Music Exam 1
1/338
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
339 Terms
Describe bone mineral density
How much bone is in the matrix, diagnostic tool for osteoporosis and osteopenia. Biggest predictor of a fracture.
How is bone density regulated?
Osteoblasts build up bone using calcium in the blood, osteoclasts resorb bone which releases calcium into the blood
What hormones affect calcium homeostasis?
Parathyroid hormone (PTH) increases blood calcium levels through increased bone resorption. Calcitonin inhibits osteoclast activity, decreasing bone resorption and decreasing blood calcium levels. Vitamin D increases calcium absorption in the intestines.
How is bone loss monitored?
BMD scans, report as either a t-score (standard deviation compared to a healthy 30 year old) or a z-score (standard deviation compared to the same age and gender)
Define osteoporosis
Systemic disease characterized by low bone mass and microarchitecture deterioration with consequent increase in bone fragility and susceptibility to fracture
Osteoporosis diagnosis
T-score <2.5, severe bone mineral density loss
Osteoporosis risk factors
increased age
caucasian or asian
thin body frame
early menopause (<45)
late menarche (>16)
family history
diet lacking vitamin D and calcium
sedentary lifestyle
type 1 diabetes
cigarette smoking
heavy alcohol use
Secondary causes of osteoporosis
corticosteroid use/cushing’s syndrome
renal failure
hyperparathyroidism
hyperthyroidism
paget’s disease
GI dysfunction
rheumatoid arthritis
eating disorders
vitamin D/calcium deficiency
hypogonadism
Remember the chicken
Chickens on a calcium free diet still produced hard shelled eggs, but their skeletons were extremely weak. Shows the skeleton isn’t static and is the largest source of calcium in the body.
How is bone mineral density measured?
Dual energy X-ray absorptiometry (DEXA) scan, expressed as mineralized tissue in an area scanned
Why is measuring BMD important?
single most important predictor of future fractures
How are BMD and risk of future fractures related?
Inverse relationship (decrease in BMD, increase in risk of future fracture)
What is a t-score and what does it represent?
Bone mineral density compared to a “young healthy adult” (30 year old), reported as the difference in standard deviation from a mean
Normal t-score
(-)1 - +1
Low bone mass t-score (osteopenia)
1-2.5 STD below mean
osteoporosis t-score
More than 2.5 std below mean
severe osteoporosis defintion
t-score greater than 2.5 std below the mean and 3+ osteoporotic fractures
Normal z-score
0-2 standard deviations below average
Low z-score
Greater than 2 stds below mean
What is the most reliable and best predictor of future fractures
Hip BMD
Weaknesses of BMD
static, no insight into bone turnover
Organ systems that regulate blood calcium levels
GI, skeletal, renal
Which system is the major pathway of blood calcium regulation?
skeletal system
osteocytes
mature bone cells in the matrix, compose a vast majority of bone cells, many functions
osteoblasts (OBs)
bone forming cells that facilitate mineralization of calcium, phosphate, and hydroxyapatite. promotes bone matrix
osteoclasts (OCs)
bone degrading cells, promote resorption of bone, promote bone remodeling
In what ways does the skeleton adapt?
size, shape, integrity to promote mineral homeostasis
salubrious (healthy) bone remodeling
growth, repair of damage, response to mechanical stress
What does calcitonin do?
inhibit OC activity, inhibits bone resorption, promotes hypocalcemia
Vitamin D’s role
increase calcium absorption in intestines
What does PTH do?
increase blood calcium levels by stimulating calcium resorption from bones, calcium reabsorption in the kidneys, and vitamin D synthesis
Age of peak bone mass
30
Why do we care about preventing fractures?
people that have severe fractures (hip, vertebrae) have a greater chance of mortality and only 50% of hip fracture pts regain the same level of independence
Why does renal failure cause osteoporosis?
failure to activate vitamin D
Why is hyperparathyroidism a cause of osteoporosis?
increases PTH levels, increasing OC activity, increasing bone resorption
What is the #1 cause of osteopenia/osteoporosis?
glucocorticoid use
Drugs that are linked to osteopenia/osteoporosis
glucocorticoids, anticonvulsants, lithium, chronic use of phosphate-binding agents, methotrexate, loop diuretics, excess thyroid supplementation
ways to prevent bone loss
adequate calcium and vitamin D intake, smoking cessation, limiting alcohol intake, weight bearing exercise, avoid falling
Goal of osteoporosis treatment
prevent or slow existing bone loss and build up existing bone, reduce the risk of fracture
Antiresorptive agents
bisphosphonates, calcitonin, denosumab, estrogen, SERMs, testosterone
Anabolic agents
teriparatide, abaloparatide, romosozumab
General daily adult dose of calcium
1 gram per day
Daily dose of calcium for men >70 and women >50
1.2 grams per day
Best salt form of calcium for absorption
phosphate
Calcium salt form that doesn’t require acid
citrate, lactate
What must be given to patients when they’re being treated for osteoporosis?
calcium and vitamin D supplements
Bisphosphonates MOA
bind to sites of active resorption on bone, inhibit osteoclast activity, inhibit further bone resorption
Frequency of alendronate
weekly
risedronate dosing frequency
weekly or monthly
ibandronate dosing frequency
monthly
zoledronate dosing frequency
yearly
Instructions for taking bisphosphonates
take on an empty stomach, full glass of water, take 30 min prior to food, do not lay down after taking
duration of bisphosphonate use
10 years for high risk patients, 5 years on then 5 years off repeating if needed
Calcitonin MOA
inhibit OCs to decrease bone resorption
Why do we use salmon calcitonin?
longer acting and more potent
Is calcitonin generally a first line agent?
no
Estrogen supplement MOA
directly inhibit OCs, stimulate OBs, antagonize PTH
SERM activity sites
estrogen agonist at bone, estrogen antagonist everywhere else
Major adverse effects of estrogen and SERMs
blood clots, uterine cancer, breast cancer
Denosumab MOA
mAB that prevents the activation of OCs, increasing bone mass and strength
Denosumab indications
postmenopausal women with OP at high risk for fractures, patients who failed other treatments, chemotherapy-induced bone loss
When do we use anabolic therapy?
When patients are at the highest risk for OP fractures and have failed other therapies
teriparatide MOA
paradoxical, binds PTH1R receptor and stimulates OB activity when given in a cyclic and pulsed manner
Duration of teriparatide therapy
2 years, then generally follow up with an anti-resorptive med
abaloparatide compared to teriparatide
same for everything except for the cost
Who is most commonly diagnosed with osteoporosis?
post menopausal women
What is osteoporosis?
Bone disorder with decreased bone density, impaired bone structure, and bone strength
What does osteoporotic bone look like?
Spongy
Non-modifiable risk factors
female, age >65, asian or white ethnicity, dementia, family history, poor health or fragility, early menopause
potentially modifiable risk factors
alcohol use, tobacco use, caffeine intake, calcium intake, exercise, body weight, medication use
medications that increase fracture risk
anticoagulants, anticonvulsants, aromatase inhibitors, chemotherapy drugs, glucocorticoids, GnRH agonists, immunosuppressants, loop diuretics, progestins, PPIs, SSRis, SGLT-2 inhibitors, TZDs, thyroid products
osteoporotic risk factors MnEmOnIc
lOw calcium intake
Seizure meds
Thin build
Ethanol intake
hypOgonadism
Previous fracture
thyrOid excess
Race asian or white
Steroid use
Inactivity
Smoking
When is the fracture risk assessment (FRAX) used
all post menopausal women, men >50 years old
Who should have BMD testing?
women >65, women 50-64 if FRAX >9.3%, men >70, post menopausal women and men >50 with risk factors, adults with a fracture after age 50, adults taking meds known to increase bone loss or fracture risk
When is vertebral imaging indicated?
women >70, men >80, women >65 if t-score <1.0, loss of height >4cm, glucocorticoid therapy equivalent to >5mg of prednisone per day for >3 months
Gold Standard test for BMD
DEXA scan
FRAX score
Predicts 10 year probability of hip fracture and major osteoporotic fracture
Bone turnover markers (BTM)
Serum tests that reflect either bone resorption or formation, not for diagnosis but assesses skeletal activity and shows if therapy is responsive
osteoporosis diagnosis
one of the following:
t-score <-2.5
low-trauma spine or hip fracture regardless of BMD
osteopenia with fragility fracture
osteopenia and high FRAX probability
Non-pharm osteoporosis treatment
adequate calcium and vitamin D intake, exercise (weight-bearing, resistance, balance), avoid tobacco, limit alcohol intake, reduce fall risk
ways to prevent falls
anchor rugs, minimize clutter, remove loose wires, nonskid mats, handrails, lights, sturdy and low heeled shoes
How much calcium is in a product based on the food label?
Label lists % of daily value of 1000 mg
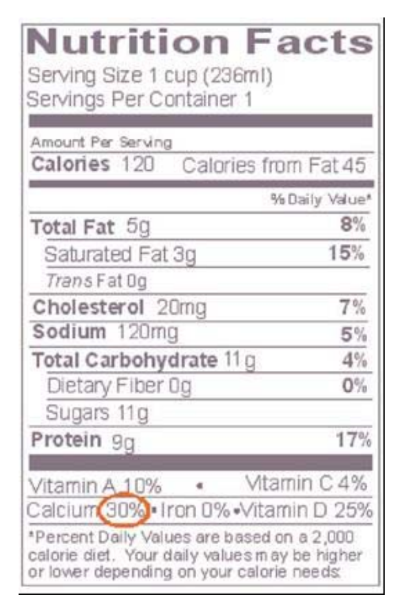
How much calcium is in this?
300 mg (1000mg*0.30)
Is diet generally adequate for calcium intake?
No, need 1000-1200 mg of calcium per day
calcium carbonate
40% elemental calcium
needs acid
take with meals
side effects: constipation and kidney stones
calcium citrate
21% elemental calcium
doesn’t need acid for absorption
don’t need to take with meals
side effects: constipation, kidney stones
normal daily dose of vitamin D
20-50 ng/mL
When is treatment strongly recommended for osteoporosis?
osteopenia with a history of fragility fracture of the hip or spine
t-score < -2.5 in the spine, femoral neck, total hip, of 1/3 radius of the hip
t-score between -1.0 and -2.5 if the FRAX score is >20% for major osteoporotic fracture of >3% for hip fracture
First line OP therapy for high risk patients with no prior fractures
alendronate, denosumab, risedronate, zoledronate
First line OP therapy for very high risk patients and those who have prior fractures
abaloparatide, denosumab, romosozumab, teriparatide, zoledronate
Bisphosphonate examples
alendronate, ibandronate, risedronate, zoledronic acid
What is first line therapy for treatment and prevention of OP?
bisphosphonates
Bisphosphonate MOA
increases bone density by inhibiting OC activity and bone resorption, reduces vertebral fracture risk
Which bisphosphonates do we avoid using in CrCl <35?
alendronate and zoledronic acid
Which bisphosphonates do we avoid using in CrCl <30?
all (alendronate, zoledronic acid, ibandronate, risedronate)
Contraindications for bisphosphonates
inability to sit upright/stand for at least 30 min (60 min with ibandronate)
esophageal abnormalities
difficulty swallowing
hypocalcemia (can correct before use)
Bisphosphonates warnings
osteonecrosis of jaw, atypical femur fractures, esophagitis, renal impairment
Bisphosphonates counseling points
administer on an empty stomach
take with 6-8 oz of water
do not eat for at least 30 min
remain upright for 30 min (60 min for ibandronate)
Raloxifene MOA
SERM, estrogen agonist at bone, estrogen antagonist at breast and uterus
Raloxifene dose
60 mg PO qD