Horse Cardiology
1/88
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
89 Terms
Equipment costs
xray 80K
probes 50K
ultrasound 5-25k
only buy if you have enough money to fund it
Ataxic
In horses, ataxia refers to a lack of voluntary muscle coordination, causing an unsteady or "wobbly" gait.
- Symptoms: Staggering, dragging toes, hindquarter swaying, or crossing limbs when walking.
- Common Causes: Neurological conditions such as Equine Protozoal Myeloencephalitis (EPM), Wobbler Syndrome (Cervical Vertebral Stenotic Myelopathy), or trauma to the spinal cord.
Grades of Ataxia
Definition: Neurological deficits in horses are graded on a scale from 0 to 5:
Grade 0: Normal neurological function.
Grade 1: Subtle deficits only detected during special maneuvers (e.g., backing up, tight circles).
Grade 2: Mild deficits that are visible at a normal walk.
Grade 3: Moderate deficits; incoordination is obvious and the horse may weave or stumble.
Grade 4: Severe deficits; the horse is highly unstable and prone to falling during normal movement.
Grade 5: Recumbent; the horse is unable to stand up
Lameness
horse is unable to walk properly, left foot down gingerly, right foot drag, then hop, limp
Atlas Vertebrae of horse
atlas is the first vertebrae, Its primary function is to protect the spinal cord at the base of the skull and support the head, allowing for a range of motion between the skull and the neck.
Axis Vertebrae of horse
second vertebrae, head side to side, longest vertebra, provides surface for neck muscles and supporting head, protects spinal cord from skull through neck
How blood moves through the heart
1. Deoxygenated blood returns from the body via the vena cava into the Right Atrium.
2.It passes through the tricuspid valve into the Right Ventricle.
3.The right ventricle pumps the blood through the pulmonary valve to the lungs via the pulmonary artery.
4.Oxygenated blood returns from the lungs via pulmonary veins into the Left Atrium.
5.It passes through the mitral valve into the Left Ventricle.
6.The left ventricle pumps the oxygenated blood through the aortic valve into the Aorta to be distributed to the rest of the body.
Pressures in left and right sides
left is high pressure, right is low pressure
What are the chordae tendinae?
anchor the leaflets of the mitral and tricuspid valves to the papillary muscles in the heart ventricles. They prevent the atrioventricular (AV) valves from inverting (prolapsing) into the atria during ventricular contraction (systole), thus preventing blood backflow and ensuring one-way flow
What is a heart murmur?
when the chordae tendinae is loose and causes the heart to make a whooshing noise
What is the one thing that is common for all heart diseases for horses?
exercise intolerance
What is the function of the veins?
The veins are to take away, only one carries oxygenated blood
remove de-oxygenated blood
walls much thinner and less elastic tissue
lower pressure
venous intima folds to form venous valves
venules = veins = vena cava
What do the arteries do?
Arteries deliver oxygenated blood
• High pressure system.
• Aorta and other larger arteries contain a large amount
of elastic tissue.
• Aorta=> Arteries=>Arterioles=>Metarterioles
• Only one artery carries de-oxygenated blood.
Capillaries
• Where the action is!
• In the lungs gas is exchanged.
• In body oxygen and nutrients delivered.
• Junctions between endothelial cells
• Vesicular transport
• Fenestration
• Capillary sphincters
• A-V shunts
A-V shunts
These shunts bypass the capillary network, allowing high-pressure arterial blood to flow directly into low-pressure veins or chambers (right atrium, right ventricle, or coronary sinus)
Vesicular transport
Vesicular transport is a fundamental, ATP-dependent active process in cells where substances move within membrane-bound sacs called vesicles, facilitating cargo delivery between organelles (ER, Golgi, lysosomes) or across the plasma membrane (endocytosis/exocytosis)
endothelial cells
Endothelial cells (ECs) are a thin, specialized layer of cells forming the inner lining of all blood vessels, lymphatic vessels, and the heart, acting as a crucial, dynamic barrier between blood and tissues. They regulate vascular tone, blood flow, nutrient exchange, and immune responses while inhibiting blood clotting. These cells are essential for angiogenesis (forming new vessels) and wound healing.
Fenestration
Fenestrated capillaries are blood vessels with tiny pores (fenestrations or "windows") in their endothelial cells, allowing for rapid filtration and exchange of water, nutrients, hormones, and waste between blood and tissues
Why does the Heart Beat?
• Cardiac Conduction System.
• Sinoatrial node (SA node).
• Internodal atrial pathways.
• Atrioventricular node AV node).
• Bundle of His
• Purkinje system
• All can spontaneously discharge
What is arrhythmia?
An arrhythmia is an irregular, too-fast (tachycardia), or too-slow (bradycardia) heartbeat caused by faulty electrical signals, often described as an "out of sync" or fluttering heart.
Sinoatrial Node
• SA node discharges most rapidly.
• Cardiac pacemaker in right atrium
Internodal atrial pathways
Internodal atrial pathways are specialized routes of conductive heart tissue connecting the SA node (natural pacemaker) to the AV node, ensuring rapid, organized electrical signal spread across the atria for coordinated contraction
Atrioventricular node AV node
The Atrioventricular (AV) Node is a crucial part of the heart's electrical system, acting as a gateway between the atria (upper chambers) and ventricles (lower chambers) to coordinate heartbeats, delaying electrical signals to ensure the atria fully contract and fill the ventricles with blood before the ventricles themselves contract
bundle of HIS
A bundle of specialized heart muscle cells that passes from the AV node into the interventricular septum. It divides into left and right bundle branches to conduct impulses to the apex of the heart.
Purkinje Fibers
A network of specialized fibers that extend from the bundle branches into the subendocardial tissue of the ventricles. They have a very fast conduction rate (approx. 75 milliseconds) to ensure rapid depolarization of the ventricles.
Automatic Nervous System
a component of the peripheral nervous system that regulates involuntary physiological processes, Parasympathetic, enteric (gastrointestinal control), and sympathetic systems
parasympathetic
relaxing system
medulla makes saliva
vagus nerve: slows heartbeat, constricts lungs/bronchii, bile release, bladder contract, stim secretion/peristalsis
sympathetic
fight or flight, active excited, dilates pupil, inhibits saliva, accelerates heart, dilates bronchi, solar plexus: inhibits peristalsis and secretion, liver converts glycogen to glucose, secretion of adrenaline and noradrenaline, inhibits bladder contraction
Sympathetic system in horses digestive system
shuts down the intestines and stomach, feels pain and therefore the horse wants to run or fight
Parasympathetic system in horses
vagus tone makes them drop a beat, cardiovascular function that facilitates adaptive responses to environmental challenge, makes them relax, skip a beat
How to count heart rate in horses?
15 sec x 4
or 30 secs x 2
count how many beats in those seconds and multiply by the additional number
What happens when the horse is scared?
Horses heartbeat can be 80 plus if animal is fearful.
• Horses know who the Vet is.
• Frequently have to take heartbeat last to let animal relax.
What are heart sounds?
Heart sounds are the closing of the cardiac valves.
• Lub is the closing of the mitral and tricuspid valves
(S1).
• Dub is the closing of the aortic and pulmonary valves
(S2).
• S3 is caused by rapid ventricular filling.
• S4 is from atrial contracting to fill ventricle
• In the horse , S4-S1-S2-S3
Electrocardiogram
Electrical activity of cardiac muscle.
Qrs ventricular depolarization (contraction) and is primarily used to diagnose cardiac arrhythmias, conduction abnormalities (like bundle branch blocks), ventricular hypertrophy, myocardial infarction (heart attack), and electrolyte imbalances
electrical system of the heart is the SA
ventricular contract is the qrs, T is where everything depolarizes, relaxes to normal
SA node does what?
makes atrium contract
If you see changes in QRS
likely afib, in humans clogged artery means a part can die and you will see changes in qrs
horse heart attack
not a real attack, but rupture of aortic, blood fills the abdominal cavity, brain shuts down and then death
Myocardial (muscular tissue) not an issue
• Aortic rupture
– Peak athletic exertion.
– Sudden death post race
– No external signs, white mm
Membrane Potential
• Normal resting membrane potential is -70mv
– Cardiac muscle is -90mv
• Na+ actively transported out of cell
• K+ actively transported into cell
• Once threshold is met. Na+ channels open
Muscle Contraction
• Muscle fibers are the building blocks.
• Cell membrane = Sarcolemma with T-tubule system
• Muscle Fiber=>Myofibrils=>Filaments
• Filaments made up of contractile proteins
• Myosin
• Actin
• Tropomysin
• Troponin I, T, C
Myosin
A molecular motor protein that converts chemical energy (ATP) into mechanical energy (force).
Forms thick filaments with heads that bind to actin.
Powers movement by "walking" along actin filaments.
thick filaments
cause contraction, cell division, migration, and intracellular transport
Actin
globular protein that polymerizes to form long, thin filaments.
Contains binding sites for myosin heads.
Key role in cell shape, movement, and division
Once Threshold reached
– Na+ influx
– K+ efflux
– Via the T-tubules the Sarcoplasmic Reticulum releases
Calcium
Tropomysin
Tropomyosin is an actin-binding, rod-shaped coiled-coil protein that regulates muscle contraction and acts as a major regulator of the cytoskeleton in non-muscle cells. In muscles, it blocks myosin-binding sites on actin, preventing contraction until calcium ions trigger a conformational shift
Troponin I, T, and C
Troponin I, T, and C are regulatory proteins within cardiac and skeletal muscle that control contraction
Troponin I, T, and C types
Troponin C (cTnC): Binds calcium ions to initiate muscle contraction. It is not specific to the heart.
Troponin I (cTnI): Inhibits myosin and actin interaction; specifically cardiac-specific, making it highly sensitive for heart muscle damage.
Troponin T (cTnT): Binds the troponin complex to tropomyosin. Primarily found in cardiac muscle, with minor, limited presence elsewhere.
Muscle Contraction
• Release of Calcium starts the contraction
• Calcium binds to Troponin C
• This binding causes tropomyosin to move off of the
actin binding site
• Myosin head then binds to actin.
• Myosin head then bends with ATP.
• Cycle is repeated many times
What is a sarcomere?
a muscle unit with myosin and actin fibers
Cortenary artery
provides blood to the heart muscle
every cell has a capillary that feeds it and takes away waste
horse lying on ground, blood from both nostrils
blood out both nostrils and that violent usually means lungs blew up, or larenx has problems
horse nostril bleeding
1 nostril, doctor did it, accidentally hit their tooth, or rotten tooth
PDA Patent Ductus Arteriosus.
Normal in foals for the first 72 hours of life
– Shunt from pulmonary artery to aorta in utero
– Washing machine murmur, turbulence
in utero no lungs are needed, bypass during that is the shunt
but as soon as the baby is born, starts to breath, pda should shut down
Atrial Septal Defect and Ventricular Septal Defect.
– Causes de-oxygenated blood to be pumped to body
– Murmur
– Exercise intolerance
wall between left and right heart sides, can have defect, high pressure blood squirts into the low blood pressure side, oxygenated blood doesn’t get around as much
Valvular Insufficiency
– All four can be effected (usually not at once)
– Murmur
– Ruptured Chordae Tendineae
• Leads to valvular insufficiency: a heart condition where valves fail to close completely, causing blood to flow backward, decreasing cardiac efficiency
Endocarditis
Endocarditis is an infection of the heart's inner lining, chambers, or valves, most commonly caused by bacteria that enter the bloodstream and attach to damaged heart tissue
Atrial Fibrillation or afib
– Most common arrhythmia
– Exercise intolerance
– Irregularly- irregular, everything discharge when they want, not good
– Can treat with Quinidine
standard bred racehorses, whoosh bum sound
Congestive Heart Failure
Congestive Heart Failure
– Dilated cardiomyopathy: a serious heart condition where the heart's main pumping chamber (left ventricle) enlarges and weakens, making it harder to pump blood, which often leads to heart failure
– Seen with COPD: Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease causing airflow obstruction, with symptoms including shortness of breath, chronic cough, and mucus production
a chronic condition where the heart cannot pump enough blood to meet the body's needs, causing fluid to build up in the lungs and body
blood composition
plasma 55%, white blood cells and platelets <1%, red blood cells 45%
Blood
8% of body weight.
• Adult horse has aprox. 10 gallons of blood
• Transports oxygen and carbon dioxide
• Transports nutrients from GI
• Transports waste to kidneys
• Transports hormones from glands to target
• Aids in thermoregulation
• Key component of Immune System
• Clotting Cascade
red blood cells
No nuclei
• Hemoglobin in conjunction with iron carries oxygen
from lungs to tissues and carbon dioxide from tissues
to be expelled in lungs
• Produced in bone marrow
• Circulate 3 – 4 months then removed
• Large reserve in spleen, horse can contract spleen
when increased oxygen carrying capacity is needed, can squeeze and dump out RBCs, usually for escape, higher and more common in wild horses
baby horse is colic, laying down like a dog
nuconium compaction, use enema to treat it, soapy water, nuconium from fluids of baby getting embryonic fluids which are protein, eating it and feces
blood loss
Reproductive tract
– Breeding
– Post delivery
– Umbilical stump
broad ligament can rupture and bleed and mother horse can bleed out
proud flesh
lower wounds, excessive granulation, bulging over the skin, can cut it back and pressure wrap it, or burn it with copper sulfate to burn it back, caustic powder
lacerations
foreheads bleed a lot, but with blood flow there is healing
legs do not have great blood flow
distal limbs should be wrapped up
old wounds should be let to drain
Lacerations on distal limbs should be wrapped.
• If first bandage becomes soaked.
• Apply second bandage over first.
• Only remove bandages when primary repair is to
occur
How does clotting work?
muscles will spasm and cause clotting, but humans can then give pressure, there is a cellulose based clotting agents for soldiers
laceration treatments
betadine: stains you brown, less cytoxins used in hospitals
nolvasan: stains you blue, usually surgical
lidocaine for pain does also dilate the blood vessels so will bleed
old wounds can be tacted together
what is epistaxis?
nosebleed, lung rupture, or vet hit something and bleed
Exertion
– Exercise-induced pulmonary hemorrhage
• Trauma
– NGT
• Sinuses
– Ethmoid hematoma
dehydration
brain and heart have priority, sucks all fluid for that
Mucus Membranes dry up as dehydration progresses.
• GI sounds decrease as dehydration progresses, constipation or compaction, leading to gasses building, intestinal stretches, horses get anxious and feel painful, flight or fight mode, cecum fills out, sounds like a drum, skin stretched, constant gas production and horse balloon up
• Skin Tenting, check the eyelids, pinch on eyelids, see if stays, very subjective
Protein calculation
use a refractometer: measure total protein concentration in blood serum or plasma.
anemia
lack of RBC
–Decreased production: stop making them
– Loss
– Increased destruction, something is killing them
ex: tick borne illness, parasite, causes body to attack RBC
red maple trees, if branch falls off and a horse eats rotten leaves, horses can get renal failure, red blood cells clogging the kidneys
black walnuts, shavings can also cause failure
PVC determination
Packed Cell Volume (PCV) determination, or hematocrit, measures the percentage of red blood cells (RBCs) in a blood sample, typically through centrifugal separation
put the blood sample in a thin plastic tube with a stopper
RBC and plasma will separate after spinning, you measure the percentages based on how high the RBC level is in the thin tube
- Dehydration causes pcv to increase
- Anemia causes pcv to decrease
Where to draw blood from a horse?
jugular, if the horse is moving around a lot, you have to aim the needle downward to poke in
carotid artery is right on top of the jugular the further up the neck you go, the artery and vein separate and that gap gets bigger
What does the carotid artery do?
It gives blood to the brain, if injured, horses can backflip and then just lie on back having seizures, can only wait it out, they may die or get better
Where is the jugular vein?
it stands above the trachea, if you squeeze the neck muscles, it will fill up
Why blood tests?
check for drugs, but also, if a horse crosses state lines, equine infectious anemia exists, Dr. Cogins came up with test for this
"swamp fever," is an incurable, often fatal, viral disease of equids (horses, mules, donkeys) characterized by fever, severe anemia, and swelling
via blood-sucking insects or contaminated equipment, infected horses become lifelong carriers, requiring permanent isolation or euthanasia
What is the gutteral pouch?
Guttural pouches in horses are paired, air-filled sacs (outpouchings of the Eustachian tubes) located in the throatlatch region
used for thermo regulation
there is also a vessel inside to warm the air as it is breathed in
prone to mycosis (fungal plaques), empyema (pus), or tympany (air entrapment)
How do the legs thermoregulate?
Arterial blood is cooled by exchanging its heat to the returning venous blood in the legs
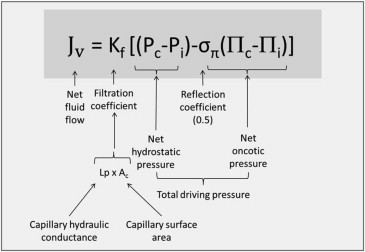
What is the starling equation?
What is interstitial pressure?
Interstitial pressure (or Interstitial Fluid Hydrostatic Pressure, IFHP) is the pressure within the fluid-filled spaces between cells (interstitial space) that influences fluid movement between these tissues and blood capillaries, typically acting as an opposing force to fluid exiting capillaries
What is osmotic pressure?
Osmotic pressure in blood is the force exerted by solutes (electrolytes, proteins) that draws water into the bloodstream, maintaining fluid balance between blood vessels and surrounding tissues
Plasma albumin
is the most abundant protein in human blood plasma, synthesized by the liver, playing critical roles in maintaining oncotic pressure (keeping fluid within blood vessels) and transporting hormones, drugs, and fatty acids. Normal levels (3.5–5.0 g/dL) indicate healthy liver/kidney function, while low levels (hypoalbuminemia) suggest disease, malnutrition, or inflammation.
low levels cause edema
pull water into bloodstream
Plasma globulins
Plasma globulins are a group of essential proteins in blood plasma—categorized as alpha, beta, and gamma—that play critical roles in immune defense, blood clotting, and the transport of nutrients, hormones, and lipids. Produced largely in the liver (alpha/beta) and by immune cells (gamma), they maintain osmotic pressure and fight infections.
Plasma electrolytes
Plasma electrolytes are essential minerals (like sodium, potassium, chloride, calcium, magnesium) dissolved in blood plasma that carry electrical charges, crucial for fluid balance, nerve signals, muscle function, and pH regulation, with imbalances indicating various health conditions. Clinically, tests measure levels of sodium, potassium, chloride, and bicarbonate, often alongside urea and creatinine, to assess hydration and organ function
plasma clotting factors
The clotting factors are Factor I (fibrinogen), Factor II (prothrombin), Factor III (tissue thromboplastin or tissue factor), Factor IV (ionized calcium), Factor V (labile factor or proaccelerin), Factor VII (stable factor or proconvertin), and Factor VIII (antihemophilic factor).
White Blood Cells
• Neutrophil: acting as the body's first responders to infections, especially bacterial and fungal, by engulfing germs and healing wounds
• Lymphocytes: Lymphocytes are crucial white blood cells—primarily T cells, B cells, and natural killer cells—that defend the body against infections, viruses, and tumors
• Monocyte: Monocytes are a type of white blood cell and key component of the innate immune system, comprising 2–10% of total leukocytes in human blood. They function by migrating into tissues to become macrophages or dendritic cells, aiding in pathogen defense, inflammation regulation, and tissue repair, low means bone marrow issues
• Basophil: Basophils are a type of white blood cell (leukocyte) that make up less than 1% of circulating white blood cells (normal range: ~0–300 cells/µL, or 0-1% of total WBC count). They play a crucial role in allergic reactions, inflammatory responses, and defense against parasites by releasing histamine, heparin, and other enzymes.
• Eosinophil: Eosinophils are a type of white blood cell crucial for fighting parasites and managing allergic reactions, killing cells, inflammatory responses
– Circulate, respond to chemotactic agents
– Diapedesis: or leukocyte extravasation, is the crucial process where white blood cells (neutrophils, monocytes, lymphocytes) pass through intact capillary walls into surrounding tissues to combat infection or inflammation. It is the final, active step of emigration, occurring after leukocyte adhesion and rolling, often driven by cytokines in postcapillary venules
What is blood doping?
Blood doping is a prohibited, illicit practice used by athletes to artificially increase their red blood cell count, enhancing oxygen delivery to muscles to improve endurance and performance
It typically involves blood transfusions (using one’s own or a donor’s blood) or the use of drugs like Erythropoietin (EPO) to stimulate RBC production. (synthetic oxygen carriers)
blood doping is dangerous and banned by the World Anti-Doping Agency (WADA). It significantly increases blood viscosity (thickness), which can lead to:
Strokes, heart attacks, and blood clots.
Infections from unsafe transfusion practices.
Increased pressure on the heart and lungs.
What is a milkshake for horses?
A "milkshake" is a performance-enhancing mixture given to racehorses that primarily contains sodium bicarbonate (baking soda), along with water, sugar, and electrolytes (salts). This illegal practice, known as "bicarbonate loading" or "milkshaking," is designed to counteract the buildup of lactic acid during intense exercise, so they do not feel the burn
tube into the stomach, this is illegal
but high dose of sodium bicarbonate acts as a buffer, raising the pH of the blood and extracellular fluid. This higher alkalinity is theorized to draw the excess hydrogen ions (from lactic acid) out of the muscle cells and into the bloodstream, where they are neutralized.
can cause death hours later, injury to nasal passages and throat, also cause accidental death and pneumonia from insertion into trachea instead of esophagus
Banamine testing
Banamine (flunixin meglumine) testing in horses is used to detect non-steroidal anti-inflammatory drug (NSAID) levels in blood or urine, typically to ensure compliance with competition rules.
How can you change protein levels?
you use IV plasma
hypertonic saline, pull water out of cells and tissues all of the vessels, reduces edema
Epsom salt (magnesium sulfate) acts as a strong saline laxative to clear the bowels for a colonoscopy, sometimes used as an adjunct to or component of prep kits. It works by pulling water into the intestine to flush out waste.