WBC 14 study document
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
32 Terms
Introduction to White Blood Cell (WBC) and Lymphoid Disorders
White blood cells (WBCs) are central to the immune system. Disorders of WBCs can be: • Benign (reactive): transient changes due to infection, inflammation, etc. • Malignant (neoplastic): uncontrolled proliferation of blood cell lines (e.g., leukemia, lymphoma). WBCs include: • Granulocytes: neutrophils, eosinophils, basophils • Mononuclear cells: lymphocytes (T, B, NK) and monocytes Organs involved: Bone marrow, lymph nodes, spleen, thymus.
2. Neutrophils – Structure, Maturation & Function
Normal Count: • Total WBC: 6,000–11,000 / mm³ • Neutrophils: about 2/3 of total WBCs Maturation Stages: • Myeloblast → Promyelocyte → Myelocyte → Metamyelocyte → Band Cell → Mature Neutrophil (aka PMN = Polymorphonuclear neutrophil) Production & Lifespan: • Produced in red bone marrow • Sequestered partly in spleen • Circulate briefly (6–10 hrs), migrate to tissues, survive 1–2 days Lysosomal Constituents: • Primary (Azurophilic): Myeloperoxidase, Lysozyme, Acid hydrolases • Secondary (Specific): Alkaline phosphatase, Lactoferrin, Lysozyme, Collagenase Key Functions: • Margination → Rolling → Adhesion → Diapedesis → Chemotaxis → Phagocytosis • Balance with splenic pool is important
3. Neutrophil Disorders
Pelger-Huet Anomaly: • Genetic (can be acquired = pseudo-PHA) • Neutrophils appear as bands (hyposegmented nuclei) • Benign, incidental finding Chediak-Higashi Syndrome: • Genetic disorder with large neutrophil granules • Impaired bacterial digestion • Associated with pigmentary issues, bleeding • Serious, especially in children
Leukopenia / Neutropenia
Neutropenia (or Agranulocytosis) = low neutrophil count Danger Zone: • <1000/mm³ = risk • <500/mm³ = life-threatening infections likely Causes: 1. Inadequate Production: • Stem cell failure (e.g., aplastic anemia) • Drugs: chemotherapy, antibiotics, thio-uracil, etc. • Megaloblastic or myelodysplastic syndromes • Congenital: Kostmann syndrome • Bone marrow shows granulocytic hypoplasia 2. Increased Destruction: • Immune-mediated: SLE, drug-induced • Splenic sequestration (hypersplenism) • Infections with high demand (esp. fungal) • Bone marrow shows hyperplasia
Leukocytosis and WBC Differentials
Leukocytosis = elevated WBC count Factors that affect it: • Bone marrow reserve • Splenic pool • Marginating pool • Cytokines (e.g., IL-1, TNF) stimulate WBC production via CSFs Neutrophilia: • Common in bacterial infections, tissue necrosis (MI) • “Left shift” = increase in immature forms • Döhle bodies and toxic granules present Eosinophilia: • Causes: Allergies (esp. drugs), Parasites Basophilia: • Rare • Associated with myeloproliferative disorders Monocytosis: • Causes: TB, SBE, rickettsia, malaria, SLE, IBD Lymphocytosis: • Viral infections: EBV, CMV, Hep A • Whooping cough (pertussis) • TB
Myeloproliferative Disorders (MPDs)
Also called chronic MPDs, because they often span years. Shared Characteristics: • Involve clonal proliferation of myeloid stem cells • Affect multiple blood cell lines • Hypercellular bone marrow, often with extramedullary hematopoiesis (e.g., spleen, liver) • Risk of transformation to acute leukemia • Include: o Chronic Myelogenous Leukemia (CML) o Polycythemia Vera (PV) o Essential Thrombocytosis (ET) o Primary Myelofibrosis (PMF)
Chronic Myelogenous Leukemia (CML)
• Affects adults • 90% have Philadelphia chromosome: t(9;22) → BCR-ABL fusion gene (constitutive tyrosine kinase) Features: • WBC >50,000/mm³, sometimes >100,000 • Left shift in neutrophils, but <10% blasts • Marked splenomegaly • Bone marrow: 100% cellularity • Can evolve into blast crisis (resembles AML) Treatment: • Tyrosine kinase inhibitors (e.g., Imatinib) → ~90% remission
Polycythemia Vera (PV)
All 3 cell lines increased, not just RBCs • Increased marrow activity → high turnover → ↑ uric acid → gout • Platelets are abnormal → both bleeding and thrombosis risks Complications: • May progress to myelofibrosis • No blast crisis like CML
Essential Thrombocytosis (ET)
Platelets >1 million/mm³ • Marrow: megakaryocytic hyperplasia • Platelets are often giant and dysfunctional • Rare and diagnosis of exclusion
Primary Myelofibrosis (PMF)
• Marrow fibrosis with extensive extramedullary hematopoiesis • Occurs in older adults (>60 yrs) • May follow other MPDs • Blood: leukoerythroblastic picture • ~20% may transform into AML
General Features of Leukemias
• Malignant proliferation of WBC precursors in bone marrow • Replace normal marrow → anemia, thrombocytopenia, neutropenia • Acute leukemias suppress hematopoiesis more than chronic • Classified as: o Acute vs. Chronic o Myeloid vs. Lymphoid • Associated with genetic changes, chromosomal translocations
Acute Lymphoblastic Leukemia (ALL)
• Mostly in children • Derived from lymphoblasts (T or B lineage) • Symptoms: Fatigue, fever, bleeding, bone pain, hepatosplenomegaly, lymphadenopathy, CNS signs • Frequently has chromosomal abnormalities (e.g., t(12;21), hyperploidy, sometimes Philadelphia chromosome) • Excellent chemo response: o ~90% remission o ~75% cure in kids
Chronic Lymphocytic Leukemia (CLL)
• Most common adult leukemia • Persistent lymphocytosis > 4,000/mm³ for months • Lymphocytes appear mature, not blasts • No need for bone marrow biopsy for diagnosis • Progression involves marrow, lymph nodes, liver Special Features: • Hypogammaglobulinemia • ~15% have autoimmune hemolytic anemia or thrombocytopenia • Related to small lymphocytic lymphoma (SLL)
Acute Myeloid Leukemia (AML)
• Seen in adults and elderly • Diagnosis: >20% blasts in marrow or blood • Subtypes: M0 to M7 (FAB classification)
FAB Type Description
FAB Type Description Key Features M0 M1 M2 M3 M4 M5 M6 M7 Minimally differentiated Without maturation With maturation Rare Auer rods rare Auer rods common Acute Promyelocytic Leukemia (APL) Risk of DIC, treat with ATRA Myelomonocytic (AMML) Monocytic Erythroleukemia Megakaryocytic Prognosis: • ~60% initial remission • Only ~20% 5-year survival • Worse than ALL Common Gum infiltration Rare Rare
Myelodysplastic Syndromes (MDS)
• Pre-leukemic conditions • Ineffective hematopoiesis → cytopenias • Marrow: dysplasia, ringed sideroblasts, nuclear budding • <20% blasts (otherwise → AML) • Can be spontaneous or drug-induced (even years later) • ~25% progress to AML
Multiple Myeloma & Related Plasma Cell Disorders
• Malignant proliferation of plasma cells in bone marrow. • Typically associated with monoclonal gammopathy.Key Features: • Bone marrow: >20% plasma cells (sheets) • Bone destruction → lytic lesions, pathologic fractures • Secretes IgG > IgA most commonly • Bence-Jones protein: light chains in urine • Elevated IL-6 is a bad prognostic marker Symptoms: • Bone pain, anemia, recurrent infections (Staph, Strep) • Hypercalcemia, renal failure, amyloidosis, bleeding Diagnostic Clues: • “Cartwheel” or “clockface” nuclear chromatin • “Hoff” or prominent Golgi zone • Monoclonal spike (M spike) on serum protein electrophoresis (SPEP) • Skull X-rays: lytic “punched-out” lesions
Other Related Disorders:
Solitary Plasmacytoma: • Localized plasma cell tumor • Nearly always progresses to multiple myeloma MGUS (Monoclonal Gammopathy of Undetermined Significance): • Asymptomatic monoclonal protein • No bone lesions, normal renal function • May evolve into MM at ~1%/year Waldenström's Macroglobulinemia: • IgM monoclonal gammopathy → hyperviscosity • Associated with lymphoplasmacytic lymphoma Heavy Chain Disease: • Rare; affects Ig heavy chains • Seen in some lymphomas Amyloidosis: • Light chains (AL type) accumulate • Can follow MM or chronic inflammation
Lymphadenopathy & Lymphadenitis
Definitions: • Lymphadenopathy: Enlarged lymph nodes (tender or non-tender) • Lymphadenitis: Inflammation of lymph nodes Benign Types: Acute: • Often tender • Caused by bacterial or viral infections • Neutrophilic or lymphocytic infiltration Chronic: • Non-tender • Two major patterns: o Follicular hyperplasia: ↑ secondary follicles in cortex o Sinus histiocytosis: prominent medullary sinuses (reticular hyperplasia)
Lymphomas (Malignant Lymphoid Tumors)
General Concepts: • Monoclonal proliferation of lymphocytes (B > T) • Can be nodal or extranodal • Terms: Small/large, follicular/diffuse, cleaved/non-cleaved • Two main categories: o Hodgkin Lymphoma (HL) o Non-Hodgkin Lymphoma (NHL) Key Features: • Normal lymph node architecture is effaced • Genetic rearrangements in antigen receptor genes • Most B-cell derived (~85%), rest T-cell • Staging is essential, especially for HL
Hodgkin Lymphoma (HL)
• Defined by presence of Reed-Sternberg (RS) cells o RS cells: large, bilobed nuclei with prominent nucleoli (“owl eyes”) Subtypes: 1. Nodular Sclerosis – most common, young women, lacunar RS cells 2. Mixed Cellularity – second most common 3. Lymphocyte Rich 4. Lymphocyte Depleted 5. Lymphocyte Predominance – CD15−, CD30−, but CD20+
Staging (Ann Arbor):
• I – one node group • II – >1 node group, same side of diaphragm • III – both sides of diaphragm • IV – extranodal (e.g., liver, marrow) • A – no systemic symptoms • B – fever, weight loss >10%, night sweats
Non-Hodgkin Lymphoma (NHL)
Non-Hodgkin Lymphoma (NHL)
WHO Classification:
B-Cell Origin:
• Precursor B-lymphoblastic lymphoma/leukemia
• Chronic Lymphocytic Leukemia (CLL)/Small Lymphocytic Lymphoma
• Follicular Lymphoma
• Diffuse Large B-cell Lymphoma
• Burkitt Lymphoma (“starry sky”)
• Mantle Cell, Marginal Zone, Hairy Cell Leukemia
• Plasmacytoma / Multiple Myeloma
T/NK-Cell Origin:
• Precursor T-lymphoblastic lymphoma/leukemia
• Mycosis fungoides / Sézary syndrome (skin involvement)
• Anaplastic large cell lymphoma
• Angioimmunoblastic, Enteropathy-associated
• Adult T-cell leukemia/lymphoma (HTLV-1)
• Extranodal NK/T-cell lymphoma (nasal type)
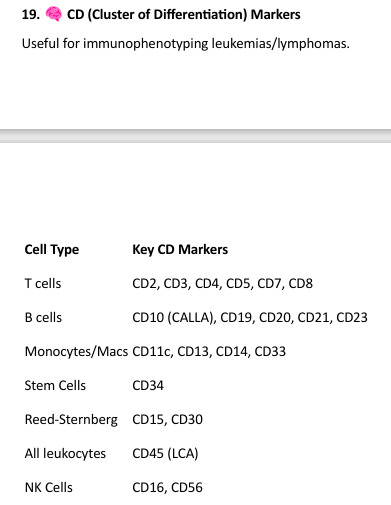
CD (Cluster of Differentiation) Markers
Spleen: Anatomy, Function & Disorders
Anatomy: • Weight: ~150 g • Location: Left upper quadrant (LUQ) • Surfaces: Adjacent to diaphragm, kidney, pancreas, stomach Functions: • Filters aged or damaged RBCs • Secondary immune organ (white pulp) • Phagocytic activity (~15% of body's macrophages) • Can resume hematopoiesis in disease • Blood cell storage (esp. platelets, RBCs)
Splenomegaly
Enlargement of the spleen, causes: 1. Congestive: • Portal hypertension (e.g., cirrhosis) • Right-sided heart failure 2. Infiltrative: • Leukemias, lymphomas, storage diseases (e.g., Gaucher, Niemann-Pick) • Amyloidosis, metastases 3. Infectious: • TB, mononucleosis, malaria, fungal infections 4. Immune-related: • Rheumatoid arthritis, SLE
Hypersplenism
• Triad: Anemia, Leukopenia, Thrombocytopenia • Due to excessive sequestration
Infarct
• Caused by emboli or sickled RBCs • Can result in wedge-shaped necrosis
Primary Splenic Tumors (Rare):
• Hemangioma, lymphangioma • Fibroma, osteoma, chondroma • Lymphoma
Miscellaneous:
• Congenital absence – rare • Accessory spleens – common • Splenic rupture – emergency (can cause massive internal bleeding)
Thymus: Role & Pathology
Function: • Site of T-cell maturation (positive/negative selection) • Prominent in infants; regresses in adulthood • Contains: o Thymocytes (immature T cells) o Epithelial reticular cells o Hassall's corpuscles (unique to thymus)
Thymic Diseases:
1. Hypoplasia/Aplasia: • Seen in DiGeorge syndrome (22q11 deletion) o Congenital absence of thymus o T-cell deficiency → immunodeficiency 2. Cysts: • Incidental, usually asymptomatic 3. Thymomas: • Tumors with both epithelial and lymphoid elements • Can be: o Benign (encapsulated) o Malignant I: Locally invasive o Malignant II: Metastasizing • Often associated with myasthenia gravis