobacteria in them. if malignant cells are seen in it, the cause is likely cancer. there are many other causes of exudative pleural effusion, but these are the most common
what is the likely cause if the fluid we retrieve is filled with leukocytes, dead WBC, bacteria, and tissue debris, otherwise known as pus?
this is typically indicative of a local infection and possible abscess